SPRAVATO® (esketamine) CIII Nasal Spray:
The First and Only N-Methyl D-Aspartate (NMDA) Receptor Antagonist Approved in Conjunction With an Oral Antidepressant for the Treatment of Adults With Treatment-Resistant Depression
Information From Industry
INDICATIONS AND USAGE
SPRAVATO® (esketamine) CIII Nasal Spray is indicated, in conjunction with an oral antidepressant, for the treatment of treatment-resistant depression (TRD) in adults.
Limitations of Use:
- The effectiveness of SPRAVATO® in preventing suicide or in reducing suicidal ideation or behavior has not been demonstrated. Use of SPRAVATO® does not preclude the need for hospitalization if clinically warranted, even if patients experience improvement after an initial dose of SPRAVATO®.
- SPRAVATO® is not approved as an anesthetic agent. The safety and effectiveness of SPRAVATO® as an anesthetic agent have not been established.
Important Safety Information
WARNING: SEDATION, DISSOCIATION; ABUSE AND MISUSE; and SUICIDAL THOUGHTS AND BEHAVIORS
See full prescribing information for complete boxed warning
- Risk for sedation and dissociation after administration. Monitor patients for at least two hours after administration (5.1, 5.2).
- Potential for abuse and misuse. Consider the risks and benefits of using SPRAVATO® prior to use in patients at higher risk of abuse. Monitor for signs and symptoms of abuse and misuse (5.3).
- SPRAVATO® is only available through a restricted program called the SPRAVATO® REMS (5.4).
- Increased risk of suicidal thoughts and behaviors in pediatric and young adult patients taking antidepressants. Closely monitor all antidepressant-treated patients for clinical worsening and emergence of suicidal thoughts and behaviors. SPRAVATO® is not approved for use in pediatric patients (5.5).
Please see additional Important Safety Information later in this article and full Prescribing Information, including Boxed WARNINGS, and Medication Guide for SPRAVATO®.
Significant Unmet Need for Patients with TRD
For decades, pharmacologic treatments for major depressive disorder (MDD) have focused on modulating the level of monoamine neurotransmitters in the brain.1 While antidepressants (ADs) have helped most patients with MDD, the landmark STAR*D trial2 found one-third of patients did not achieve remission by the third line of therapy.3 Remission rates were progressively lower in each subsequent therapy line and only 14% of patients achieved remission after the third line of therapy.3
For those with TRD, some patients may benefit from treatment with a different kind of medication.1,3 TRD may be defined as failure to respond to two or more antidepressants of adequate dose and duration in the current depressive episode.1,4
An option for adults with TRD is SPRAVATO® (esketamine) CIII Nasal Spray, the first and only NMDA receptor antagonist approved in conjunction with an oral AD for adults with TRD.5
THE FIRST NMDA Receptor Antagonist APPROVED FOR TRD
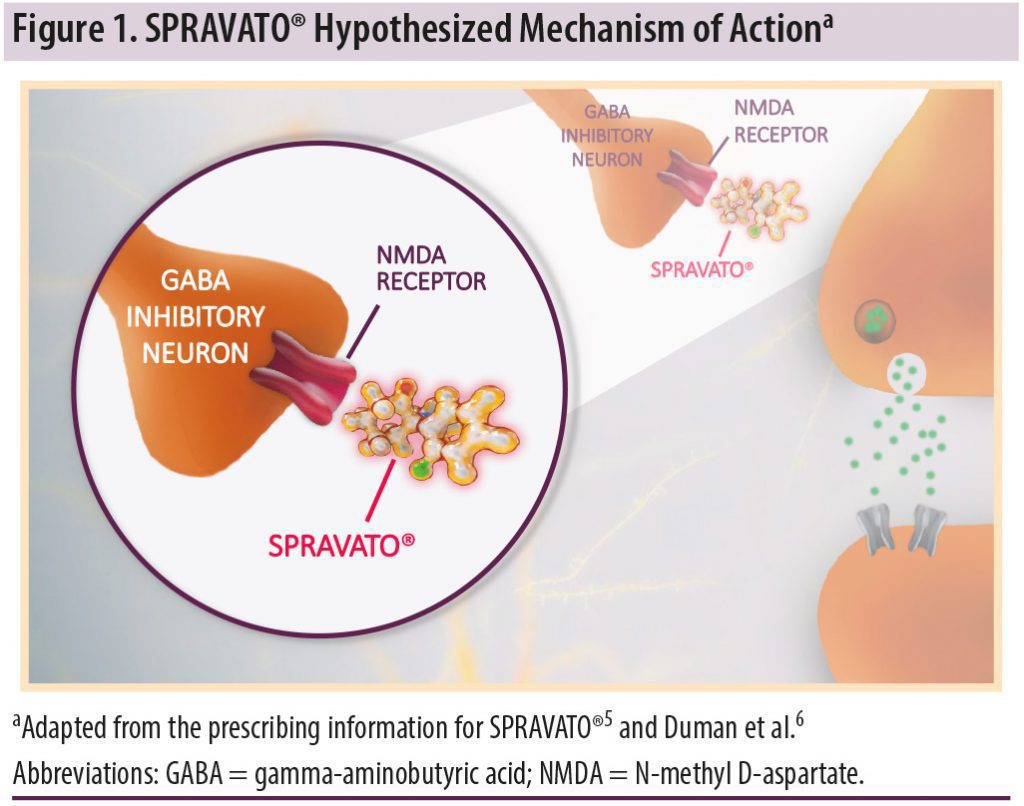
SPRAVATO®, the S-enantiomer of racemic ketamine, is the first and only treatment (in conjunction with an oral AD) formulated for nasal spray use in TRD (Figure 1).5 The mechanism by which it exerts its antidepressant effect is unknown.5
Clinical Program Overview
SPRAVATO® (esketamine) CIII Nasal Spray was evaluated for safety in more than 1700 adult patients with TRD.4 This program consisted of 5 phase 3 studies (3 short-term and 2 long-term) and 1 phase 2 study.5
Study 1 and Study 2 evaluated the efficacy and safety of SPRAVATO® plus a newly initiated oral AD in comparison to placebo nasal spray plus oral AD.7,8 In Study 1:
