Electroconvulsive Therapy in Patients With Skull Defects or Metallic Implants: A Review of the Literature and Case Report

ABSTRACT
Context: Head injury is often associated with psychiatric morbidity. While it is well understood that the loss of critical areas of the brain may play a role in cognitive dysfunction and change in personality, head injury can also have profound effects on mood and cognition. The role of medications in the treatment of mood disorders associated with brain injury is well documented, and there is also evidence favoring the use of electroconvulsive therapy (ECT) in this context. However, data are limited on the use of ECT in patients with skull defects or metallic head implants.
Evidence Acquisition: First, a review of the literature on use of ECT in patients with metallic head implants is provided. Electronic databases and online sites, including PubMed, Cochrane Library of Systematic Reviews, and UpToDate, were used to search for relevant articles and case reports on the use of ECT in patients with and without metallic implants in the head (1964 to 2009). The search terms electroconvulsive, electroconvulsive therapy, ECT, electroshock therapy, EST, head injury, brain injury, metallic plates, metallic implants, skull prosthesis, and depression were used interchangeably. The search produced 7 articles discussing exclusively the use of ECT in patients with a metallic skull plate. Second, the case of the successful and safe use of ECT in an individual with a previous history of brain trauma and metallic plate implantation is described.
Results: Most cases of head injury are managed by neurologists and rehabilitation consultants; the more severe cases of depression and other mood disorders tend to be referred for specialist psychiatric care. With greater degrees of deficit following head injury, management becomes more complicated. Our patient showed positive results with ECT, including improvement in depressive features and resolution of suicidal ideas/plans.
Conclusion: ECT is an effective and safe alternative in patients with a history of brain trauma and metallic plate implantation who subsequently develop treatment-resistant depression and associated suicidal ideas or plans refractory to management with medications.
Prim Care Companion CNS Disord 2012;14(2):doi:10.4088/PCC.11r01228
© Copyright 2012 Physicians Postgraduate Press, Inc.
Submitted: June 6, 2011; accepted August 4, 2011.
Published online: March 1, 2012.
Corresponding author: Shabbir Amanullah, MD, Hillsborough Hospital, PO Box 1929, Charlottetown, Prince Edward Island, Canada C1A 7N5 ([email protected]).
Brain injury is common. In the United States, about 1.4 million people suffer from brain injury resulting from various causes.1 Individuals older than 75 years of age have the highest rates of traumatic brain injury-related admission to the hospital and mortality from brain injury.1 Medical complications are varied and include seizures,2 deep venous thrombosis,3 stress ulcers, urinary incontinence, and normal pressure hydrocephalus.4 Given the financial difficulties, stress on relationships, organic mood disorders, and possible personality changes that an individual faces after head injury, the availability of effective treatments is crucial for these patients.
Head injury is often associated with psychiatric morbidity, and the rate of mood disorder may be up to 40%.5 While the loss of critical areas of the brain may play a direct role in cognitive dysfunction and change in personality and mood, brain injury can also affect the brain’s neurochemistry and thus secondarily affect mood5 and cognition.6 Subtle cognitive deficits may erroneously be subsumed under the “functional” category.6 Atrophy of the hippocampus and frontal cortical areas may have particularly significant consequences.7 Most cases of head injury are managed by neurologists and rehabilitation consultants, and the more severe cases of depression and other mood disorders tend to be referred for specialist psychiatric care. With greater degrees of deficit following head injury, management becomes more complicated.8
The report of the National Institutes of Health consensus developmental panel on rehabilitation of persons with traumatic brain injury itemizes the common behavioral deficits in such individuals and lists among others agitation, aggression, sexual dysfunction, mood disorders, and anxiety disorders.9 This report highlights the role of psychotherapy and psychopharmacologic agents but makes no mention of electroconvulsive therapy (ECT).9
The role of medications in the treatment of mood disorders associated with brain injury is well documented,10,11 and there is evidence of benefit from ECT in this context.12 Data are, however, sparse on the use of ECT in patients with skull defects or metallic head implants. Theoretical concerns about the use of ECT in patients with skull defects or metallic implants pertain to the possibility of the passage of excessive amounts of electricity with consequential damage to brain tissue and could account for its infrequent use in practice and the lack of much description in the medical literature. The hypothetical neuronal injury attributed to prosthetic heating during ECT was successfully refuted in 1 case study, with the caveat that equidistant electrode placement from the prosthesis would be beneficial.13
ECT has been used effectively in patients with metastatic brain cancer without raised intracranial pressure.14 Similarly, ECT has been utilized in patients with normal pressure hydrocephalus without raised intracranial pressure.4 The status of recent and open head injury as a relative contraindication to ECT was negated by several reports describing individuals who developed severe major depression refractory to medical therapy after sustaining gunshot wounds and who were then successfully treated with ECT.15-17 Mania following head injury has also been successfully treated with ECT.18
We hereby provide a review of the relevant literature on the use of ECT in patients with metallic head implants. Also, the successful and safe use of ECT in a patient with a previous history of brain trauma and metallic plate implantation is described.
