Manic Episode Misdiagnosed in a Case of Temporal Lobe Epilepsy
The association of temporal lobe epilepsy (TLE) with behavioral problems, cognitive impairment, and personality changes has been widely reported.1-3 Previous literature reported sparing of executive function, a frontal lobe task, in TLE.4 However, emerging research suggests a connection between the temporal lobe and frontal lobe processes, elucidating executive dysfunction in TLE.5 We hereby report a case of TLE with frontotemporal involvement.
Case Report
Mr A, 28-year-old factory worker, was brought to the emergency department by a friend. He was observed to be overtalkative, overfamiliar, and euphoric with increased psychomotor activity. A tentative diagnosis of manic episode was made, injectable lorazepam 2 mg was given, and a reliable informant was called. Mr A’s mother reported that he had discontinued studies in the fourth grade and started working as a helper at a construction site. He lost this job at age 15 years due to overtalkativeness, stubbornness, seizures, and difficulty managing multiple tasks. He was difficult to interrupt during conversations, so the family stopped having him participate in social gatherings. The antenatal period was uneventful with normal developmental milestones. His mother recalled that he had his first seizure at 3 months of age, which was characterized by abnormal jerky movements of the left side of the body. He was treated with antiepileptics for 3 years for which exact records were unavailable. The patient remained seizure free from 3 months to 15 years of age when he developed generalized tonic-clonic movements associated with loss of consciousness with a frequency of 1 to 2 per day that lasted for 3 to 4 months. He was treated with phenytoin sodium 300 mg/day at a primary health center for 2 to 3 years and remained seizure free for 15 months before presenting to the emergency department, when he again started having generalized tonic-clonic movements every 2 months. There was no history of substance use, head injury, or encephalitis. The physical examination was unremarkable.
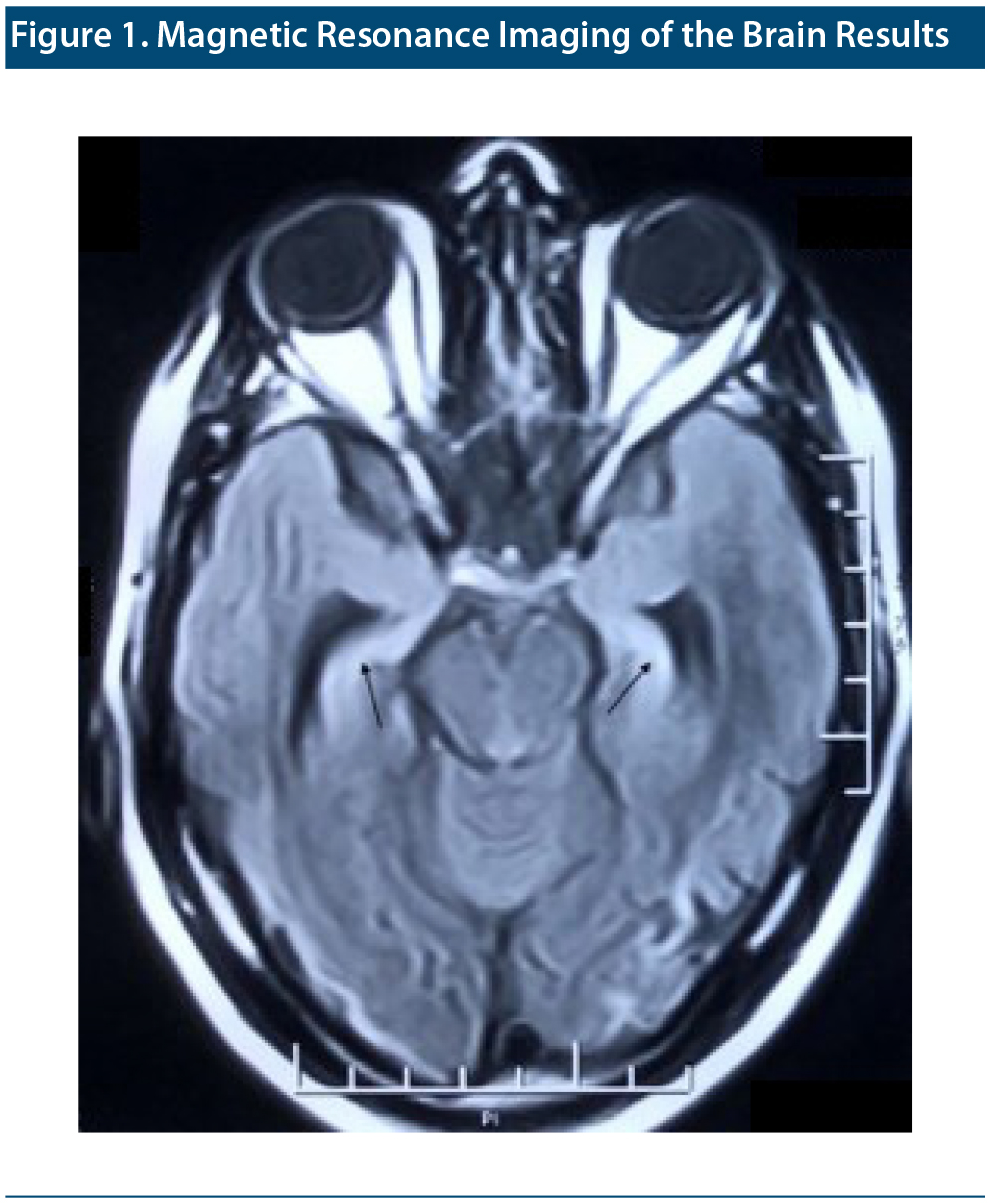
The mental state examination revealed increased psychomotor activity and speech productivity with overinclusive details, circumstantiality, and euphoric affect. He showed viscosity by sticking to his conversation, with difficulty in leaving the consultant’s room. Neuropsychological testing6 revealed impairment in attention on serial subtraction and digital repetition and in immediate recall and abstraction. Magnetic resonance imaging (MRI) of the brain showed increased signal intensity on T2/fluid-attenuated inversion recovery in bilateral medial temporal lobes with severe atrophy and dilatation of adjacent temporal horns (Figure 1). Electroencephalogram (EEG) showed intermittent spikes in the bilateral frontotemporal region. Complete blood count, liver function test, kidney function test, serum electrolytes, serum vitamin B12, serum vitamin D3, serum folate, and thyroid function test results were within normal limits. He was nonreactive for HIV, hepatitis B, and hepatitis C and the venereal disease research laboratory and urine drug toxicology screen results were negative. A provisional diagnosis of organic personality disorder (ICD-10 code F07.0) was made. A psychotherapeutic approach was planned for Mr A, and he received valproate 1 g for both seizure disorder and behavioral problems.
