ABSTRACT
Sedentary behaviors are leisurely behaviors that occur during waking hours performed while lying down or seated; examples are relaxing, conversing, using a smartphone, watching television, traveling in private or public transport, and thinking or working at a desk. Sedentary behaviors are common in everyday life; the average person spends 9–10 h/d sedentary. Findings from meta-analyses show that higher levels of physical activity are associated with a reduced risk of dementia and that near-absence of moderate to vigorous physical activity is associated with an increased risk of dementia. Sedentariness is a clearly defined construct that is more than just low levels of physical activity. Sedentariness, therefore, merits independent study. In this context, a recent cohort study, conducted in elderly subjects (mean age, 67 years) who were followed for a mean of 6.7 years, found that sedentariness, independent of current levels of moderate to vigorous physical activity, was associated in a dose-dependent fashion with the risk of incident dementia; the finding held true when reverse causation was addressed through the exclusion of subjects who developed dementia within 4 years of follow-up. The adjusted 10-year risk of dementia rose from about 8% with sedentariness at 10 h/d to about 23% with sedentariness at 15 h/d; the difference is clinically meaningful. Limitations of studies in the field are that residual confounding cannot be excluded, and that no randomized controlled trials exist upon which guidance may be based. Nevertheless, it could be prudent to decrease sedentary behaviors if only because these have also been associated with other adverse physical and mental health outcomes. Additional subjects explained in this article include reverse causation and how it may be dealt with during research design and data analysis, individual participant data meta-analysis, and making sense of results that are reported in terms of “per 1,000 person-years.”
J Clin Psychiatry 2024;85(1):24f15270
Author affiliations are listed at the end of this article.
One metabolic equivalent (MET) is the energy expenditure of a person who is seated and at rest, and sedentary behaviors are waking hours behaviors with an energy expenditure that is < 1.5 METs. Examples of sedentary behaviors are all leisurely behaviors that are performed while lying down or seated. Such behaviors include lazing, chatting, using a smartphone, watching television, using a laptop, commuting in private or public transport, and thinking or working at a desk. As is immediately apparent, these behaviors are common in everyday life; consequently, the average person is sedentary for 9–10 h/d.1
Many studies have shown that, independent of engagement in health-related physical activity, greater sedentary time is associated with higher risks of adverse physical and mental health outcomes. The previous article in this column presented an overview on sedentariness and its possible effects on physical and mental health.1 This article specifically examines associations between sedentariness and dementia as demonstrated in a recently published cohort study.2
