Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Individuals who sleep for 6 hours or less and have no daytime impairment are considered to be short-sleepers. This variation in sleep duration is relatively rare and thought to occur in 3.6% of men and 4.3% of women. While short sleepers themselves may have no complaints, their caregivers might be concerned about the short duration of sleep and/or express frustration about the impact that this is having on their own ability to obtain adequate rest.
Short Sleep in Patients With Chronic Paranoid Schizophrenia
To the Editor: Individuals who sleep for 6 hours or less and have no daytime impairment are considered to be short-sleepers.1 This variation in sleep duration is relatively rare and thought to occur in 3.6% of men and 4.3% of women.2 While short sleepers themselves may have no complaints, their caregivers might be concerned about the short duration of sleep and/or express frustration about the impact that this is having on their own ability to obtain adequate rest. There is little evidence supporting the use of hypnotics in this patient population.
Previous actigraphy studies of community dwelling schizophrenics have shown total sleep times of over 9 to 10 hours.3,4 These studies did not report any patients who were short sleepers. Here, we report 2 patients who presented for a sleep consultation due to caregiver concerns about their long-standing pattern of short sleep times.
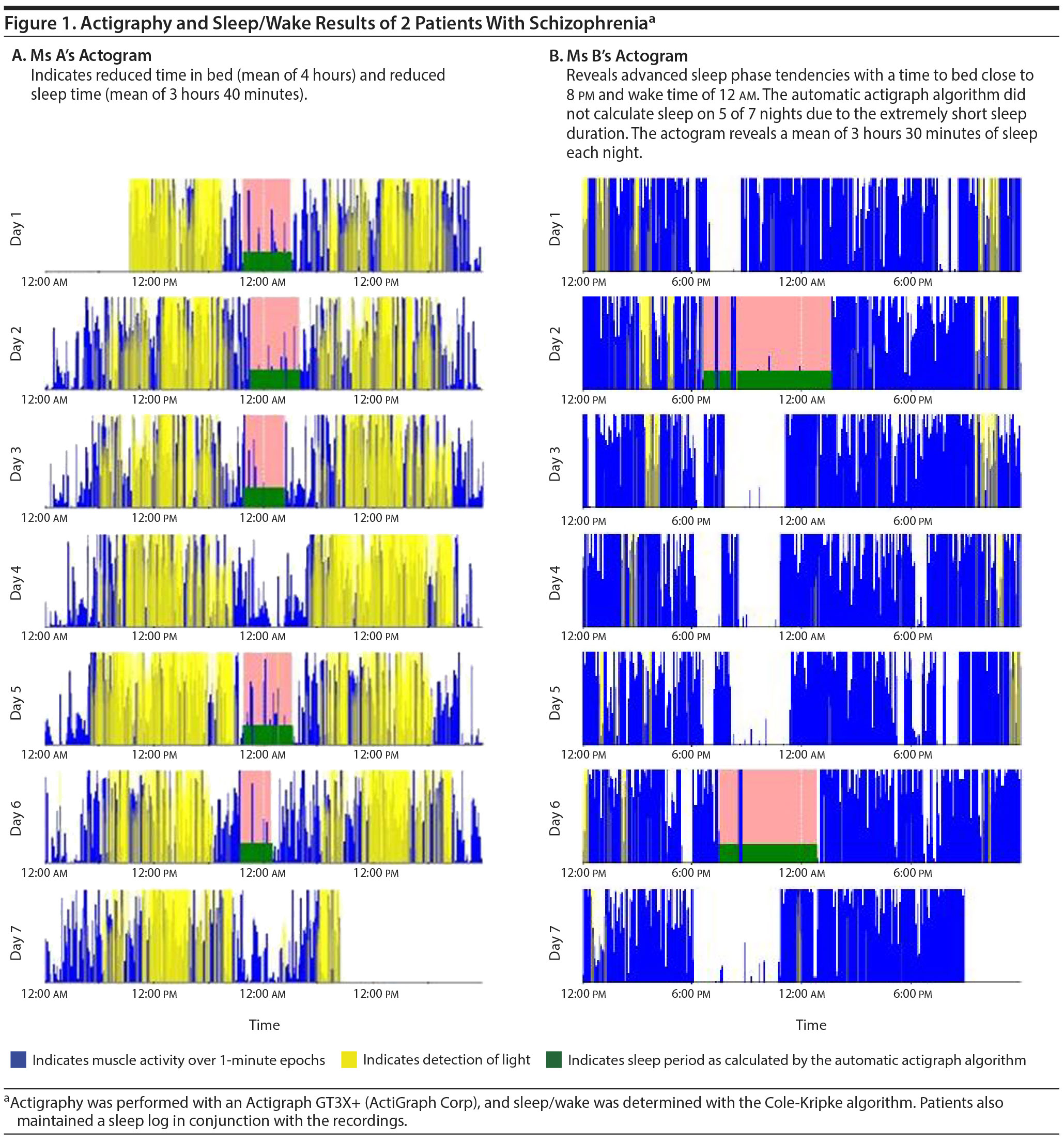
Case 1. Ms A, a 71-year-old woman with a history of chronic paranoid schizophrenia (DSM-5) was taking aripiprazole 10 mg, venlafaxine 150 mg, and a recent addition of trazodone 100 mg and presented due to caregiver concerns about the quantity of sleep she was obtaining. She had had no active psychotic symptoms for a few years. Ms A had no sleep complaints and described going to bed at 9:30 pm, falling asleep quickly and sleeping until midnight. She would wake for unclear reasons and either remain up or sometimes (< 50% of nights) sleep again from 2 am-5 am. Trazodone was started by her primary care provider for her short sleep duration. She did endorse no daytime consequences or impairments secondary to her short sleep duration and did not nap during the day. Seven-day wrist actigraphy revealed a mean of 4 hours in bed and 3 hours 40 minutes of sleep with no daytime naps recorded (Figure 1A).
