Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Dupuytren’s contracture is a fibroproliferative disorder that has a US prevalence rate of approximately 7%, with those reporting a diagnosis or treatment having a mean age of 59 years. Progressive fibrosis of the palm leading to flexion, hypertrophy, contracture of the palmar, and digital fascia are key symptoms of Dupuytren’s contracture.
Fibroblast dysregulation, the xanthine oxidase pathway, oxidase stress, and proinflammatory protein mediators (cytokines) play a crucial role in the pathogenesis and prognosis of Dupuytren’s contracture.
Depression Can Aggravate Symptoms Associated With Dupuytren’s Contracture
To the Editor: Dupuytren’s contracture is a fibroproliferative disorder that has a US prevalence rate of approximately 7%, with those reporting a diagnosis or treatment having a mean age of 59 years.1 Progressive fibrosis of the palm leading to flexion, hypertrophy, contracture of the palmar, and digital fascia are key symptoms of Dupuytren’s contracture.2
Fibroblast dysregulation, the xanthine oxidase pathway, oxidase stress, and proinflammatory protein mediators (cytokines) play a crucial role in the pathogenesis and prognosis of Dupuytren’s contracture.2 Evidence suggests that fibroblast and proinflammatory protein mediator dysregulation may be present in patients with major depression.3 Even though Dupuytren’s contracture is associated with many comorbid conditions, literature is sparse with regard to the co-occurrence of Dupuytren’s contracture and major depression. This case report shows possible associations of depression with Dupuytren’s contracture.
Case report. Mr A, a 50-year-old white man with a medical history of Dupuytren’s contracture, past alcoholism, hypothyroidism, Peyronie’s disease, and depression and a smoking history of a half pack per day for over 30 years, presented to a university clinic in February 2015 with exacerbation of his depression and bilateral Dupuytren’s contracture. Mr A complained of pain, which he rated as 7/10, making it difficult for him to use his hands, and he denied any history of trauma. Mr A worked in construction for more than 25 years, which required repetitive use of both hands. He became unable to work and went on disability in 2013 due to severe Dupuytren’s contracture in both hands.
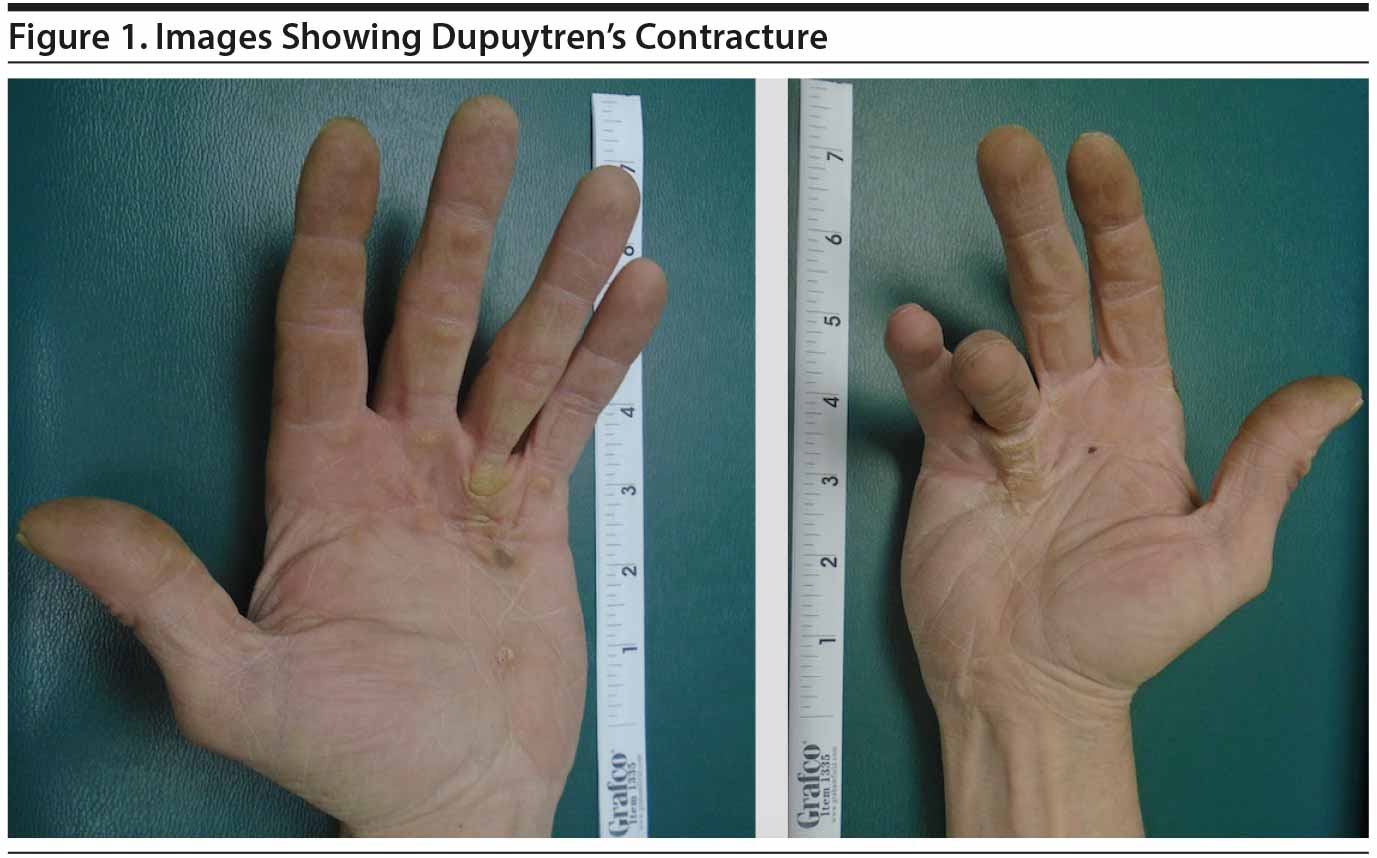
Mr A complained of worsening depression coinciding with Dupuytren’s contracture together with loss of appetite, feeling hopeless, insomnia, loss of interest, and low energy of more than 4 weeks’ duration, with no suicidal ideation. Mr A had no other significant mental health issue, and he scored 21 on the Hamilton Depression Rating Scale.4 Mr A also stated that he noticed a cyclical pattern of his depression aggravating his Dupuytren’s contracture symptoms. He stated that once his depression started or relapsed, the Dupuytren’s contracture pain became more intense. He also noticed a significant reduction in pain whenever his depressive symptoms improved. At examination, he had a blunt affect and contracture in both palms, with significant bowstringing in his right hand making it difficult to place the hand flat on a table (Figure 1). Complete blood count and basic metabolic panel tests were normal, although his thyroid-stimulating hormone level was elevated.
