Objective: Providing psychiatric consultation to elite athletes presents unique and complex issues. These patients present with multifaceted medical, psychological, and performance concerns. We provide the first report of professional and ethical quandaries that arise in treating elite athletes and ways to address them.
Method: We identified studies through a MEDLINE search. Search terms included the following, individually and in combination: psychiatry, athletes, elite athletes, professional athletes, sports, sport psychiatry, mental illness, major depressive disorder, depression, bipolar disorder, suicide, anxiety, generalized anxiety disorder, obsessive compulsive disorder, social phobia, social anxiety disorder, panic disorder, post traumatic stress disorder, specific phobia, psychosis, eating disorders, anorexia nervosa, bulimia nervosa, attention deficit hyperactivity disorder, substance abuse, substance dependence, addiction, alcohol, anabolic steroids, stimulants, antidepressants, mood stabilizers, anxiolytics, antipsychotics, sedative-hypnotics, psychotropics, medications, and psychiatric medications. We restricted results to the English language and used no date restrictions. We retrieved all articles discussing psychiatric diagnosis or psychiatric treatment of athletes. We reviewed each article’s findings to see if they applied to elite athletes and reviewed the references of each article for additional articles that had been missed in the initial search and that might include findings relevant to the scope of our article. Our search found no controlled data to guide treatment in working with elite athletes. We describe the literature that does exist and present 4 case examples to illustrate diagnostic and treatment issues with elite athletes.
Results: Patient and family characteristics are described as they bear on treatment context. The key pitfalls that interfere with treatment are listed, and clinical guidelines to improve outcomes are suggested. Specific key pitfalls that interfere with treatment include elite athletes’ expecting “special treatment,” issues of flexibility in treatment to accommodate travel schedules and the need for privacy, and inclusion of coaches and significant others in treatment. Recommendations for working with this population include being flexible within reason about timing of sessions, involving family members when relationship issues are involved, and not compromising on delivering the appropriate treatment, including medications and hospitalizations as necessary.
Conclusions: The challenges of treating the elite athlete are great, but successful treatment is possible.
J Clin Psychiatry 2012;73(5):640-644
© Copyright 2012 Physicians Postgraduate Press, Inc.
Submitted: September 8, 2011; accepted October 31, 2011 (doi:10.4088/JCP.11r07381).
Corresponding author: Ira D. Glick, MD, 401 Quarry Rd, Ste 3365, Stanford, CA 94305 ([email protected]).
Find more articles on this and other psychiatry and CNS topics:
The Journal of Clinical Psychiatry
The Primary Care Companion for CNS Disorders
ABSTRACT
Objective: Providing psychiatric consultation to elite athletes presents unique and complex issues. These patients present with multifaceted medical, psychological, and performance concerns. We provide the first report of professional and ethical quandaries that arise in treating elite athletes and ways to address them.
Method: We identified studies through a MEDLINE search. Search terms included the following, individually and in combination: psychiatry, athletes, elite athletes, professional athletes, sports, sport psychiatry, mental illness, major depressive disorder, depression, bipolar disorder, suicide, anxiety, generalized anxiety disorder, obsessive compulsive disorder, social phobia, social anxiety disorder, panic disorder, post traumatic stress disorder, specific phobia, psychosis, eating disorders, anorexia nervosa, bulimia nervosa, attention deficit hyperactivity disorder, substance abuse, substance dependence, addiction, alcohol, anabolic steroids, stimulants, antidepressants, mood stabilizers, anxiolytics, antipsychotics, sedative-hypnotics, psychotropics, medications, and psychiatric medications. We restricted results to the English language and used no date restrictions. We retrieved all articles discussing psychiatric diagnosis or psychiatric treatment of athletes. We reviewed each article’s findings to see if they applied to elite athletes and reviewed the references of each article for additional articles that had been missed in the initial search and that might include findings relevant to the scope of our article. Our search found no controlled data to guide treatment in working with elite athletes. We describe the literature that does exist and present 4 case examples to illustrate diagnostic and treatment issues with elite athletes.