review of the literature
Method
Electronic databases and online sites, including PubMed, Cochrane Library of Systematic Reviews, and UpToDate, were used to search for relevant articles and case reports on the use of ECT in patients with metallic implants in the head. The terms electroconvulsive, electroconvulsive therapy, ECT, electroshock therapy, EST, head injury, brain injury, metallic plates, metallic implants, skull prosthesis, and depression were used interchangeably to ensure the greatest range of returns. Literature consistent with the topic of ECT use in patients with metallic head implants was drawn from a variety of journal sources using MeSH subject headings.

- Head injury and metallic plate implantation with subsequent severe depression is a challenging clinical problem, and a high suicide risk makes effective treatment imperative.
- A course of electroconvulsive therapy (ECT) in such patients and, if needed, maintenance ECT is a safe and effective option.
An initial review of the literature of the past 10 years (July 1989 to July 2009) on the use of ECT in patients with metallic skull plates yielded only 3 relevant articles in PubMed. The literature search was then broadened to include all brain-injured patients, including those with and without metallic skull plates, and the date limits of the literature review were modified to include all relevant literature written from the first discussions of the use of this procedure on such patients, originating back to 1964. These adaptations to the scope of brain injuries and the timeline allowed a scan of over 45 years of relevant data and research on the use of ECT in this subgroup of patients, for a total of 58 studies. Of these 58 articles, we found 4 more relevant articles, for a total of 7 articles in PubMed discussing exclusively the use of ECT in patients with a metallic skull plate.
Results
Table 1 lists the studies that described patients with metallic head implants and/or skull defects. These studies were selected on the basis of information provided about the parameters used. Studies that gave no clear indications of parameters used were not included. Studies involving spinal Harrington rods and maxillofacial repairs without skull defects were also excluded.

Case Report
Mr A is a 54-year-old man with a history of traumatic brain injury at the age of 4 years, when he was hit by a car and lost consciousness for 2 weeks. Surgical treatment included the placement of a metallic clip in the left parietal region for a vessel tear (patient recall). Mr A had academic difficulties related to poor concentration and difficulty processing information and dropped out of school after grade 8 at the age of 13 years. As an adolescent, substance abuse was significant (lysergic acid diethylamide, cannabis, and alcohol) prior to Mr A suffering a generalized tonic-clonic seizure just before his 18th birthday. Since then, he has received anticonvulsant medication, with no established recurrences.
Mr A went on to work and later married and settled down to family life. Over the ensuing years, however, he suffered from bouts of low mood that fulfilled DSM-IV criteria for major depressive disorder with a recurrent pattern. Some of the bouts of depression were severe, with 2 attempted suicides by overdoses with prescribed medications. Mr A had a history of lapses in memory dating back 20 years. Various antidepressants from different groups were prescribed in adequate doses for adequate durations, with inadequate to poor response. It was during this phase that Mr A’s son died by suicide, and his depression worsened. Mr A was preoccupied, with poor appetite and sleep.
At presentation to our mental health service, Mr A had low mood, lack of energy, sadness (with no diurnal pattern), lack of interest, guilt, irritability, and suicidal ideas with plans. His Global Assessment of Functioning (GAF) score was 40. His medications included phenytoin 100 mg bid; carbamazepine controlled release 1,000 mg po daily; dimenhydrinate 50 mg po daily; lorazepam 1 mg po daily as needed; sertraline 150 mg po daily; clonazepam 2 mg po 1-2 tablets daily; and risperidone 2 mg po daily. A consultant neurologist concluded that Mr A had epilepsy with partial and secondarily generalized tonic-clonic seizures. There were 2 types of seizures, the first characterized by a sensation of his tongue getting thicker and speech becoming slurred, with full recall of these events, and a second type characterized by loss of consciousness and tongue biting, with no recall, headache, and feeling sleepy on recovery. There was a positive family history of suicide and alcohol dependence, with a first-degree relative dying by suicide and another with alcohol dependence syndrome.