Why Might There Be a Relationship Between Sedentariness and Cognitive Health?
Lower levels of physical activity are associated with higher risks of dyslipidemia, atherosclerosis, hypertension, thromboembolism, diabetes, and other conditions that have been associated with cerebrovascular disease and impaired cognitive health. In contrast, higher levels of physical activity are associated with greater collateral circulation and better blood supply to tissues, as well as with greater hippocampal neuroplasticity, all of which can protect against cognitive decline. Furthermore, physical activity may reduce the production and increase the removal of β-amyloid, and may also reduce oxidative stress and inflammatory processes that are harmful to the brain.3,4 Because sedentariness is an extreme example of low physical activity, it may predispose to poorer cognitive health through the stated mechanisms.
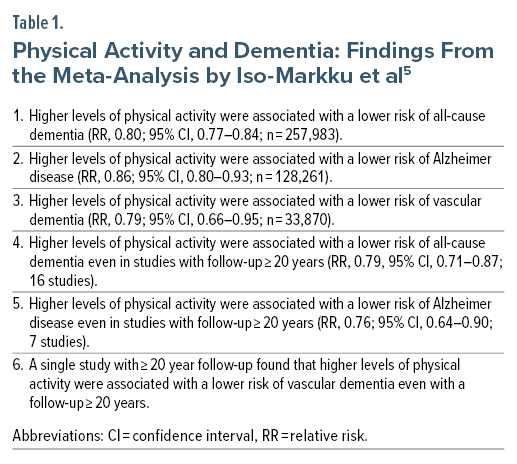
Physical Activity and Dementia: Meta-Analysis
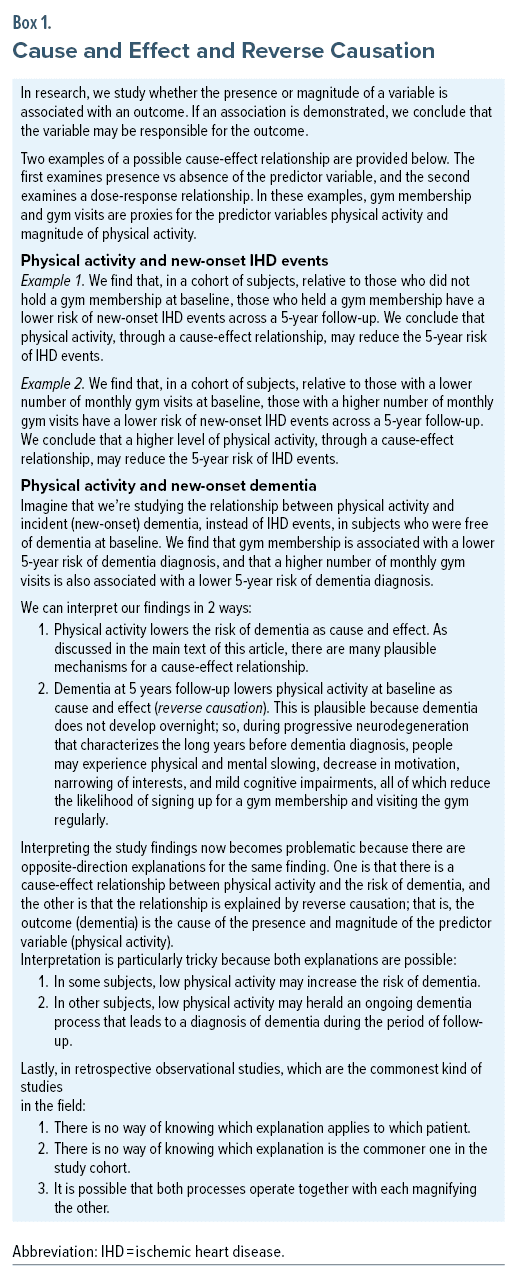
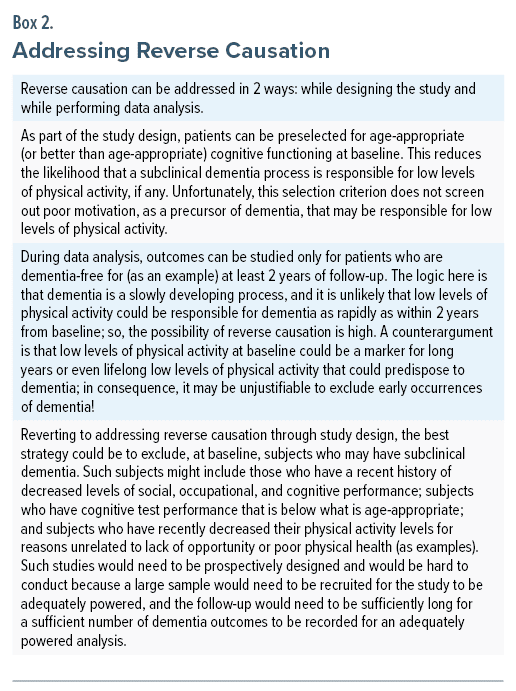
In a systematic review and meta-analysis of 58 observational studies, Iso-Markku et al5 found that higher levels of physical activity were associated with a lower risk of all-cause dementia, Alzheimer disease, and vascular dementia. The findings were consistent in analyses of studies with long follow-up (≥ 20 years) for all-cause dementia, Alzheimer disease, and vascular dementia (Table 1). The studies with long follow-up are important because they help exclude reverse causation as an explanation for the findings.4,6 Cause and effect and reverse causation are discussed in Box 1, and ways in which reverse causation can be addressed (in research) are suggested in Box 2.
Physical Inactivity and Dementia: Meta-Analysis
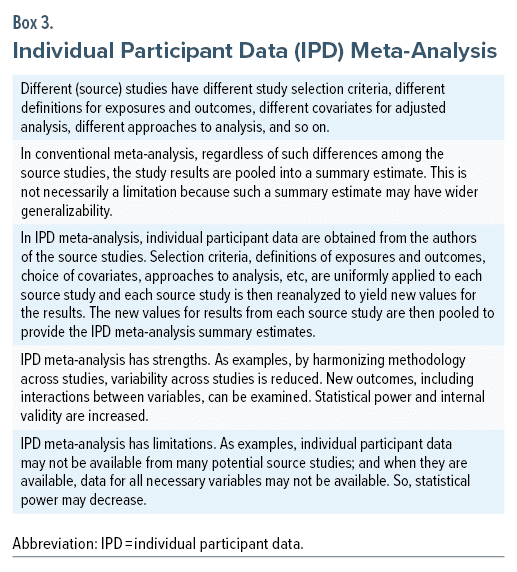
If higher levels of physical activity are associated with a lower risk of dementia, the finding can legitimately be expressed as the converse; that is, lower levels of physical activity should be associated with a higher risk of dementia. This has indeed been found in a systematic review and independent participant data (IPD) meta-analysis described by Kivimäki et al7; Box 3 provides a simple explanation about IPD meta-analysis.8
In this IPD meta-analysis,7 the exposure variable was physical inactivity, defined as very little or no physical activity. Because this definition could not be harmonized across the source studies, the best fit was taken; as an example, as less than 30 minutes per week of brisk walking (or any other equally or more vigorous exercise). In the first step, the source studies were reanalyzed with adjustment for age, sex, ethnicity, education, socioeconomic status, body mass index, smoking, and alcohol intake. The outcome variables were dementia and Alzheimer disease.