Results: Patient and family characteristics are described as they bear on treatment context. The key pitfalls that interfere with treatment are listed, and clinical guidelines to improve outcomes are suggested. Specific key pitfalls that interfere with treatment include elite athletes’ expecting “special treatment,” issues of flexibility in treatment to accommodate travel schedules and the need for privacy, and inclusion of coaches and significant others in treatment. Recommendations for working with this population include being flexible within reason about timing of sessions, involving family members when relationship issues are involved, and not compromising on delivering the appropriate treatment, including medications and hospitalizations as necessary.
Conclusions: The challenges of treating the elite athlete are great, but successful treatment is possible.
J Clin Psychiatry 2012;73(5):640-644
© Copyright 2012 Physicians Postgraduate Press, Inc.
Submitted: September 8, 2011; accepted October 31, 2011 (doi:10.4088/JCP.11r07381).
Corresponding author: Ira D. Glick, MD, 401 Quarry Rd, Ste 3365, Stanford, CA 94305 ([email protected]).
Working with high profile individuals, including elite athletes, creates unique challenges for sports physicians, including sports psychiatrists. Certain characteristics are shared by many elite athletes and may make psychiatric interventions more challenging. We identified studies through a MEDLINE search. Search terms included the following, individually and in combination: psychiatry, athletes, elite athletes, professional athletes, sports, sport psychiatry, mental illness, major depressive disorder, depression, bipolar disorder, suicide, anxiety, generalized anxiety disorder, obsessive compulsive disorder, social phobia, social anxiety disorder, panic disorder, post traumatic stress disorder, specific phobia, psychosis, eating disorders, anorexia nervosa, bulimia nervosa, attention deficit hyperactivity disorder, substance abuse, substance dependence, addiction, alcohol, anabolic steroids, stimulants, antidepressants, mood stabilizers, anxiolytics, antipsychotics, sedative-hypnotics, psychotropics, medications, and psychiatric medications. We restricted results to the English language and used no date restrictions. We retrieved all articles discussing psychiatric diagnosis or psychiatric treatment of athletes. We reviewed each article’s findings to see if they applied to elite athletes and reviewed the references of each article for additional articles that had been missed in the initial search and that might include findings relevant to the scope of our article. Our search found no controlled data to guide treatment in working with elite athletes. This article starts with an introduction to sports psychiatry in general and then describes the literature that does exist on the unique issues to be considered in working with elite athletes. Many of the principles we discuss also apply to competitive athletes, including youth, at non-elite levels. These principles are illustrated with 4 patient cases. We conclude with a list of “dos” and “don’ ts” for the physician who works with elite athletes.
SPORTS PSYCHIATRY
The specialty of sports psychiatry has continued to evolve and expand over the past 2 decades. In its origin in the medical literature in 1990, Begel1 described the specialty as “the application of the principles of and practice of psychiatry to the world of sports.”(p606) Glick and colleagues2 identified 3 key issues that led to the need for sports psychiatry as a specific subspecialty. Foremost, they noted that “an athlete’s state of mind has a significant impact on performance.”(p608) Secondly, “participation in sports affects the mood, thinking, personality, and health of the participant in specific ways.”(p608) Last, “the psychiatric care of the athlete must be adapted to the athletic context in order to be effective.”(p608) The authors also attested that the sports psychiatrist must possess unique skills in treating not only the athlete but also the athlete’s family, significant others, and the entire system comprising coaches and teammates. Glick et al3 delineated the primary aims of the specialty as (1) optimizing physical health, (2) ethically improving athletic performance by enhancing positive psychological strengths, and (3) managing psychiatric symptoms over the lifetime of the athlete with the aim of maintaining athletic performance.