Case 2. Ms B, a 55-year-old woman with a DSM-5 diagnosis of chronic paranoid schizophrenia with no current psychotic symptoms was brought for an evaluation by her mother who was concerned about her long-standing sleep pattern. Ms B was taking venlafaxine 75 mg, asenapine 5 mg twice daily, and lorazepam 0.5 mg 3 times a day. She described a pattern of going to bed at 8 pm, falling asleep quickly, and awakening spontaneously at midnight. She did not describe any daytime consequences or impairments secondary to her short sleep duration and did not nap during the day. Seven-day wrist actigraphy revealed advanced sleep-wake phase tendencies with a mean sleep duration of 3 hours and 30 minutes with a sleep efficiency of 95% (Figure 1B). No daytime naps were recorded.
In both of our patients, the sleep duration was significantly reduced, but as with all short sleepers, neither patient had any sleep complaints per se and presented only because of caregiver concerns. It is possible that in addition to short sleep, our cases had advanced sleep-wake phase tendencies, based on the reported sleep-wake cycle. Also, automatic scoring of actigraphs may under or over estimate total sleep time. The use of a concurrent sleep diary with manual entry of data by the patient is useful to obtain a better idea of the overall time spent in bed. In Ms A, the use of trazodone resulted in no increased sleep duration. After discussion with their sleep-care providers, neither patient chose to pursue further treatment.
While polysomnographic studies of patients with schizophrenia have shown a decrease in total sleep time and sleep efficiency along with an increase in sleep-onset latency, the reduced total sleep time in these studies did meet criteria for short sleep.5 A previous study of 20 outpatients with schizophrenia reported mean sleep times of 8.22 hours on 6-week actigraphy.4 This amount was significantly longer than age-, sex-, and chronotype-matched controls (P = .0001). Another study examining 28 older patients with schizophrenia (mean age = 58 years) reported a mean of 11 hours in bed at night with sleep efficiencies of 68% on 3-day actigraphy.3 In addition, this study reported that, on average, patients obtained an additional hour-long nap.
Further research on sleep in patients with schizophrenia would need to explore the possibility of whether this rare sleep-duration phenotype occurs frequently and potentially influences adverse outcomes. Clinicians treating patients with schizophrenia should also be alert to the possibility of short sleep in addition to other sleep disorders that are commonly associated with this diagnosis.
References
1. International Classification of Sleep Disorders, Third Edition (ICSD-3), 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014.
2. Kripke DF, Garfinkel L, Wingard DL, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131-136. PubMed doi:10.1001/archpsyc.59.2.131
3. Martin J, Jeste DV, Caliguiri MP, et al. Actigraphic estimates of circadian rhythms and sleep/wake in older schizophrenia patients. Schizophr Res. 2001;47(1):77-86. PubMed doi:10.1016/S0920-9964(00)00029-3
4. Wulff K, Dijk DJ, Middleton B, et al. Sleep and circadian rhythm disruption in schizophrenia. Br J Psychiatry. 2012;200(4):308-316. PubMed doi:10.1192/bjp.bp.111.096321
5. Chouinard S, Poulin J, Stip E, et al. Sleep in untreated patients with schizophrenia: a meta-analysis. Schizophr Bull. 2004;30(4):957-967. PubMed doi:10.1093/oxfordjournals.schbul.a007145
aDepartment of Psychiatry and Psychology, Mayo Clinic, Rochester, Minnesota
bCenter for Sleep Medicine, Mayo Clinic, Rochester, Minnesota
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: The patients provided verbal permission to publish their cases, and information has been completely de-identified to protect anonymity.
Published online: August 17, 2017.
Prim Care Companion CNS Disord 2017;19(4):17l02094
https://doi.org/10.4088/PCC.17l02094
© Copyright 2017 Physicians Postgraduate Press, Inc.
Enjoy this premium PDF as part of your membership benefits!