Soon after Mr A’s contact with our services, we noted a decline in his mood and worsening in his suicidal ideation. Mr A was admitted to the hospital on a reduced dose of antiepileptic medication and suffered what was thought to be an unwitnessed generalized tonic-clonic seizure, after which he claimed that his mood improved significantly and his suicidal ideas vanished. After discharge, intensive work was continued to help motivate Mr A, and a schedule was put in place for him to structure his day. Given his inadequate response to medications, Mr A was told that ECT would be an alternative intervention if he were to suffer a relapse. He consented to this treatment should it be needed.
Over the next 6 months, there was improvement in Mr A’s mood, and he then reduced his medications of his own volition. Four weeks later, Mr A’s mood worsened significantly, and he was taken to the hospital on the anniversary of his son’s death. At that point, his GAF score was 10 due to the persistent thoughts of self-harm and nondisclosure of plans. After discussion with Mr A and his partner about the risks and benefits of ECT, he consented to receiving bitemporal ECT.
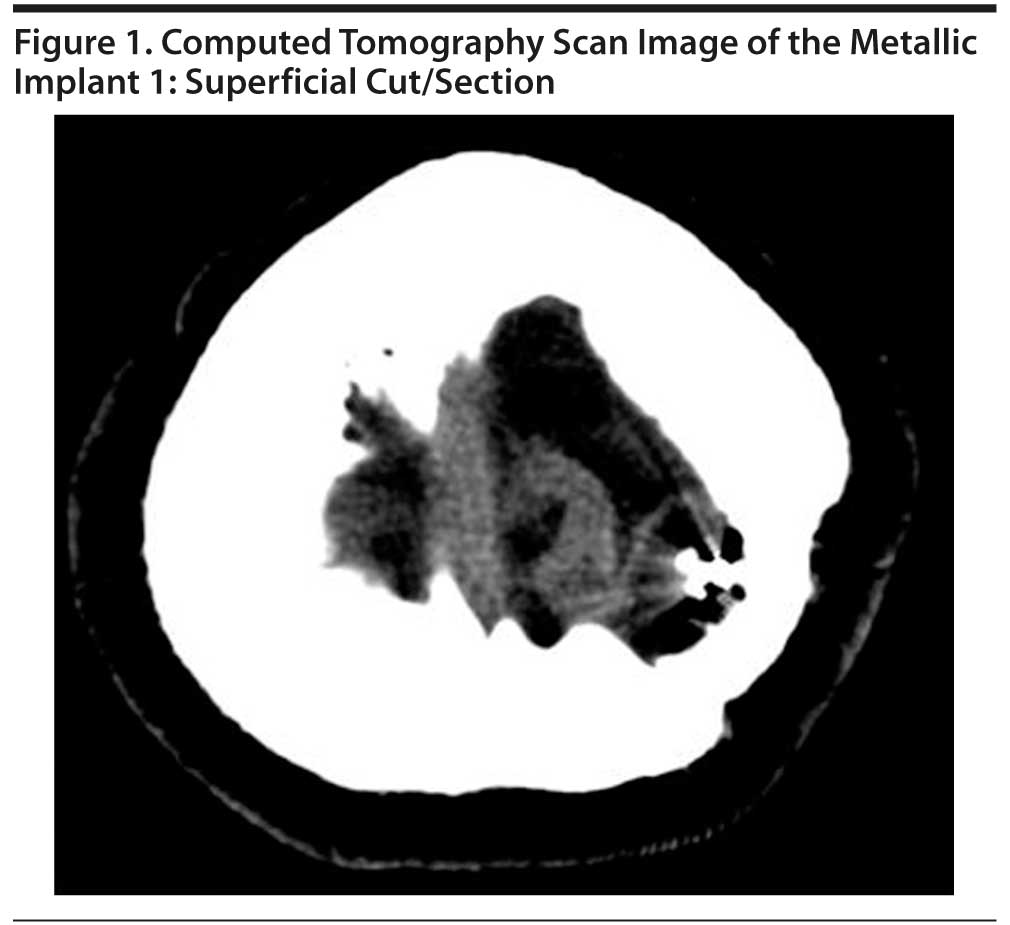
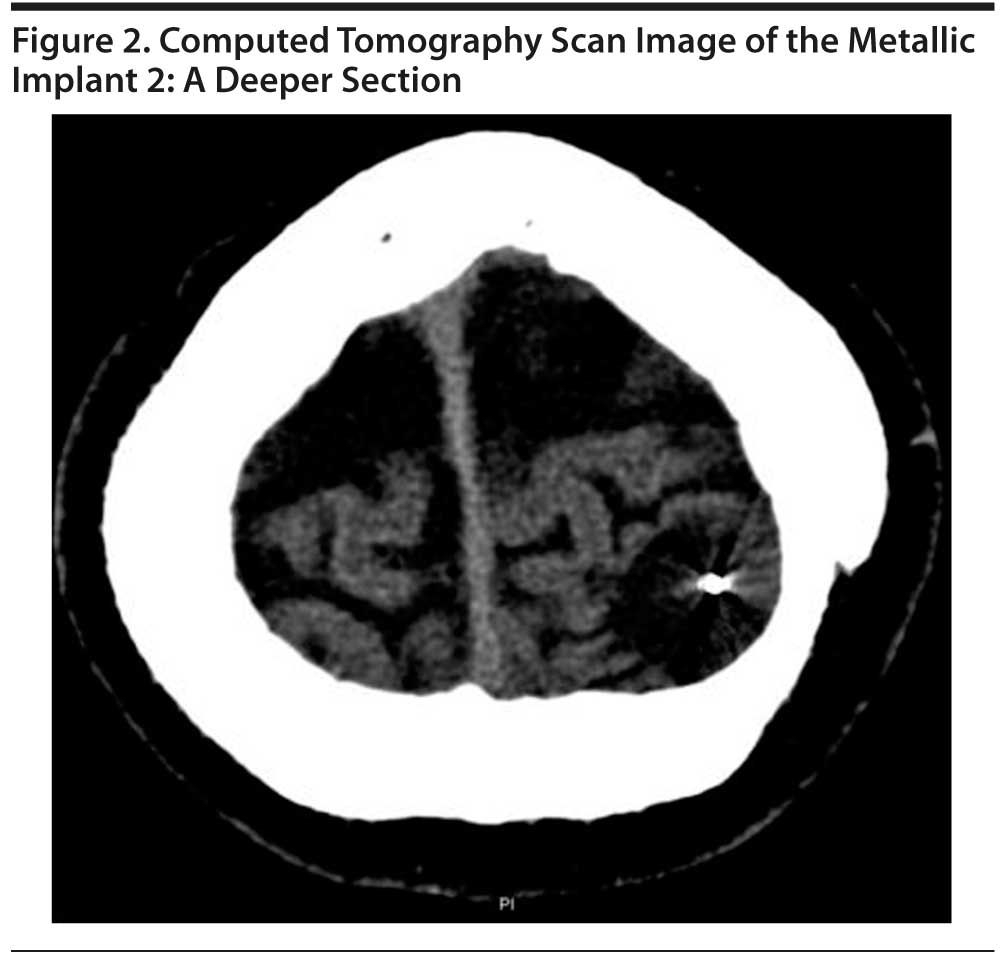
A computed tomography (CT) scan of the head was reviewed by the physician (S.A.) and the radiologist on the morning of the procedure to reconfirm the final electrode placement. Two pictures of the clip are presented in Figures 1 and 2. The figures show the object in the superficial slices. Although there was a skull defect, it was not deemed to be significant, and a bitemporal placement was chosen over ultra brief placement to reduce any chance of the clip heating up with the increased duration of current application associated with ultra brief placement. Application of unilateral placement would have meant closer proximity of both electrodes to the clip, thus increasing the likelihood of a loop forming by which the current would likely be shunted and thereby reducing the chances of inducing a seizure. With ECT stimulus parameters of current 800 mA, pulse width 1 ms, frequency 90 Hz, and duration 4 seconds, Mr A had a well-modified seizure of adequate duration. There were no concerns post-ECT, and the following day, significant improvements were seen in his condition: an absence of suicidal ideas, better energy levels, better sleep, and a renewed interest in activities. By the sixth ECT treatment, Mr A was showing sustained positive changes and a marked renewal of interest in interacting with staff and some of the others on the unit and wanting to “get back to living.” Over the next 2 ECT treatments, his subjective sadness reduced further, and a repeat Mini-Mental State Examination (MMSE)22 was performed to ensure that there was no memory loss. In total, Mr A received 8 ECT treatments and consistently scored 30/30 on the MMSE, with no forgetfulness or lapses in concentration.