A diagnosis of recurrent major depressive disorder was made (DSM-5 criteria), and he was started on venlafaxine extended release 150 mg/d, along with pain management with morphine controlled release 30 mg every 12 hours. Mr A noted a significant improvement of his symptoms while on this regimen and after 3 months was scheduled for surgical exploration and repair of the hand, which was unsuccessful.
Depression has been linked to dysregulation of the fibroblast, possibly via the mechanism of oxidative stress.3 Worsening of Mr A’s depression coinciding with exacerbation of Dupuytren’s contracture suggests that symptoms of both conditions might be due to similar pathways. Antidepressant doses of venlafaxine have been shown to modulate oxidative stress,5 which might have been the reason for Mr A’s improvement. Venlafaxine has been shown to inhibit glucocorticoid-induced gene transcription in both mouse fibroblasts.6 Mr A’s current history of smoking, previous alcohol use, and repetitive use of his hands might have contributed to the Dupuytren’s contracture since they are modifiable factors; however, he was able to correlate the cyclic worsening of his Dupuytren’s contracture pain with relapse of his depression.
This case highlights the fact that Dupuytren’s contracture with comorbidities such as severe depression could alter the prognosis via complex interactions affecting fibroblast dysregulation and oxidase stress. Further studies are required.
References
1. Dibenedetti DB, Nguyen D, Zografos L, et al. Prevalence, incidence, and treatments of Dupuytren’s disease in the United States: results from a population-based study. Hand (NY). 2011;6(2):149-158. PubMed doi:10.1007/s11552-010-9306-4
2. Hart MG, Hooper G. Clinical associations of Dupuytren’s disease. Postgrad Med J. 2005;81(957):425-428. PubMed doi:10.1136/pgmj.2004.027425
3. Evans SJ, Choudary PV, Neal CR, et al. Dysregulation of the fibroblast growth factor system in major depression. Proc Natl Acad Sci U S A. 2004;101(43):15506-15511. PubMed doi:10.1073/pnas.0406788101
4. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56-62. PubMed doi:10.1136/jnnp.23.1.56 >
5. Abdel-Wahab BA, Salama RH. Venlafaxine protects against stress-induced oxidative DNA damage in hippocampus during antidepressant testing in mice. Pharmacol Biochem Behav. 2011;100(1):59-65. PubMed doi:10.1016/j.pbb.2011.07.015
6. Augustyn M, Otczyk M, Budziszewska B, et al. Effects of some new antidepressant drugs on the glucocorticoid receptor-mediated gene transcription in fibroblast cells. Pharmacol Rep. 2005;57(6):766-773. PubMed
Author affiliations: Department of Psychiatry, Central Michigan University College of Medicine, Saginaw (Dr Osuagwu), Department of Family Medicine, Central Michigan University College of Medicine, Saginaw (Drs Noveloso, Hashmi, and Reddy), and Ross University School of Medicine, Dominica, West Indies (Mr Amalraj).
Potential conflicts of interest: None reported.
Funding/support: None reported.
Published online: December 3, 2015.
Prim Care Companion CNS Disord 2015;17(6):doi:10.4088/PCC.15l01832
© Copyright 2015 Physicians Postgraduate Press, Inc.
Enjoy this premium PDF as part of your membership benefits!