Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
Psychiatric manifestations of tumors in the pediatric population are not uncommon; however, in the absence of overt neurologic symptoms, the likelihood of serious intracranial pathology is low and routine neuroimaging is not indicated. Nonetheless, it is possible for pediatric patients to present with a brain tumor with psychiatric symptoms but without neurologic findings. Here, we present the case of a young man who evaded diagnosis of pituitary prolactinoma for 3 years despite debilitating psychiatric symptoms.
Delayed Diagnosis of a Pituitary Prolactinoma
Psychiatric manifestations of tumors in the pediatric population are not uncommon; however, in the absence of overt neurologic symptoms, the likelihood of serious intracranial pathology is low and routine neuroimaging is not indicated.1 Nonetheless, it is possible for pediatric patients to present with a brain tumor with psychiatric symptoms but without neurologic findings. Here, we present the case of a young man who evaded diagnosis of pituitary prolactinoma for 3 years despite debilitating psychiatric symptoms.
Case Report
The patient was an 18-year-old Hispanic young man from a low-income family with history of anxiety, asthma, and migraines who presented to the emergency department (ED) with a worsening, gradual, pulsating bitemporal headache, which had not improved with outpatient administration of acetaminophen. He endorsed light-headedness, 40-lb weight loss over the course of a year, decreased social interaction, excessive daytime sleeping, anxiety, poor school performance, and avoidance. The patient had 4 previous visits to the ED for headaches over 3 years and history of child protective services involvement due to medical neglect.
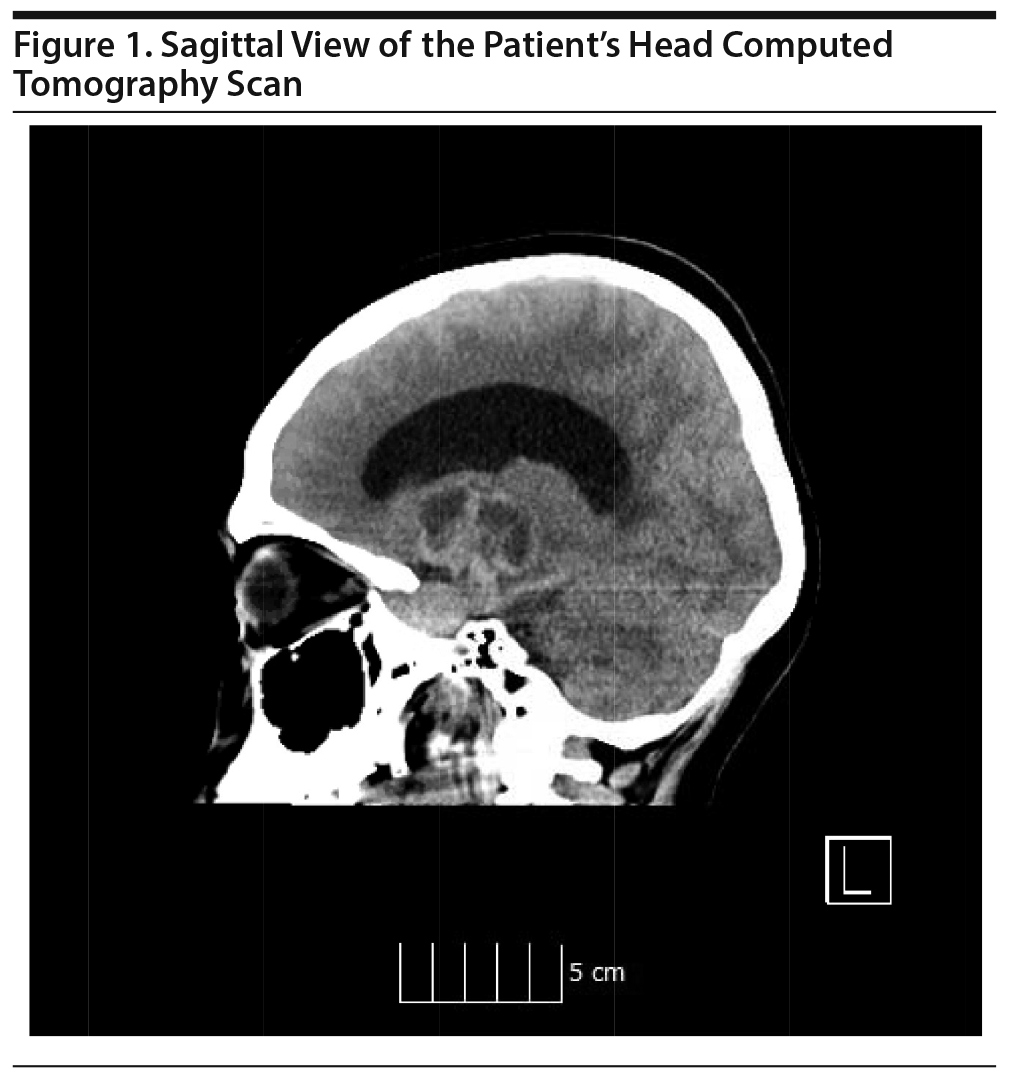
He denied any weakness, numbness, nausea, or emesis; his vital signs and physical examination were noncontributory. Neuroimaging was recommended; however, he left the ED, only to return the next morning with cephalgia and 2 bouts of emesis at home. His symptoms were attributed to long-standing migraines, and a psychiatric consultation was requested for mood symptoms. The patient was diagnosed with depression and offered voluntary inpatient admission, but his family refused, and he was subsequently discharged. He returned to the ED 5 hours later with another bout of emesis and an episode of syncope, with changes in vital signs as indicated in Table 1. He was not oriented to time and had decreased motor strength of 3/5 in all extremities. Head computed tomography revealed a brain mass causing obstructive hydrocephalus (Figure 1). He received resuscitation in the ED, requiring intubation and admission to the surgical intensive care unit for shunt placement. The brain lesion was diagnosed as pituitary prolactinoma. Subsequent chart review revealed the patient’s clinic attendance was poor, which had led to termination of his case.
