Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Hydrocephalus is one of the most common neurosurgical disorders observed in both adult and pediatric populations. On the basis of pathology, hydrocephalus is classified as either communicating (nonobstructive) or noncommunicating (obstructive) types. Etiology can be congenital or acquired.
Noncommunicating Hydrocephalus Presenting With Pseudoseizures: A Case Report
To the Editor: Hydrocephalus is one of the most common neurosurgical disorders observed in both adult and pediatric populations. On the basis of pathology, hydrocephalus is classified as either communicating (nonobstructive) or noncommunicating (obstructive) types. Etiology can be congenital or acquired. Another variant that does not fit into the above categories is normal pressure hydrocephalus.1
Case report. A 16-year-old boy in the 10th grade presented to a psychiatry outpatient department with episodes of sudden onset of mutism along with hyperventilation lasting for 10-15 minutes for the past month. The episodes were not associated with loss of consciousness, incontinence, tongue biting, or any abnormal jerky limb movements. During a detailed workup, the patient disclosed that he was particularly distressed about his upcoming school examinations. His mother also added that he had complaints of headache and declining academic performance for the past year. A general physical examination revealed a thin-built boy with stable vital signs. A mental status examination revealed ill-sustained eye-to-eye contact, anxious affect, intact judgment, and higher mental functions. There was no past or family history of any chronic psychiatric or medical disorder or substance abuse.
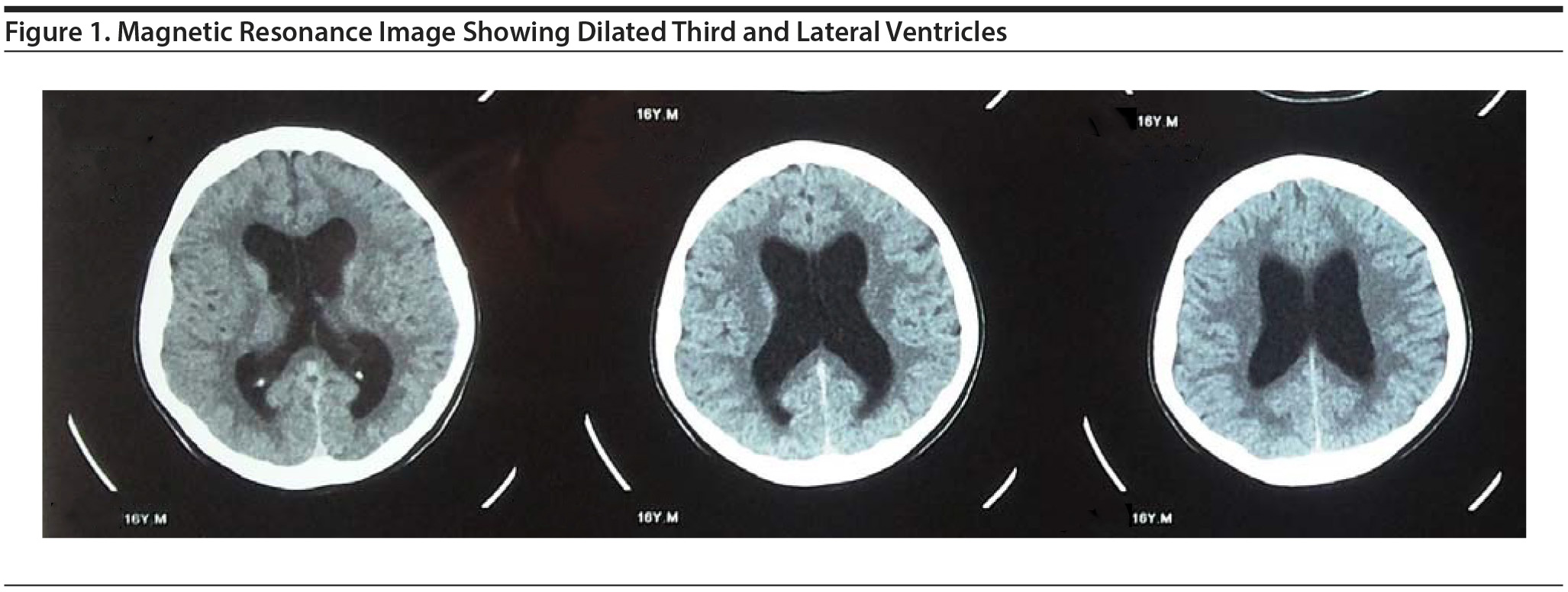
During his stay in the hospital, the patient had episodes of abnormal behavior varying in nature from mutism along with hyperventilation to sudden onset of screaming, fearfulness, and impaired consciousness. The episodes were dissociative in nature. An electroencephalograph showed a normal awake study. He was started on tablet etizolam 0.5 mg twice a day and supportive psychotherapy sessions, which led to resolution of the dissociative episodes. However, the patient complained of persistent headache. A funduscopic examination was normal. Radiologic imaging in the form of noncontrast head computed tomography revealed dilated lateral and third ventricles. Subsequently, brain magnetic resonance imaging confirmed the diagnosis of noncommunicating hydrocephalus with dilated bilateral lateral and third ventricles with normal fourth ventricle with no periventricular edema (Figure 1). Neurosurgical opinion was sought and conservative management in the form of tablet acetazolamide 250 mg twice a day was started. This regimen led to a reduction in the frequency and severity of his headaches. At follow-up 3 months later, the patient was back in school and adjusting well in his new class.
Patients mostly present with headache, nausea, vomiting, blurring of vision, diplopia, poor coordination, incontinence, and behavioral manifestations such as lethargy, drowsiness, irritability, cognitive decline, and personality changes. In the pediatric population, declining school performance with intermittent headache is often an important clue for diagnosis.2-4 Psychiatric manifestations are more commonly encountered in the normal pressure hydrocephalus variant.5 This is the first report of noncommunicating hydrocephalus presenting with pseudoseizures.
A high index of suspicion and thorough evaluation even in cases of pseudoseizure can help in early diagnosis and timely intervention.
References
1. Sheet HF. National Institute of Neurological Disorders and Stroke. NIH Publication No. 08385; May 2013. http://www.ninds.nih.gov/disorders/hydrocephalus/detail_hydrocephalus.htm. Updated 2015. Accessed April 13, 2015.
2. Ropper AH, Brown RH. Adam and Victor’s Principles of Neurology. 8th ed. New York, NY: McGraw-Hill; 2005.
3. Kirkpatrick M, Engleman H, Minns RA. Symptoms and signs of progressive hydrocephalus. Arch Dis Child. 1989;64(1):124-128. PubMed doi:10.1136/adc.64.1.124
4. Amorim Júnior RF, Dantas SEC, Mendonça RH, et al. Screening of epileptic seizures in children and adolescents with hydrocephalus and ventriculoperitoneal shunt. J Epilepsy Clin Neurophysiol Porto Alegre. 2009;15(3):106-109. doi:10.1590/S1676-26492009000300002
5. Kito Y, Kazui H, Kubo Y, et al. Neuropsychiatric symptoms in patients with idiopathic normal pressure hydrocephalus. Behav Neurol. 2009;21(3):165-174. PubMed doi:10.1155/2009/791491
aDepartment of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi, India.
Potential conflicts of interest: None reported.
Funding/support: None reported.
Published online: December 31, 2015.
Prim Care Companion CNS Disord 2015;17(6):doi:10.4088/PCC.15l01827
© Copyright 2015 Physicians Postgraduate Press, Inc.
Enjoy this premium PDF as part of your membership benefits!