Reardon and Factor4 recently conducted an extensive, systematic review of the literature on the diagnosis and treatment of mental illness in athletes. This review provides information on the frequency and unique features of psychiatric disorders among athletes. They report that depression is equally common in athletes and nonathletes, although in athletes it can be precipitated by overtraining, injury, poor performance, and retirement.5 The study by Reardon and Factor also revealed that eating disorders and substance abuse appear to be the most common psychiatric problems among athletes. Up to 60% of female athletes in certain sports suffer from eating disorders. Among substance abuse disorders in athletes, alcohol is abused more than any other substance.4 Collegiate athletes have been found to engage in higher rates of alcohol abuse than their nonathlete peers.6 Moreover, findings reveal a potential relationship between psychopathology and alcohol abuse among these athletes.7
Fortunately, most athletes will be appropriately concerned about using substances or medication that could impact their performance. Certain medications are prohibited by some sport governing bodies, while others, such as stimulants, may be allowed only with completion of therapeutic use exemptions.4 It is important for the sports physician to have familiarity with the guidelines the athlete has to follow before prescribing any medication.
- Although elite, professional sports teams have large medical and nonmedical staff (sometimes including psychologists) to improve performance, there has been an almost complete absence of psychiatrists to diagnose and treat psychiatric problems and disorders—in part because of the stigma of mental illness.
- Active and retired athletes have psychiatric problems and disorders like nonathletes and require diagnosis and treatment to function in their sport and in the rest of their lives. Some modifications (depending on the clinical situation) of standard psychiatric interventions may be necessary.
THE ATHLETE-PATIENT
Though athletes when compared to the general population have an equal risk for the development of psychiatric illness, they generally do not seek out psychiatric treatment.8 This is due to the social stigma regarding psychiatric illness and the notion that mental health treatment represents weakness to athletes and coaches.8,9
Schwenk10 noted that the current conceptualization of mental illness in athletes is “fraught with stigmatization, denial, and dichotomous paradigms of ‘ psychological’ versus ‘ physical’ disease, which are inaccurate, unhelpful, and deprive the athlete of effective care.”(p4) More specifically, sports physicians tend to label athlete-patients with “overtraining” when they present with complaints of fatigue, amotivation, trouble sleeping, and irritability. A nonathlete patient presenting with these same symptoms would be suspected of having major depressive disorder (MDD) and would be treated accordingly.11 The hesitation in diagnosing mental illness in athletes persists despite evidence showing significant mood disturbances, including elevations in depression, tension, and anger, in many seriously injured athletes.12
Accurate diagnosis is a vital first step in laying the foundation for successful treatment.8 The signs and symptoms defining psychiatric diagnoses (eg, MDD, alcohol abuse) should be explored.8 Importantly, denial of psychological problems and of pain is common among successful athletes.8,13 To help obtain accurate information, a clinical interview should be conducted not only with the athlete, but also as indicated with family members, coaches, agents, and teammates. Of course, the sports psychiatrist must exercise judgment and maintain confidentiality when contacting collateral sources of information.8
THE ELITE ATHLETE
While the research in sports psychiatry has grown steadily, little attention has been placed on the most complex patient within this group: the elite athlete. The McGraw-Hill Dictionary of Modern Medicine14 defines the elite athlete as “an athlete with potential for competing in the Olympics; elite athletes are at increased risk for injuries, given the amount of training, for psychological abuse by coaches and parents, and self-abuse.”(p216) In many respects, this definition also describes serious athletes at non-elite levels.
As a product of the praise and attention these athletes receive, they can present unique and challenging characteristics as compared to their noncompetitive counterparts. Elite athletes are accustomed to being the “VIP” and in charge. People often are particularly solicitous of their opinions. They are used to being in the spotlight. They may have what has been termed “situational narcissism.” These traits may make it difficult for them to seek or accept assistance. On the other hand, elite athletes are used to having agents, family, and coaches giving them advice and support. In some cases, relationships with parents may have been supplanted by other relationships such as those with coaches. Accordingly, they may develop a rapid and powerful transference reaction to the physician.
