Empowering mental health professionals with peer-reviewed psychiatric research and insights
Just Published
A Primer on Individual Participant Data Meta-Analysis and Its Strengths and Limitations
July 7, 2025
Global Population-Based Study on the Association Between Ketamine and Esketamine with Suicidality Using WHO VigiBase
July 7, 2025
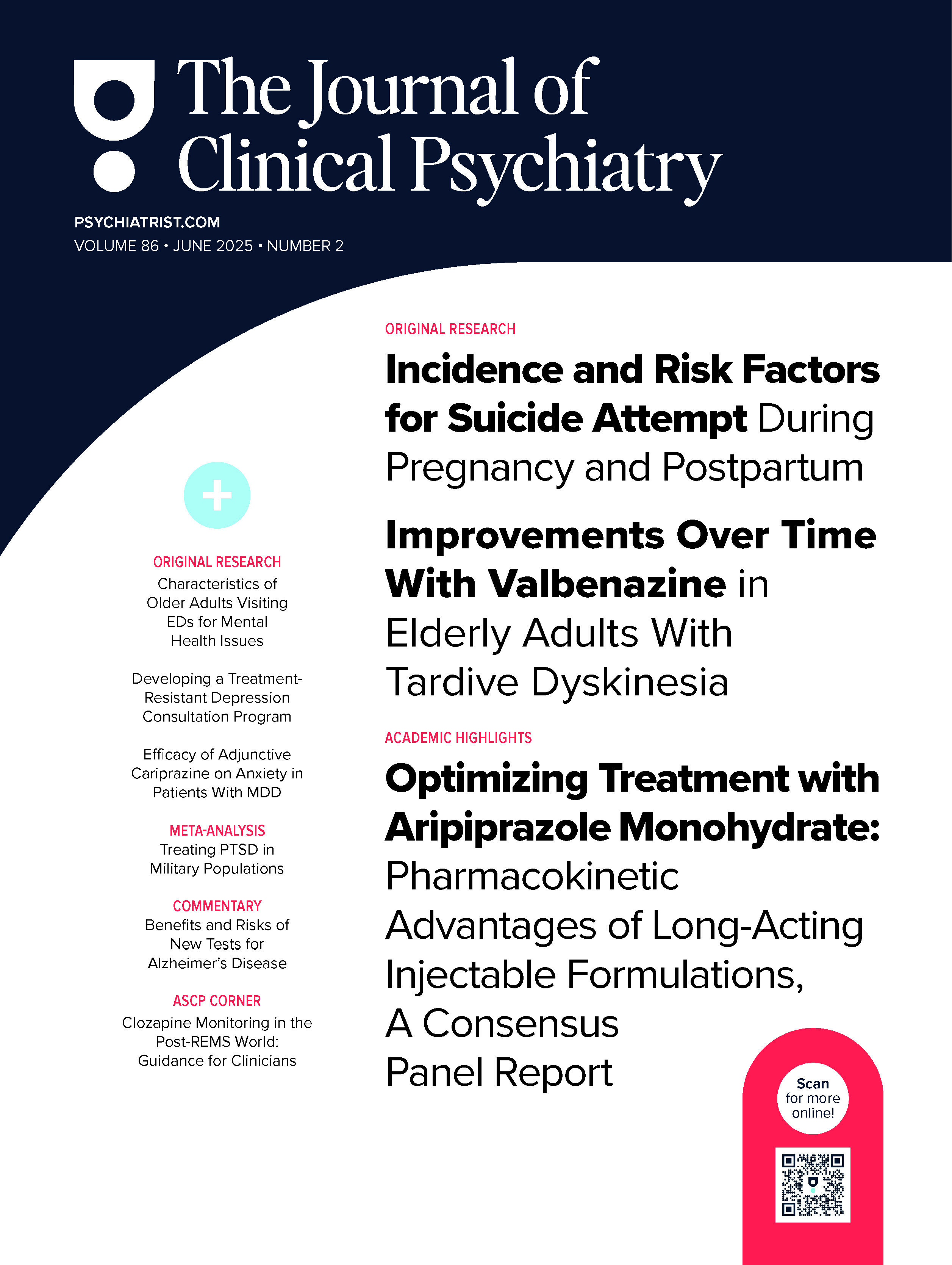
Vol 86 • 2025 • Number 2
Read the Current Issue
Original Research
Incidence and Risk Factors for Suicide Attempt During Pregnancy and Postpartum
Original Research
Valbenazine in Elderly Adults With Tardive Dyskinesia
Academic Highlights
Optimizing Treatment With Aripiprazole Monohydrate: Pharmacokinetic Advantages of Long-Acting Injectable Formulations, A Consensus Panel Report
Original Research
Older Adults Visiting Emergency Departments for Mental Health Issues:A CHIRPP Database Study
Consensus Statement
Developing a Treatment-Resistant Depression Consultation Program, Part I: Practical and Logistical Considerations
Brief Report
Psychosocial Correlates of Optimism among US Military Veterans
Original Research
Differentiating Subtypes of MDD Using Serum Biomarkers
June 23, 2025
Bright Light Therapy in the Morning or Midday for Nonseasonal Depression in Bipolar Disorder
June 23, 2025
Review Articles
Cognitive Effects of ECT in Schizophrenia: A Review
June 5, 2024
Read articles from ASCP Corner
Letters to the Editor
Mental Health Assessment and Psychosocial Intervention in Maternal-Fetal Interventions
November 18, 2024
Commentaries
Lower Risk of Cardiovascular Disorders in Antidepressant-Treated Women Veterans: Encouraging Findings but Concerns Remain
May 7, 2025
Eating Disorders Among Transgender and Gender Diverse People: Qualitative Analysis of Reddit Threads
March 10, 2025
More JCP Articles
Association Between Adult Sexual Assault and Psychiatric Disorders: Results From NESARC
June 16, 2025
Schizophrenia, Antipsychotic Drugs, and Risk of Breast Cancer
June 16, 2025
Cognitive Behavioral Therapy for Insomnia with Prolonged Exposure Compared to Sleep Hygiene and Prolonged Exposure
June 4, 2025
Idiopathic Hypersomnia: Recognition and Management in Psychiatric Practice
June 2, 2025
Outpatient Ketamine Prescribing Practices in Psychiatry in the US: A Nationwide Survey Study
May 26, 2025