At the time of discharge, Mr A was doing very well. Neuropsychological testing performed before and after ECT treatments and results are shown in Tables 2, 3, and 4.22-29 At review after discharge, Mr A displayed an interest in activities that he had been avoiding such as reading the paper and going into the garden. Prior to his admission, Mr A’s partner had rated him at 2/10 (10 equals well) on a visual analog scale, and at review, she rated him at 7/10. There were no hypomanic or manic features.
Mr A was advised maintenance ECT due to the severity of his depression and suicidal ideas. He had 15 ECT treatments as an outpatient. While the advice was for weekly and then biweekly treatments, due to transportation issues, Mr A had treatments initially weekly, then biweekly, and then monthly. On review at 1 year, following transfer to the outpatient psychiatrist, it was noted that Mr A was engaged in activities and feeling well with no concerns about depressive features and suicidal ideas or plans. He discontinued follow-up toward the 2-year follow-up period of his own volition, as he had to rely on a friend for the commute to receive outpatient ECT.
DISCUSSION
ECT is equal or superior to pharmacologic treatments in treatment-resistant depression.30 Previous studies have found that the incidence of depression for which the criteria for major depressive disorder were met ranges from 18%-61% in individuals with head injury.31 The role of ECT was addressed in a case series by Kant et al,12 and all patients showed improvement after ECT. The authors noted no adverse significant cognitive or physical sequelae.12 Concerns about the flow of current were addressed by Weaver et al,32 who studied current flow patterns and elucidated that the current density is highest beneath the electrodes and the areas close to the electrode axis. While bilateral ECT provides a more diffuse distribution of current, the current density is greatest along the anterior part of the electrode axis and in the frontal lobes. Cognitive tolerability has been addressed by Martino and colleagues,33 who examined the use of ECT in individuals with head injury who were responsive to antidepressants prior to the head injury but treatment refractory after the injury. The authors concluded that there were no concerns with regard to cognitive tolerability of ECT after head injury as evidenced by neuropsychological testing.33 Modern ventriculoperitoneal shunts use medical-grade silicone elastomers, and, therefore, electric conductance should not be a major concern. However, even with metallic components or content, ECT could also safely be used.
In summary, we advise the following before proceeding with ECT in patients with skull defects:
1. Complete a thorough history with full medication and physical health review;
2. Complete a CT scan of the head to confirm the existence of the implant (discussion with the radiologist may be helpful in deciding on electrode placement);
3. Discuss with the anesthetist the possibility of the need for restimulating if there are subthreshold seizures;
4. Map the planned electrode placement on the patient’s head;
5. Discuss with the patient and next of kin the advantages and disadvantages of the treatment and potential complications;
6. Complete baseline psychometric assessment and rating on the Hamilton Depression Rating Scale23,24 and MMSE22—alternatively the Montgomery-Asberg Depression Rating Scale34 or the Beck Depression Inventory35 could be used;
7. Place the electrodes as far away from the metallic implant as possible;
8. Consider that use of ultra brief stimuli and unilateral electrode placement may be an option in order to minimize cognitive deficits, but one will have to weigh issues such as increased duration of stimulus and potential heating of the clip and shunting of current;
9. Use of hyperventilation with oxygen or the administration of caffeine (pre-ECT) may be useful options;
10. Consider that the number of ECT treatments will depend on the severity of the depression and the response during the course of ECT (an average of 8-10 treatments seems to be adequate, with some patients going onto maintenance ECT); and
11. Conduct post-ECT reviews every 2 weeks for the first month by the psychiatrist and/or nurse in the community and repeat the MMSE and Hamilton Depression Rating Scale at each visit.