In addition to the impact of public attention and personality traits on psychiatric treatment, elite athletes often have lifestyle factors that impact mental health care. Entitlement and control issues, especially regarding scheduling and fees, may emerge early in treatment. Most elite athletes work very long hours and require continuous travel. They are used to being wealthy, and, at the same time, are not used to paying for much. Others often take care of their daily needs and travel arrangements. Services and goods are given for free. Thus, setting and collecting fees may be more challenging than usual. Many athletes may be world-travelers, and yet their development may have been slowed in some ways. They may be lacking a general education. Social relationships are often colored by their sports lives and success. They may not be used to privacy and, thus, individual psychiatric treatment may seem unusual. Athletes may not easily share emotions and may have been taught to “work through pain.” This coping style may have worked well for many years, contributing to a reluctance to seek psychotherapy.
In summing up these unique psychiatric issues pertaining to this subgroup of athletes, Glick et al8 noted that
Emotional maturity may be delayed in professional athletes due to their iconization—placing elite athletes on a pedestal and having others insulate them from the stresses and problems of daily life.(p773)
and
The pampered, highly paid, professional athlete may be developmentally immature, that is, have a childlike personality in contrast to a “macho adult” presentation to the public.(p776)
Sands et al15 discussed the difficulties in conducting research with elite athletes. Finding a group of elite athletes to participate in clinical research can be problematic, as participant willingness, adequate sample size, and homogeneity are difficult to attain.16 Since this population is small, authors have recommended the more feasible use of single-subject design.15 Given the higher potential for breaching patient confidentiality when reporting treatment details of individuals in the public eye, the number of published cases of mental illness in high-profile athletes is understandably small. The following disguised case reports utilize this method and illustrate the principles discussed above.
CASE REPORTS
Case 1: History
A male professional athlete presented for treatment because of an exacerbation of a mood disorder. The patient refused to have his wife involved in treatment or to have anyone from his team know the seriousness of his condition. His psychiatrist started him on treatment with an antidepressant, and after 5 weeks, his symptoms were mildly improved. After a crucial mistake in a game, which cost his national team the victory, he became more depressed and suicidal. He refused hospitalization, which was recommended by the psychiatrist. After another poor performance in the subsequent game, he committed an impulsive act of suicide.
Case 1: Discussion
This case highlights the difficulty in getting many athletes to follow good clinical practices, eg, hospitalization for severe depression and involvement of collateral support systems. The psychiatrist confronted the challenges of whether to break confidentiality protections to involve others in this very ill patient’s care and whether to pursue involuntary hospitalization. Although this case provides an extreme example of the dire outcomes that can occur, we believe that non-enforcement of treatment recommendations by providers treating elite athletes is common. Providers should strive to follow good clinical judgment regardless of the patient’s elite status.
Case 2: History
The young wife of a high-profile athlete and mother of a toddler presented with a chief complaint of marital dissatisfaction. She felt overwhelmed with the responsibilities of motherhood, and her husband was traveling for much of the season. They met in her home state, but he played for a team out of town. She had relocated to be with him, but in the process had given up her support system. She was born and raised in a close multicultural family, the other members of which remained in her home state. She temporarily returned to the area to be with her mother to seek treatment. She was anxious and tearful. She was seen individually for several months, was treated with medication and psychotherapy, and improved.
During the off-season, her husband joined her in her home state and participated fairly regularly in sessions. When the season resumed, she and her husband returned to their home together to pursue treatment in that area. Despite her moving to be with him, he did not attend sessions. Months into the season, she returned to her home state, as her symptoms of depression returned. The provider now suspected that she was abusing substances. The couple separated and divorced.