- The patients were moderately to severely depressed with a mean baseline Montgomery-Åsberg Depression Rating Scale* (MADRS) score of 376,9
- A third of patients reported a history of suicidal ideation10,†
*MADRS is a 10-item, clinician-rated scale used to assess severity of depressive symptoms. Scores on MADRS range from 0 to 60, with higher scores indicating more severe depression.
†Observed at screening during Study 1. Patients with intent to act or recent suicidal behavior were excluded from the study.8
Short-Term Efficacy—Superior Improvement at Week 4
Study 1,7 was a pivotal phase 3, short-term (4-week), randomized, placebo-controlled, double-blind, multicenter trial in which the primary endpoint was change in MADRS score from baseline to day 28.7 Patients in both treatment arms were discontinued from their current oral AD to which they had previously not responded and initiated a new oral AD (Figure 2).7 The efficacy analyses included 223 adult patients randomized to receive flexible dosing of SPRAVATO® 56 mg or 84 mg plus an oral AD vs placebo nasal spray plus oral AD.7 SPRAVATO® plus an oral AD achieved superior improvement in depression symptoms vs placebo nasal spray plus and oral AD at Day 28. LS mean (SE) change in MADRS score: –19.8 in the SPRAVATO group vs –15.8 in the placebo group at Week 4 (P =.020).5
- Most of the treatment difference between SPRAVATO® and placebo was observed at 24 hours5
- Between 24 hours and Day 28, both SPRAVATO® and placebo groups continued to improve5
- The difference between the groups generally remained but did not appear to increase over time through Day 285
Long-Term Efficacy—Significantly Delayed Time to Relapse
Study 28 was a long-term, randomized, double-blind, multicenter, controlled, maintenance-of-effect study conducted in adult patients with TRD who had achieved stable remission or stable response after 16 weeks of SPRAVATO® plus oral AD (induction and optimization phases).8 The primary endpoint was time to relapse during the maintenance phase among stable remitters (Figure 3).8
Stable remitters who continued treatment with SPRAVATO® plus oral AD:
- Demonstrated statistically significant superiority in delayed time to relapse (P = .003)8
- Were 51% less likely to relapse5
The study also showed that patients who were stable responders to SPRAVATO® plus an oral AD and continued treatment were 70% less likely to relapse than patients who switched to placebo nasal spray plus oral AD during the maintenance phase (Figure 4).5 Additionally, time to relapse was significantly delayed in stable responders (2-sided P = .001).8
- Stable remission was defined as MADRS total score ≤12 at least 3 of the last 4 weeks of the optimization phase5
- Stable response was defined as ≥50% reduction in the MADRS total score from baseline in each of the last 2 weeks of the optimization phase but not meeting criteria for stable remission5,8
- Stable remitters and stable responders were not overlapping groups8
- Relapse was defined as a MADRS total score of ≥22 for 2 consecutive weeks and/or hospitalization for worsening depression, or any other clinically relevant event determined per clinical judgment to be suggestive of a relapse of depressive symptoms5
Safety and Tolerability
Table 1 lists the adverse reactions occurring in 2% or more of patients treated with SPRAVATO® plus oral AD at any dose and at a greater rate than patients treated with placebo nasal spray plus oral AD in short-term studies.
