Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Catatonia is a disorder of movement associated with cognitive, motor, and behavioral clinical signs and symptoms. The differential diagnosis of catatonia includes psychiatric and neurological conditions. We present a case of a man initially diagnosed with catatonia and treated with electroconvulsive therapy (ECT) who was referred for neuropsychiatric opinion following acute deterioration.
To the Editor: Catatonia is a disorder of movement associated with cognitive, motor, and behavioral clinical signs and symptoms.1 The differential diagnosis of catatonia includes psychiatric and neurological conditions. We present a case of a man initially diagnosed with catatonia and treated with electroconvulsive therapy (ECT) who was referred for neuropsychiatric opinion following acute deterioration. A diagnosis of Creutzfeldt-Jakob disease (CJD) was made on the basis of clinical and imaging findings.
Case report. Mr A, a 61-year-old male electrical engineer, presented to a psychiatrist in August 2014 with 2 weeks of confusion, word-finding difficulties, slurred speech, and right-hand clumsiness. Ten years previously, he had developed a delusion that his wife was having an affair. He was treated with paroxetine and olanzapine, which led to resolution of symptoms, but he was unable to return to full-capacity work despite remaining on long-term medication. His background medical and psychiatric history was otherwise unremarkable. There had been no recent infectious contacts.
Mr A was admitted to a neurology ward with a provisional diagnosis of posterior circulation stroke. Examination showed no focal signs. Brain computed tomography and magnetic resonance imaging (MRI) results were reported as normal. Findings of blood tests including viral serology, thyroid hormones, vitamin levels, and antineuronal autoantibodies were negative. Provisional diagnoses of an adjustment or conversion disorder were suggested, and Mr A was discharged to his psychiatrist.
The patient’s wife noted continued deterioration over a fortnight, with difficulty communicating and following commands, groaning, upper limb posturing, and apraxia. He was readmitted to the hospital, but repeated examination, neurology review, and blood test results were unremarkable. On the basis of the presentation and history of psychosis, the patient was diagnosed with an atypical catatonic relapse and received 4 treatments of ECT. He continued to deteriorate, becoming dehydrated and tachycardic, with myoclonic jerks. He was referred for specialist neuropsychiatric opinion.
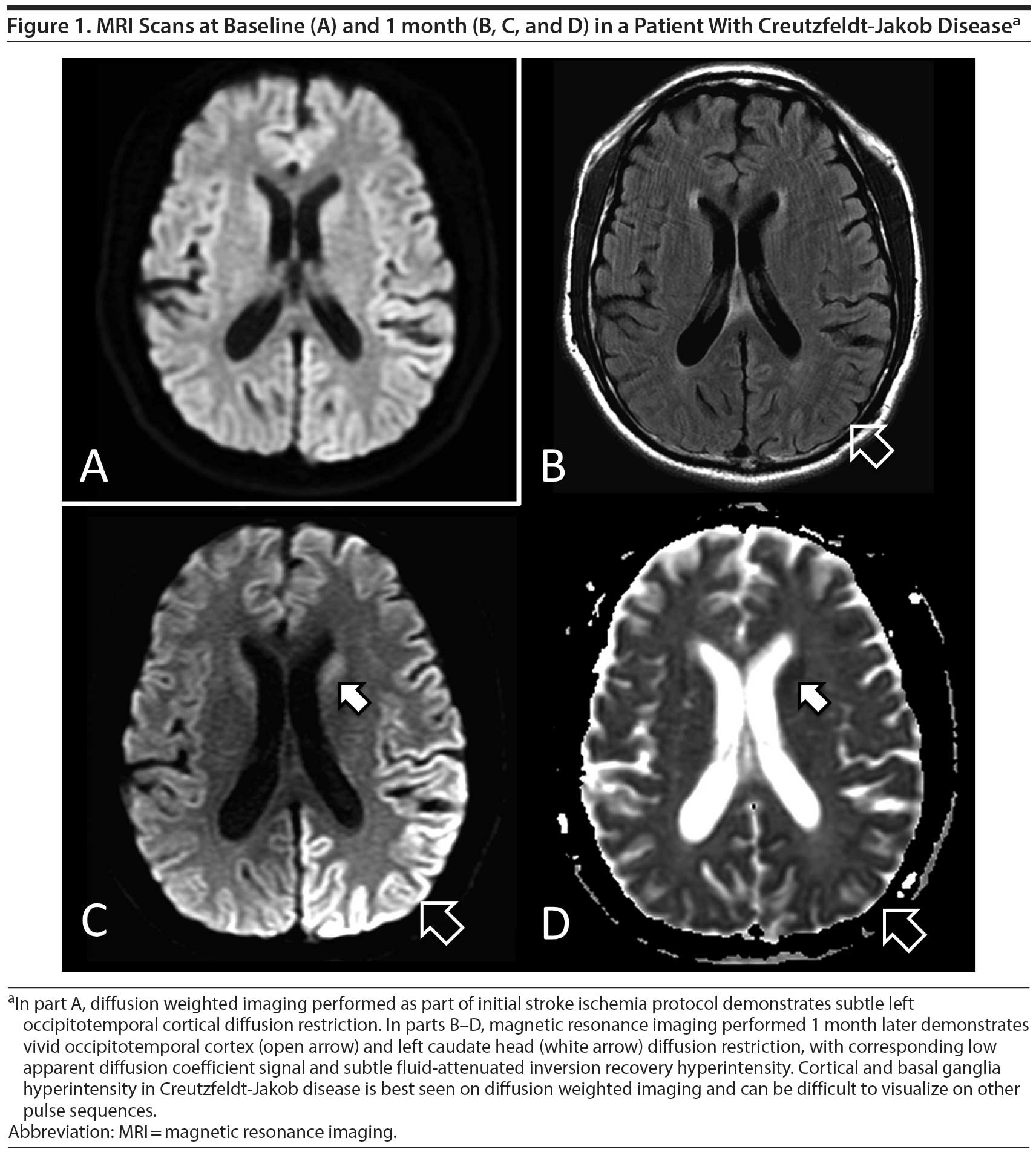
A neuropsychiatric review identified subtle abnormalities on Mr A’s previous MRI scan suggestive of CJD (Figure 1A). He deteriorated further, with more frequent myoclonic jerks and reduced conscious state. A second MRI scan showed characteristic signs of sporadic CJD (Figure 1C and Figure 1D). An electroencephalogram (EEG) showed generalized slowing but no periodic complexes or epileptiform discharges, and cerebrospinal fluid (CSF) 14-3-3 protein was positive. The patient was discharged to palliative care with a diagnosis of sporadic CJD and died 4 weeks later. An autopsy confirmed CJD, with spongiform encephalopathy, neuronal loss, and gliosis in cerebral, basal ganglia, cerebellar cortex, and brain stem sections, with patchy prion protein immunoreactivity in both a synaptic and focally granular pattern.