Case 2: Discussion
An athlete may require special consideration due to travel schedules. The case demonstrates the flexibility a spouse must display in some relationships (and that we may need to mimic as treaters). Even with a flexible approach, though, for successful treatment of symptoms that are primarily related to the couple or family, the athlete-patient must attend sessions regularly.
Case 3: History
Mr A was a multiply divorced, retired star athlete. He requested evaluation because of a suspicion that his peers were unfairly judging him about his request for disability. He emphasized he was a “former all-star and could not be treated this way.” He insisted on bringing voluminous records and reading them out loud to the psychiatrist. Mental status examination revealed a thought disorder and paranoia. He denied substance abuse.
Mr A refused all treatment recommendations. He denied he had a mental illness, declined to bring a significant other to the session, and did not return for further treatment.
Case 3: Discussion
This case presents the challenge of a patient with severe psychiatric illness and limited insight. In this situation, a significant other would have been necessary to provide collateral information and to encourage the patient to undergo treatment. Serious psychiatric symptoms, such as psychosis, superimposed on an athlete’s sense of entitlement and need for control make for a particularly difficult situation, almost always which will necessitate involvement of significant others.
Case 4: History
A psychiatrist was called by the agent of a high-profile athlete who was out of town competing and was involved in an accident that led to a fatality. The athlete was requesting to be seen quickly because of severe anxiety and insomnia since the accident. The physician agreed to see him Saturday morning to expedite the visit and avoid his being seen by other patients. At the end of the visit, the athlete requested to pay with a credit card. The psychiatrist was unable to process the card and thus requested he pay at the next visit. Instead, 2 days later 4 tickets to a game arrived with a thank you note from the agent. Though the monetary value of the tickets was comparable to the visit charge, the doctor called the agent to explain that it would be unethical to accept the tickets. The agent understood the concern and sent a check, but also insisted that the psychiatrist keep the tickets. The patient never returned for a second visit.
Case 4: Discussion
This case illustrates the need to maintain as “normal” an atmosphere as possible. Simple accommodations, such as seeing a patient outside of usual hours, may hamper the therapeutic process. The case was further complicated by the involvement of the agent, who may have interfered with the treatment. In this case, the agent was involved with the physician for scheduling and payment, which prevented the psychiatrist from getting information directly from the patient before and after the appointment.
We considered adding cases with “better” outcomes, all of which embody the principles of working with elite athletes that we describe above but would not as clearly illustrate the potential pitfalls in working with this population. To be sure, success stories (such as the anecdote in the discussion below) in working with elite athletes are plentiful, as these patients are often quite motivated to get well as quickly as possible.
DISCUSSION
As illustrated in the cases, elite athletes are accustomed to “special treatment” and may expect it from their health care providers. Some flexibility in treatment may be necessary for privacy and to accommodate travel schedules, but establishing a relationship with a patient that does not follow the “usual rules” can lead to unintended boundary violations.
Elite athletes are used to health care providers coming to them, rather than the other way around, for treatment on the court or at practice sessions. Additionally, because confidentiality issues are important to high profile public figures, they may expect providers to come to their home or hotel to avoid public exposure. The psychiatrist must carefully weigh the pros and cons of evaluating any patient outside the usual office practice. Coaches, trainers, or agents as well as family members may want to be included in treatment, as they are used to being involved in the athlete’s day-to-day life. While involvement of these significant others can be intrusive, they can also provide crucial collateral information and support patient adherence with treatment recommendations. Thus, we err on the side of including these significant others.