Implications
In the foreseeable future, head injuries will remain common, as will the associated mood disorders. The option of ECT will be an effective alternative in patients who have not responded to pharmacotherapy. Rapid advances in stroke interventions could mean an increased use of stents as a preventive mechanism in individuals at risk for cerebrovascular events, and ECT may become a common mode of intervention in those with severe treatment-resistant poststroke depression. The field of psychiatry will need to be prepared for this and other advances including deep-brain stimulation with intracranial “pacemakers.” The steps outlined above will be a helpful guide to the administration of ECT in patients with head injury and implants with severe depression and suicidal risk. Finally, it should be noted that cochlear implant manufacturers have cautioned against the use of ECT due to the risk of damaging the device,21 but the pros and cons of ECT will have to be weighed carefully in each case.
Drug names: carbamazepine (Carbatrol, Equetro, and others), clonazepam (Klonopin and others), lorazepam (Ativan and others), phenytoin (Dilantin, Phenytek, and others), risperidone (Risperdal and others), sertraline (Zoloft and others).
Author affiliations: Departments of Psychiatry (Drs Amanullah and Delva) and Medicine (Mr McRae), Dalhousie University, Halifax, Nova Scotia; and Departments of Psychiatry (Dr Amanullah) and Psychology (Dr Campbell), Hillsborough Hospital, and Queen Elizabeth Hospital (Ms Cole), Charlottetown, Prince Edward Island, Canada.
Potential conflicts of interest: Dr Amanullah has served on the speakers or advisory boards of Eli Lilly and Janssen. Drs Delva and Campbell, Mr McRae, and Ms Cole report no financial affiliations related to the subject of this article.
Funding/support: None reported.
Acknowledgments: The authors thank Kathy Lecky and Jacinta Keoughan for their work in ensuring that the document was in order. Mss Lecky and Keoughan are employees of Hillsborough Hospital, Charlottetown, Prince Edward Island, Canada, and report no conflicts of interest related to the subject of this article.
REFERENCES
1. Langois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2004.
2. Bushnik T, Englander J, Duong T. Medical and social issues related to posttraumatic seizures in persons with traumatic brain injury. J Head Trauma Rehabil. 2004;19(4):296-304. PubMed doi:10.1097/00001199-200407000-00004
3. Cifu DX, Kaelin DL, Wall BE. Deep venous thrombosis: incidence on admission to a brain injury rehabilitation program. Arch Phys Med Rehabil. 1996;77(11):1182-1185. PubMed doi:10.1016/S0003-9993(96)90145-8
4. Tsuang MT, Tidball JS, Geller D. ECT in a depressed patient with shunt in place for normal pressure hydrocephalus. Am J Psychiatry. 1979;136(9):1205-1206. PubMed
5. Jorge RE, Starkstein SE. Pathophysiologic aspects of major depression following traumatic brain injury. J Head Trauma Rehabil. 2005;20(6):475-487. PubMed doi:10.1097/00001199-200511000-00001
6. Young AW, Newcombe F, de Haan EH, et al. Face perception after brain injury: selective impairments affecting identity and expression. Brain. 1993;116(Pt 4):941-959. PubMed doi:10.1093/brain/116.4.941
7. Smith DH, Chen XH, Pierce JE, et al. Progressive atrophy and neuron death for one year following brain trauma in the rat. J Neurotrauma. 1997;14(10):715-727. PubMed doi:10.1089/neu.1997.14.715
8. Sidaros A, Skimminge A, Liptrot MG, et al. Long-term global and regional brain volume changes following severe traumatic brain injury: a longitudinal study with clinical correlates. Neuroimage. 2009;44(1):1-8. PubMed doi:10.1016/j.neuroimage.2008.08.030
9. NIH Consensus Development Panel on Rehabilitation of Persons With Traumatic Brain Injury. Consensus conference: rehabilitation of persons with traumatic brain injury. JAMA. 1999;282(10):974-983. PubMed doi:10.1001/jama.282.10.974
10. Saran AS. Depression after minor closed head injury: role of dexamethasone suppression test and antidepressants. J Clin Psychiatry. 1985;46(8):335-338. PubMed