Important Safety Information (continued)
Contraindications.
SPRAVATO® is contraindicated in patients with:
- Aneurysmal vascular disease (including thoracic and abdominal aorta, intracranial and peripheral arterial vessels) or arteriovenous malformation5
- History of intracerebral hemorrhage5
- Hypersensitivity to esketamine, ketamine, or any of the excipients5
Sedation.
- In clinical trials, 48% to 61% of SPRAVATO®-treated patients developed sedation, and 0.3% to 0.4% of SPRAVATO®-treated patients experienced loss of consciousness.5
- Because of the possibility of delayed or prolonged sedation, patients must be monitored by a healthcare provider for at least 2 hours at each treatment session, followed by an assessment to determine when the patient is considered clinically stable and ready to leave the healthcare setting.5
- Closely monitor for sedation with concomitant use of SPRAVATO® with CNS depressants (e.g., benzodiazepines, opioids, alcohol).5
Dissociation.
- The most common psychological effects of SPRAVATO® were dissociative or perceptual changes (including distortion of time, space and illusions), derealization and depersonalization (61% to 84% of SPRAVATO®-treated patients developed dissociative or perceptual changes). Given its potential to induce dissociative effects, carefully assess patients with psychosis before administering SPRAVATO®; treatment should be initiated only if the benefit outweighs the risk.5
- Because of the risks of dissociation, patients must be monitored by a healthcare provider for at least 2 hours at each treatment session, followed by an assessment to determine when the patient is considered clinically stable and ready to leave the healthcare setting.5
Abuse and misuse.
- SPRAVATO® contains esketamine, a Schedule III controlled substance (CIII), and may be subject to abuse and diversion. Assess each patient’s risk for abuse or misuse prior to prescribing and monitor all patients for the development of these behaviors or conditions, including drug-seeking behavior, while on therapy. Individuals with a history of drug abuse or dependence are at greater risk; therefore, use careful consideration prior to treatment of individuals with a history of substance abuse disorder and monitor for signs of abuse or dependence.5
SPRAVATO® Risk Evaluation and Mitigation Strategy (REMS).
- SPRAVATO® is available only through a restricted program called the SPRAVATO® REMS because of the risks of serious adverse outcomes from sedation, dissociation, and abuse and misuse.5
- Important requirements of the SPRAVATO® REMS include the following:
- Healthcare settings must be certified in the program and ensure that SPRAVATO® is5:
- Only dispensed and administered in healthcare settings.5
- Patients treated in outpatient settings (e.g., medical offices and clinics) must be enrolled in the program.5
- Administered by patients under the direct observation of a healthcare provider and that patients are monitored by a healthcare provider for at least 2 hours after administration of SPRAVATO®.5
- Pharmacies must be certified in the REMS and must only dispense SPRAVATO® to healthcare settings that are certified in the program.5
- Healthcare settings must be certified in the program and ensure that SPRAVATO® is5:
- Further information, including a list of certified pharmacies, is available at SPRAVATOrems.com or 1-855-382-6022.5
Suicidal Thoughts and Behaviors in Adolescents and Young Adults.