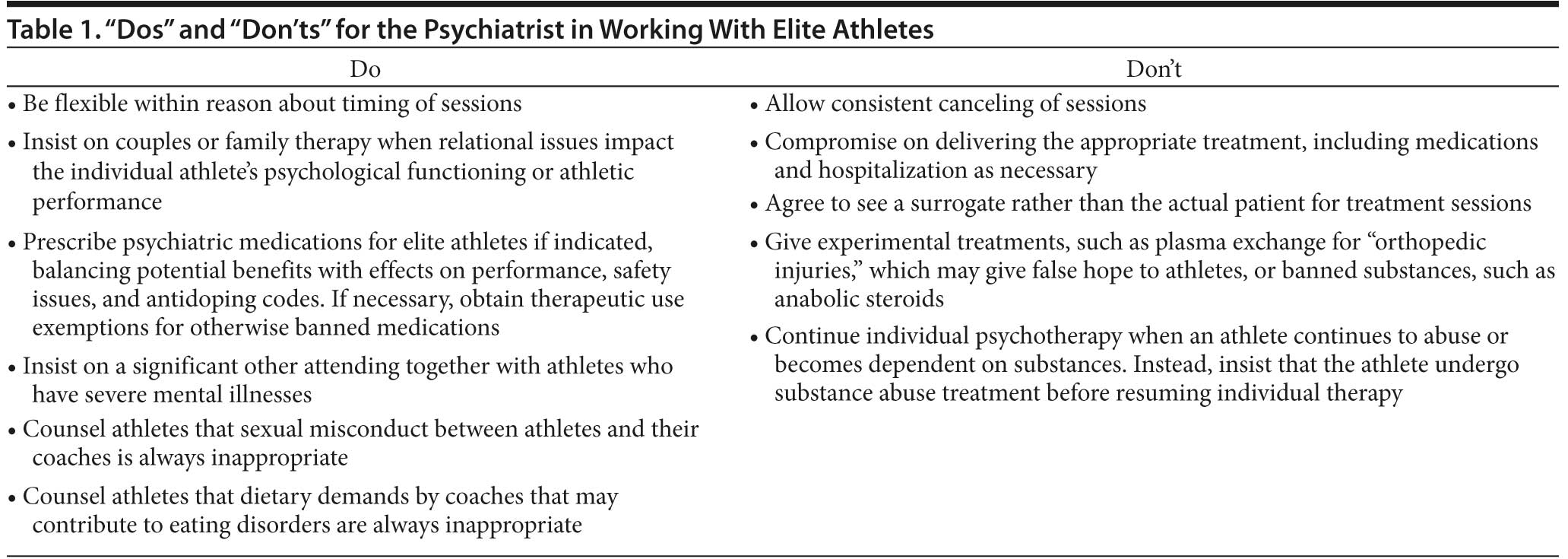
This article focuses on the unique issues involved in treating elite athletes. The guiding principle is “flexibility with appropriate boundaries.” In addition, we offer a list of “dos” and “don’ ts” derived from the existing literature and the authors’ professional work with this population (Table 1).
In conclusion, although some clinical guidelines can be bent in treating elite athletes, most should not. The challenges of treating the elite athlete are great, but successful treatment is possible with adherence to the above recommendations. While our cases emphasize challenges, another recent anecdote illustrates the potential for success. A professional player was arrested for actions stemming from psychiatric symptoms. He was in the manic phase of bipolar disorder and was required to see a psychiatrist. The psychiatrist worked with the agent, family, patient, and other officials. Thereafter, with recognition of the gravity of the consequences of his mental illness if untreated, it was written into his contract that he would need to see his psychiatrist regularly and take his medication to be allowed to play. The psychiatrist enforced treatment recommendations, the athlete adhered to them, and all involved were satisfied with the care provided. This anecdote demonstrates the teamwork that it takes to yield optimal outcomes. Importantly, many of the tenets we have addressed in this article, including the need for teamwork, also apply to other competitive, but non-elite, athletes.
Brooks16 summarizes future directions for work with top-level athletes in explaining,
Increasingly, the need for psychiatric consultation and intervention is being recognized in the world of professional sports. The need for more research providing empirical evidence, insight, and understanding into the coping and adjustment aspects of the professional athlete is clear.(p264)
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, no investigational information about pharmaceutical agents that is outside US Food and Drug Administration-approved labeling has been presented in this article.