Discussion
Headaches are a common occurrence in children; however, chronic daily headaches are associated with an increased risk of suicide in adolescents.2,3 While the most common etiology is migraines (62%), followed by tension (22%), the 1% prevalence of tumors4 requires attention. The presence of associated symptoms like apathy, asexuality, adiposity, papilledema, abnormal eye movements, nystagmus, or gait dysfunction4,5 might suggest a prolactinoma. Gender differences exist: males exhibit tumors that are less prevalent but more aggressive, although there are fewer symptoms of hypogonadism compared to women. These differences are more likely to contribute to delayed diagnoses.6
Given the low prevalence of tumors and the high prevalence of headaches, the indication for neuroimaging in the pediatric population has to be carefully weighed. Lewis and Dorbad1 found the yield of neuroimaging in children with uncomplicated migraine and normal neurologic examination to be 3.7%, while the yield in children with chronic daily headache and normal neurologic examination was higher at 16.6%. The current recommendation is that neuroimaging is not warranted in children and adolescents with defined clinical headache syndromes and normal neurologic examinations.1,4 Apathy is a key feature of pituitary tumors and may allow for differentiation from other affective disorders5 but may be misdiagnosed as depression. There may be lower adherence with treatment in minority and low-income families.7
Headaches in the adolescent and young adult population are common, but tumors are not. In the absence of neurologic signs, imaging is not indicated. However, prolactinomas may present with a variety of psychiatric symptoms and with no overt neurologic signs. Delay in diagnosis and treatment may result in poor clinical and social outcomes, notably in the male, minority, and low-income populations due to lower treatment engagement and nature of disease course. Prolactinomas should remain on the list of differential diagnoses for primary care providers, especially if there is history of chronic headaches with psychiatric manifestations.
Published online: March 12, 2020.
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
REFERENCES
1.Lewis DW, Dorbad D. The utility of neuroimaging in the evaluation of children with migraine or chronic daily headache who have normal neurological examinations. Headache. 2000;40(8):629-632. PubMed CrossRef
2.Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433-2445. PubMed CrossRef
3.Wang SJ, Juang KD, Fuh JL, et al. Psychiatric comorbidity and suicide risk in adolescents with chronic daily headache. Neurology. 2007;68(18):1468-1473. PubMed CrossRef
4.Lewis DW, Ashwal S, Dahl G, et al; Quality Standards Subcommittee of the American Academy of Neurology; Practice Committee of the Child Neurology Society. Practice parameter, evaluation of children and adolescents with recurrent headaches: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2002;59(4):490-498. PubMed CrossRef
5.Cohen LM, Greenberg DB, Murray GB. Neuropsychiatric presentation of men with pituitary tumors (the ‘ four A’s ‘ ). Psychosomatics. 1984;25(12):925-928. PubMed CrossRef
6.Fainstein Day P, Glerean M, Lovazzano S, et al. Gender differences in macroprolactinomas: study of clinical features, outcome of patients and ki-67 expression in tumor tissue. Front Horm Res. 2010;38:50-58. PubMed CrossRef
7.Alpern ER, Clark AE, Alessandrini EA, et al; Pediatric Emergency Care Applied Research Network (PECARN). Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21(4):365-373. PubMed CrossRef
aDepartment of Psychiatry, Maimonides Medical Center, Brooklyn, New York
bDepartment of Emergency Medicine, Maimonides Medical Center, Brooklyn, New York
cDepartment of Clinical Psychiatry, Columbia University, New York, New York
dDepartment of Psychiatric Emergency Services, Maimonides Medical Center, Brooklyn, New York
*Corresponding author: Domantas Mikonis, DO, 4802 10th Ave, Brooklyn, NY 11219 ([email protected]).
Prim Care Companion CNS Disord 2020;22(2):19l02522
To cite: Mikonis D, Ghazzawi A, Hoffman TE, et al. Delayed diagnosis of a pituitary prolactinoma. Prim Care Companion CNS Disord. 2020;22(2):19l02522.
To share: https://doi.org/10.4088/PCC.19l02522
© Copyright 2020 Physicians Postgraduate Press, Inc.
Enjoy this premium PDF as part of your membership benefits!