- In pooled analyses of placebo-controlled trials of antidepressant drugs (SSRIs and other antidepressant classes) that included adult and pediatric patients, the incidence of suicidal thoughts and behaviors in patients age 24 years and younger was greater than in placebo-treated patients. SPRAVATO® is not approved in pediatric (<18 years of age) patients.5
- There was considerable variation in risk of suicidal thoughts and behaviors among drugs, but there was an increased risk identified in young patients for most drugs studied.5
- Monitor all antidepressant-treated patients for clinical worsening and emergence of suicidal thoughts and behaviors, especially during the initial few months of drug therapy and at times of dosage changes. Counsel family members or caregivers of patients to monitor for changes in behavior and to alert the healthcare provider. Consider changing the therapeutic regimen, including possibly discontinuing SPRAVATO® and/or the concomitant oral antidepressant, in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.5
Increase in Blood Pressure.
- SPRAVATO® causes increases in systolic and/or diastolic blood pressure (BP) at all recommended doses. Increases in BP peak approximately 40 minutes after SPRAVATO® administration and last approximately 4 hours.5
- Approximately 8% to 19% of SPRAVATO®-treated patients experienced an increase of more than 40 mmHg in systolic BP and/or 25 mmHg in diastolic BP in the first 1.5 hours after administration at least once during the first 4 weeks of treatment. A substantial increase in blood pressure could occur after any dose administered even if smaller blood pressure effects were observed with previous administrations. SPRAVATO® is contraindicated in patients for whom an increase in BP or intracranial pressure poses a serious risk (e.g., aneurysmal vascular disease, arteriovenous malformation, history of intracerebral hemorrhage). Before prescribing SPRAVATO®, patients with other cardiovascular and cerebrovascular conditions should be carefully assessed to determine whether the potential benefits of SPRAVATO® outweigh its risk.5
- Assess BP prior to administration of SPRAVATO®. In patients whose BP is elevated prior to SPRAVATO® administration (as a general guide: >140/90 mmHg), a decision to delay SPRAVATO® therapy should take into account the balance of benefit and risk in individual patients.5
- BP should be monitored for at least 2 hours after SPRAVATO® administration. Measure blood pressure around 40 minutes post-dose and subsequently as clinically warranted until values decline. If BP remains high, promptly seek assistance from practitioners experienced in BP management. Refer patients experiencing symptoms of a hypertensive crisis (e.g., chest pain, shortness of breath) or hypertensive encephalopathy (e.g., sudden severe headache, visual disturbances, seizures, diminished consciousness, or focal neurological deficits) immediately for emergency care.5
- Closely monitor blood pressure with concomitant use of SPRAVATO® with psychostimulants (e.g., amphetamines, methylphenidate, modafinil, armodafinil) or monoamine oxidase inhibitors (MAOIs).5
- In patients with a history of hypertensive encephalopathy, more intensive monitoring, including more frequent blood pressure and symptom assessment, is warranted because these patients are at increased risk for developing encephalopathy with even small increases in blood pressure.5
Please see additional Important Safety Information later in this article and full Prescribing Information, including Boxed WARNINGS, and Medication Guide for SPRAVATO®.