Author affiliations: Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, California (Dr Glick); Department of Psychology, School of Liberal Arts, Georgia Gwinnett College, Lawrenceville (Dr Stillman); Department of Psychiatry, University of Wisconsin School of Medicine and Public Health, Madison (Dr Reardon); and Department of Psychiatry and Behavioral Sciences, University of Miami School of Medicine, Miami, Florida (Dr Ritvo).
Financial disclosure: Dr Glick has a small amount of equity in Johnson & Johnson. Drs Stillman, Reardon, and Ritvo have no personal affiliations or financial relationships with any commercial interest to disclose relative to the article.
Funding/sources: None reported.
REFERENCES
1. Begel D. An overview of sport psychiatry. Am J Psychiatry. 1992;149(5):606-614. PubMed
2. Glick ID, Kamm R, Morse E. The evolution of sport psychiatry, circa 2009. Sports Med. 2009;39(8):607-613. PubMed doi:10.2165/00007256-200939080-00001
3. Glick ID, Morse E, Reardon CL, et al. Sport psychiatry—a new frontier in a challenging world. Die Psychiatrie (Stuttg). 2010;7:249-253.
4. Reardon CL, Factor RM. Sport psychiatry: a systematic review of diagnosis and medical treatment of mental illness in athletes. Sports Med. 2010;40(11):961-980. PubMed doi:10.2165/11536580-000000000-00000
5. Burton RW. Mental illness in athletes. In: Begel D, Burton RW, eds. Sport Psychiatry. New York, NY: W W Norton & Company, Inc; 2000:61-81.
6. Martens MP, Cox RH, Beck NC. Negative consequences of intercollegiate athlete drinking: the role of drinking motives. J Stud Alcohol. 2003;64(6):825-828. PubMed
7. Miller BE, Miller MN, Verhegge R, et al. Alcohol misuse among college athletes: self-medication for psychiatric symptoms? J Drug Educ. 2002;32(1):41-52. PubMed doi:10.2190/JDFM-AVAK-G9FV-0MYY
8. Glick ID, Horsfall JL. Diagnosis and psychiatric treatment of athletes. Clin Sports Med. 2005;24(4):771-781, vii. PubMed doi:10.1016/j.csm.2005.03.007
9. Linder DE, Brewer BW, Van Raalte JL, et al. A negative halo for athletes who consult sport psychologists: replication and extension. J Sport Exerc Psychol. 1991;13:133-148.
10. Schwenk TL. The stigmatisation and denial of mental illness in athletes. Br J Sports Med. 2000;34(1):4-5. PubMed doi:10.1136/bjsm.34.1.4
11. Sundgot-Borgen J, Torstveit MK. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med. 2004;14(1):25-32. PubMed doi:10.1097/00042752-200401000-00005
12. Quinn AM, Fallon BJ. The changes in psychological characteristics and reactions of elite athletes from injury onset until full recovery. J Appl Sport Psychol. 1999;11(2):210-229. doi:10.1080/10413209908404201
13. Pavelski R, Kryden A, Steiner H, et al. Adaptive styles in elite collegiate athletes [abstract]. Presented at the 45th Annual Meeting of The American Academy of Child and Adolescent Psychiatry; November 1998; Anaheim, CA.
14. Segen JC. Concise Dictionary of Modern Medicine. New York, NY: The McGraw-Hill Companies, Inc; 2002.
15. Sands WA, McNeal JR, Stone MH. Plaudits and pitfalls in studying elite athletes. Percept Mot Skills. 2005;100(1):22-24. PubMed doi:10.2466/pms.100.1.22-24
16. Brooks YB. Building a healthy work-lifestyle balance for professional athletes and their families. In: Rozensky RH, Johnson NG, Godheart CD, et al, eds. Psychology Builds a Healthy World: Opportunities for Research and Practice. Washington, DC: American Psychological Association; 2003:256-265.