Discussion
This case highlights the features of interictal personality change. The mixed presentation of circumstantiality, viscosity, elation, disinhibition, inattention, and impaired abstraction in our patient has been supported by the overlap of frontal lobe involvement in temporal lobe epilepsy.5,7 At the initial presentation, he was misdiagnosed as having a manic episode. However, detailed history, serial mental status examinations, associated cognitive impairment, neuroimaging, EEG, and laboratory investigations helped in reaching the final diagnosis. Strub and Black’s 6 clinical utility for neuropsychological testing and teaching purposes has been demonstrated in several studies.8
The plausible explanation for the occurrence of repetitive seizures in a case of temporal lobe epilepsy may be attributed to mesial temporal sclerosis including the pathological involvement of the hippocampus.9 Previous research10,11 has found that recurrence of seizures after a silent period in a case of childhood epilepsy demonstrates further exacerbation of brain insult. Further, studies12 have concluded the importance of MRI of the head in diagnosing hippocampal sclerosis with hippocampal atrophy on T1-weighted images and enhanced hippocampal signal on T2-weighted images. Use of antiepileptics with psychotherapy has been the treatment of choice for chronic intractable seizure; however, patients may need surgery localized to the temporal lobe.13
Published online: December 31, 2020.
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
REFERENCES
1.Blumer D. Evidence supporting the temporal lobe epilepsy personality syndrome. Neurology. 1999;53(suppl 2):S9-S12. PubMed
2.Perrine K, Kiolbasa T. Cognitive deficits in epilepsy and contribution to psychopathology. Neurology. 1999;53(suppl 2):S39-S48. PubMed
3.Schwartz JM, Marsh L. The psychiatric perspectives of epilepsy. Psychosomatics. 2000;41(1):31-38. PubMed CrossRef
4.Squire LR, Stark CEL, Clark RE. The medial temporal lobe. Annu Rev Neurosci. 2004;27(1):279-306. PubMed CrossRef
5.Stretton J, Thompson PJ. Frontal lobe function in temporal lobe epilepsy. Epilepsy Res. 2012;98(1):1-13. PubMed CrossRef
6.Strub RL, Black W. The Mental Status Examination in Neurology. 2nd ed. Philadelphia, PA: F. A. Davis; 1985.
7.Bear DM, Fedio P. Quantitative analysis of interictal behavior in temporal lobe epilepsy. Arch Neurol. 1977;34(8):454-467. PubMed CrossRef
8.Simpson N, Black FW, Strub RL. Memory assessment using the Strub-Black Mental Status Examination and the Wechsler Memory Scale. J Clin Psychol. 1986;42(1):147-155. PubMed CrossRef
9.Galanopoulou AS, Vidaurre J, Moshé SL. Under what circumstances can seizures produce hippocampal injury: evidence for age-specific effects. Dev Neurosci. 2002;24(5):355-363. PubMed CrossRef
10.Liu Z, Mikati M, Holmes GL. Mesial temporal sclerosis: pathogenesis and significance. Pediatr Neurol. 1995;12(1):5-16. PubMed CrossRef
11.Koh S, Storey TW, Santos TC, et al. Early-life seizures in rats increase susceptibility to seizure-induced brain injury in adulthood. Neurology. 1999;53(5):915-921. PubMed CrossRef
12.Jackson GD, Berkovic SF, Duncan JS, et al. Optimizing the diagnosis of hippocampal sclerosis using MR imaging. AJNR Am J Neuroradiol. 1993;14(3):753-762. PubMed
13.Trimble M. Treatment issues for personality disorders in epilepsy. Epilepsia. 2013;54(suppl 1):41-45. PubMed CrossRef
aDepartment of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi, India
*Corresponding author: Shruti Srivastava, MBBS, DNB Psychiatry, MNAMS, Department of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi, 110095 India ([email protected]).
Prim Care Companion CNS Disord 2021;23(1):20l02601
To cite: Srivastava S, Singh A, Punera A. Manic episode misdiagnosed in a case of temporal lobe epilepsy. Prim Care Companion CNS Disord. 2021;23(1):20l02601.
To share: https://doi.org/10.4088/PCC.20l02601
© Copyright 2020 Physicians Postgraduate Press, Inc.
Enjoy this premium PDF as part of your membership benefits!