 Test Your Knowledge Question
Test Your Knowledge Question
Discontinuation Rates Due to Adverse Reactions Were Less Than 5% Across the 2 Pivotal Short- and Long-Term Clinical Trials5,‡,§
In 2 short-term studies in adults <65 years old, 4.6% of adults treated with SPRAVATO® plus oral AD discontinued treatment vs 1.4% of patients who received placebo nasal spray plus oral AD (Figure 5).5
Across all phase 3 studies, adverse reactions leading to discontinuation were5:
- Anxiety (1.2%)
- Depression (0.9%)
- Blood pressure increased (0.6%)
- Dizziness (0.6%)
- Suicidal ideation (0.5%)
- Dissociation (0.4%)
- Nausea (0.4%)
- Vomiting (0.4%)
- Headache (0.3%)
- Muscular weakness (0.3%)
- Vertigo (0.2%)
- Hypertension (0.2%)
- Panic attack (0.2%)
- Sedation (0.2%)
‡Induction phase only for Study 1 and a second similar 4-week study.7
§Maintenance phase only for Study 2.8
Dosing Schedule

SPRAVATO® (esketamine) CIII Nasal Spray does not require daily dosing and should be administered in conjunction with an oral AD.5 SPRAVATO® is patient-administered with a single-use device that delivers a total of 28 mg of SPRAVATO® in 2 sprays (1 spray per nostril) with each device. SPRAVATO® is self-administered using 2 devices (for a 56-mg dose) or 3 devices (for an 84-mg dose), depending on the dose prescribed, with a 5-minute rest between use of each device to allow medication to absorb.5
- The recommended treatment schedule for SPRAVATO® (esketamine) CIII Nasal Spray is divided into 2 phases: the induction phase and the maintenance phase5
- SPRAVATO® is administered twice weekly during the induction phase. The recommended administration during this 4-week phase is a 56-mg dose on Day 1 with subsequent doses of 56 mg or 84 mg based on clinical judgment5
- Evidence of therapeutic benefit should be evaluated at the end of the induction phase to determine need for continued treatment5
- In the subsequent maintenance phase, the recommended dose is 56 or 84 mg once weekly from weeks 5 to 8, and then 56 or 84 mg every 2 weeks or once weekly5
- Dosing frequency should be individualized to the lowest frequency needed to maintain remission/response5
Important Safety Information (continued)
Cognitive Impairment.
Short-Term Cognitive Impairment. In a study in healthy volunteers, a single dose of SPRAVATO® caused cognitive performance decline 40 minutes post-dose. Compared to placebo-treated subjects, SPRAVATO®-treated subjects required a greater effort to complete the cognitive tests at 40 minutes post-dose. Cognitive performance and mental effort were comparable between SPRAVATO® and placebo at 2 hours post-dose. Sleepiness was comparable after 4 hours post-dose.
Long-Term Cognitive Impairment. Long-term cognitive and memory impairment have been reported with repeated ketamine misuse or abuse. No adverse effects of SPRAVATO® nasal spray on cognitive functioning were observed in a one-year open-label safety study; however, the long-term cognitive effects of SPRAVATO® have not been evaluated beyond one year.
Impaired Ability to Drive and Operate Machinery.
- Before SPRAVATO® administration, instruct patients not to engage in potentially hazardous activities requiring complete mental alertness and motor coordination, such as driving a motor vehicle or operating machinery, until the next day following a restful sleep. Patients will need to arrange transportation home following treatment with SPRAVATO®.
Ulcerative or Interstitial Cystitis.
- Cases of ulcerative or interstitial cystitis have been reported in individuals with long-term off-label use or misuse/abuse of ketamine. In clinical studies with SPRAVATO® nasal spray, there was a higher rate of lower urinary tract symptoms (pollakiuria, dysuria, micturition urgency, nocturia, and cystitis) in SPRAVATO®-treated patients than in placebo-treated patients. No cases of esketamine-related interstitial cystitis were observed in any of the studies, which involved treatment for up to a year.
- Monitor for urinary tract and bladder symptoms during the course of treatment with SPRAVATO® and refer to an appropriate healthcare provider as clinically warranted.
Pregnancy, Embryo-Fetal Toxicity, and Lactation
- SPRAVATO® is not recommended during pregnancy. SPRAVATO® may cause fetal harm when administered to pregnant women. Advise pregnant women of the potential risk to an infant exposed to SPRAVATO® in utero. Advise women of reproductive potential to consider pregnancy planning and prevention.
- There are risks to the mother associated with untreated depression in pregnancy. If a woman becomes pregnant while being treated with SPRAVATO®, treatment with SPRAVATO® should be discontinued and the patient should be counseled about the potential risk to the fetus.
- Pregnancy Exposure Registry: There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antidepressants, including SPRAVATO®, during pregnancy. Healthcare providers are encouraged to register patients by contacting the National Pregnancy Registry for Antidepressants at 1-844-405-6185 or online at https://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/antidepressants/.
- SPRAVATO® is present in human Because of the potential for neurotoxicity, advise patients that breastfeeding is not recommended during treatment with SPRAVATO®.
Select Use In Specific Populations
Geriatric Use.