CJD, the commonest prion disease, occurs at a rate of around 1 in 1 million per year.2 Ninety percent of cases are sporadic (sCJD), 10% are familial, and less than 1% are iatrogenic or variant CJD. The typical clinical presentation is of a rapid cognitive deterioration with myoclonic jerks. Centers for Disease Control and Prevention criteria for probable sCJD require rapidly progressive dementia with 2 or more of the following: myoclonus, visual or cerebellar symptoms, pyramidal or extrapyramidal symptoms, or akinetic mutism, along with 1 or more positive findings on EEG (periodic sharp wave complexes), CSF (positive 14-3-3 protein), or MRI.1 Psychiatric symptoms including mood disturbance, behavioral disturbance, or psychosis may feature early in younger patients.3 Promising new tests with high sensitivity and specificity using CSF,4 nasal brushings (sCJD),5 or urine (variant CJD)6 have been recently described.
Imaging findings in CJD, particularly on diffusion weighted imaging (DWI) MRI sequences, are more sensitive than either EEG or CSF and may precede pathognomonic clinical features such as myoclonic jerks. Restricted diffusion on DWI in the basal ganglia, thalamus, or the cortex (“cortical ribbon sign,” Figure 1A-1D) is a classic finding early on, thought to result from a number of histopathological factors: vacuolation, accumulation of prion protein, and reactive gliosis.7 Although similar changes can be appreciated on T2, fluid-attenuated inversion recovery, and proton density sequences, these tests are far less sensitive, and the findings may be normal in a large proportion of patients.8 Later in the course of the disease, changes are more pronounced, leading to more widespread involvement and generalized atrophy.8
In summary, the patient’s history of psychosis together with apparently normal neurologic testing and investigations initially masked the underlying diagnosis. The presentation of a rapidly progressive mental deterioration with neurologic features should trigger consideration of a diagnosis of CJD and investigations including EEG, lumbar puncture, and DWI MRI.
aNeuropsychiatry Unit, Royal Melbourne Hospital, Parkville, Australia
bDepartment Consultation and Liaison Psychiatry, Sunshine Hospital, Sunshine, Australia
cDepartment of Radiology, Royal Melbourne Hospital, Parkville, Australia
dMelbourne Neuropsychiatry Centre, University of Melbourne and Melbourne Health, Parkville, Australia
Potential conflicts of interest: None reported.
Funding/support: None reported.
J Clin Psychiatry 2016;77(7):e900-e901
dx.doi.org/10.4088/JCP.15cr09951
© Copyright 2016 Physicians Postgraduate Press, Inc.
References
1. Wijemanne S, Jankovic J. Movement disorders in catatonia. J Neurol Neurosurg Psychiatry. 2015;86(8):825-832. PubMed doi:10.1136/jnnp-2014-309098
2. Centers for Disease Control and Prevention. Creutzfeldt-Jakob Disease, Classic (CJD). CDC Web site. http://www.cdc.gov/prions/cjd/index.html. Updated February 6, 2015.
3. Thompson A, MacKay A, Rudge P, et al. Behavioral and psychiatric symptoms in prion disease. Am J Psychiatry. 2014;171(3):265-274. PubMed doi:10.1176/appi.ajp.2013.12111460
4. Atarashi R, Satoh K, Sano K, et al. Ultrasensitive human prion detection in cerebrospinal fluid by real-time quaking-induced conversion. Nat Med. 2011;17(2):175-178. PubMed
5. Orrú CD, Bongianni M, Tonoli G, et al. A test for Creutzfeldt-Jakob disease using nasal brushings. N Engl J Med. 2014;371(6):519-529. doi:10.1056/NEJMoa1315200PubMed doi:10.1038/nm.2294
6. Moda F, Gambetti P, Notari S, et al. Prions in the urine of patients with variant Creutzfeldt-Jakob disease. N Engl J Med. 2014;371(6):530-539. PubMed doi:10.1056/NEJMoa1404401
7. Geschwind MD, Potter CA, Sattavat M, et al. Correlating DWI MRI with pathologic and other features of Jakob-Creutzfeldt disease. Alzheimer Dis Assoc Disord. 2009;23(1):82-87. PubMed doi:10.1097/WAD.0b013e31818323ef
8. Kallenberg K, Schulz-Schaeffer WJ, Jastrow U, et al. Creutzfeldt-Jakob disease: comparative analysis of MR imaging sequences. AJNR Am J Neuroradiol. 2006;27(7):1459-1462. PubMed
This PDF is free for all visitors!