11. Perino C, Rago R, Cicolini A, et al. Mood and behavioural disorders following traumatic brain injury: clinical evaluation and pharmacological management. Brain Inj. 2001;15(2):139-148. PubMed doi:10.1080/026990501458371
12. Kant R, Coffey CE, Bogyi AM. Safety and efficacy of ECT in patients with head injury: a case series. J Neuropsychiatry Clin Neurosci. 1999;11(1):32-37. PubMed
13. Madan S, Anderson K. ECT for a patient with a metallic skull plate. J ECT. 2001;17(4):289-291. PubMed doi:10.1097/00124509-200112000-00010
14. Dressler DM, Folk J. The treatment of depression with ECT in the presence of brain tumor. Am J Psychiatry. 1975;132(12):1320-1321. PubMed
15. Ruedrich SL, Chu CC, Moore SL. ECT for major depression in a patient with acute brain trauma. Am J Psychiatry. 1983;140(7):928-929. PubMed
16. Crow S, Meller W, Christenson G, et al. Use of ECT after brain injury. Convuls Ther. 1996;12(2):113-116. PubMed
17. Singh D, Morley S. Safety of electroconvulsive therapy in a patient with intracranial lead. Aust N Z J Psychiatry. 2008;42(12):1075-1076. PubMed
18. Clark AF, Davison K. Mania following head injury. A report of two cases and a review of the literature. Br J Psychiatry. 1987;150(6):841-844. PubMed doi:10.1192/bjp.150.6.841
19. Glezer A, Murray E, Price B, et al. Effective use of electroconvulsive therapy after craniofacial reconstructive surgery. J ECT. 2009;25(3):208-209. PubMed doi:10.1097/YCT.0b013e31818e2d5d
20. Hartmann SJ, Saldivia A. ECT in an elderly patient with skull defects and shrapnel. Convuls Ther. 1990;6(2):165-171. PubMed
21. Everman PD Jr, Kellner CH, Beale MD, et al. Modified electrode placement in patients with neurosurgical skull defects. J ECT. 1999;15(3):237-239. PubMed
22. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198. PubMed doi:10.1016/0022-3956(75)90026-6
23. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56-62. PubMed doi:10.1136/jnnp.23.1.56
24. McIntyre RS, Konarski JZ, Mancini DA, et al. Measuring the severity of depression and remission in primary care: validation of the HAMD-7 scale. CMAJ. 2005;173(11):1327-1334. PubMed doi:10.1503/cmaj.050786
25. Wechsler D. Wechsler Adult Intelligence Scale. 3rd ed. San Antonio, TX: The Psychological Cooperation; 1997.
26. Spreen O, Strauss E. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. 2nd ed. New York, NY: Oxford University Press; 1998.
27. Delis D, Kramer J, Kaplan E, et al. California Verbal Learning Test-Second Edition (CVLT-II) Manual. Sydney, Australia: The Psychological Cooperation, Harcourt Assessment, Inc; 1999.
28. Heaton KH, Chelune GJ, Talley JL, et al. Wisconsin Card Sorting Test: Computer Version 4 (WCST: CV4) Research Edition. Psychological Assessment Resources. San Antonio, Texas: Harcourt Assessment, Inc; 2003.
29. Rey Complex Figure Test and Recognition Trial: Professional Manual. Odessa, Florida: Psychological Assessment Resources, Inc; 1995.
30. Pagnin D, de Queiroz V, Pini S, et al. Efficacy of ECT in depression: a meta-analytic review. J ECT. 2004;20(1):13-20. PubMed doi:10.1097/00124509-200403000-00004
31. Kim E, Lauterbach EC, Reeve A, et al; ANPA Committee on Research. Neuropsychiatric complications of traumatic brain injury: a critical review of the literature (a report by the ANPA Committee on Research). J Neuropsychiatry Clin Neurosci. 2007;19(2):106-127. PubMed doi:10.1176/appi.neuropsych.19.2.106
32. Weaver L, Williams R, Rush S. Current density in bilateral and unilateral ECT. Biol Psychiatry. 1976;11(3):303-312. PubMed
33. Martino C, Krysko M, Petrides G, et al. Cognitive tolerability of electroconvulsive therapy in a patient with a history of traumatic brain injury. J ECT. 2008;24(1):92-95. PubMed doi:10.1097/YCT.0b013e31814faae5
34. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(4):382-389. PubMed doi:10.1192/bjp.134.4.382
35. Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893-897. PubMed doi:10.1037/0022-006X.56.6.893