- No overall differences in the safety profile were observed between patients 65 years of age and older and patients younger than 65 years of age. At the end of a 4-week, randomized, double-blind study, there was no statistically significant difference between groups on the primary efficacy endpoint.
Hepatic Impairment.
- SPRAVATO®-treated patients with moderate hepatic impairment may need to be monitored for adverse reactions for a longer period of time.
- SPRAVATO® has not been studied in patients with severe hepatic impairment (Child-Pugh class C). Use in this population is not recommended.
Adverse Reactions
- The most common adverse reactions with SPRAVATO® plus oral antidepressant (incidence ≥5% and at least twice that of placebo nasal spray plus oral antidepressant) were:
- TRD: dissociation, dizziness, nausea, sedation, vertigo, hypoesthesia, anxiety, lethargy, blood pressure increased, vomiting, and feeling drunk.
Please see full Prescribing Information, including Boxed WARNINGS, and Medication Guide for SPRAVATO®.
Become a Certified SPRAVATO® Treatment Center
Practices interested in becoming a certified SPRAVATO® (esketamine) CIII Nasal Spray treatment center11 should evaluate the following requirements and considerations:
- Handling and storage of Schedule III products
- Space requirements for self-administration and monitoring
- Staff and equipment for post-administration monitoring
- Ability and capacity for scheduling frequent appointments
- Controlled distribution network
- Insurance benefits investigation and reimbursement management
Certified SPRAVATO® treatment centers must comply with full SPRAVATO® REMS requirements, which can be obtained at www.spravatorems.com or by calling 855-382-6022.
Locate a Certified SPRAVATO® Treatment Center
To locate a certified SPRAVATO® treatment center, visit www.spravatohcp.com/findacenter, or call Janssen CarePath at 844-777-2828.
Conclusions
SPRAVATO® is the first and only NMDA receptor antagonist approved, in conjunction with an oral AD, for TRD in adults. It is for adults who have not responded adequately to at least 2 oral ADs of adequate dose and duration in their current depressive episode.
SPRAVATO® plus an oral AD demonstrated statistically superior improvement in depression symptoms after 4 weeks compared to placebo plus oral AD, based on the short-term study.5 In the long-term maintenance study, SPRAVATO® significantly delayed time to relapse in patients who were stable remitters on SPRAVATO®.5
SPRAVATO® demonstrated safety in short- and long-term studies conducted in more than 1700 adult patients with TRD.5 SPRAVATO® has Boxed WARNINGS for sedation, dissociation, abuse and misuse, and suicidal thoughts and behaviors – see full Boxed WARNINGS in the SPRAVATO® full Prescribing Information.
For information on how to become a certified
SPRAVATO® treatment center, please visit
spravatotreatmentcenter.com
REFERENCES
- Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1–21. PubMed CrossRef
- Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Study. National Institute of Mental Health website. https://www.nimh.nih.gov/funding/clinical-research/practical/stard/index.shtml. Accessed March 6, 2019.
- Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–1917. PubMed CrossRef
- Gaynes BN, Asher GA, Gartlehner G, et al. Definition of Treatment-Resistant Depression in the Medicare Population. Rockville, MD: Agency for Healthcare Research and Equality (US); 2018. PubMed
- SPRAVATO® (esketamine) CIII Nasal Spray [prescribing information]. Titusville, NJ: Janssen Pharmaceuticals, Inc; 2020.
- Duman RS, Adhajanian GK, Sanacora G, et al. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(3):238–249. PubMed CrossRef
- Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428–438. PubMed CrossRef
- Daly EJ, Trivedi M, Janik A, et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2019;76(9):893–903. PubMed CrossRef
- Cusin C, Yang H, Yeung A, et al. Rating scales for depression. In: Baer L, Blais MA, eds. Handbook of Clinical Rating Scales and Assessment in Psychiatry and Mental Health. New York, NY: Humana Press; 2010:7–35.
- Data on file. Janssen Pharmaceuticals, Inc, Titusville, NJ.
- Janssen Pharmaceuticals, Inc. SPRAVATO® Treatment Center. https://www.spravatotreatmentcenter.com. April 2019.
October 2021 cp-158049v3