In the second step, data were pooled for 404,840 subjects in 19 observational studies. No subject had dementia at baseline. The authors7 found that, during the 10 years before dementia diagnosis, physical inactivity was associated with an increased risk of Alzheimer disease (hazard ratio [HR], 1.36; 95% confidence interval [CI], 1.12–1.65) and all-cause dementia (HR, 1.40; 95% CI, 1.21–1.62).
In order to rule out reverse causation as an explanation for the findings, the authors7 examined exposure to physical inactivity 10 years or longer before dementia diagnosis. They found that, in these analyses, physical inactivity was not associated with an increased risk of either Alzheimer disease (HR, 0.96; 95% CI, 0.85–1.08) or all-cause dementia (HR, 1.01; 95% CI, 0.89–1.14). There were minor differences in their summary estimates reported across abstract, main text, and figures, and what is presented here is what appeared in the main text.
Kivimäki et al7 interpreted their findings to indicate that reverse causation may explain the relationship between physical inactivity and dementia, and that physical activity may not play an important role in reducing long-term dementia risk. They failed to consider problems associated with a very long follow-up after a one-time measurement of physical activity. These problems include changes in levels of physical activity, the possibility that low levels of physical activity may have a lower impact in younger persons who carry a lower burden of cardiometabolic disease, and others.6
A further matter is that the authors7 defined the group of interest (subjects displaying physical inactivity) but did not define the comparison group (subjects displaying physical activity). Finally, despite having individual participant data, the authors could not or did not present information on how wide the separation in physical activity was between the groups being compared; if the separation was narrow, it might have explained the absence of long-term follow-up differences.
Thus, the findings of this IPD meta-analysis7 supported the possibility of reverse causation but could not confirm it. The counterarguments (presented above) to their conclusions are important because their findings should not discourage physically inactive persons from becoming more active.
Sedentariness and Dementia: Cohort Study
In the IPD meta-analysis by Kivimäki et al,7 people who spent their day puttering around the house and garden, or walking leisurely, daily, would have failed to meet the 30 minute threshold per week of brisk activity and would have been classified as physically inactive. Yet, such people would not be sedentary. Sedentariness, as explained earlier in this article, is not the same as lower levels of physical activity; sedentariness is an independent behavioral construct.1
Sedentary behaviors such as television viewing and driving have been associated with poorer cognitive test performances in both cross-sectional and longitudinal analyses.9 So, is sedentariness also associated with a higher risk of dementia? This question was examined in a retrospective cohort study with prospective data ascertainment, described by Raichlen et al.2
These authors extracted data from the UK Biobank. Subjects comprised 49,841 adults aged ≥ 60 years (mean age, 67 years; 55% female; 98% white) who provided wrist accelerometry data for 3–7 days (at least 16 h/d) and who were free from dementia at baseline. Sedentariness (waking behaviors expending ≤ 1.5 METs) was identified using a validated machine learning algorithm.
The reference value for the analyses was set at the median (sedentariness of 9.27 h/d). Analyses were adjusted for ethnicity, education, healthiness of diet, smoking and drinking, a deprivation index, presence of the APOE ε4 allele, medical comorbidities, body mass index, and depression. Importantly, analyses were also adjusted for health-related physical activity (≥ 3 METs) so that conclusions could be drawn about whether or not sedentariness, independent of health-related physical activity, was associated with dementia at a mean of 6.7 years of follow-up.
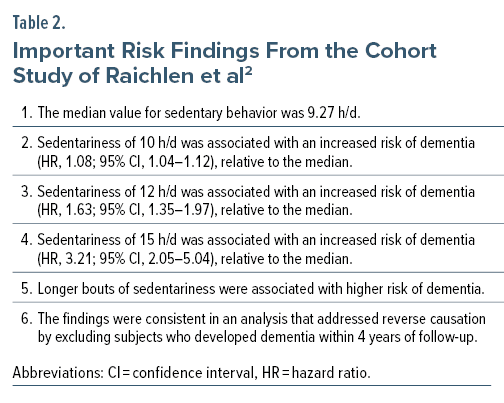
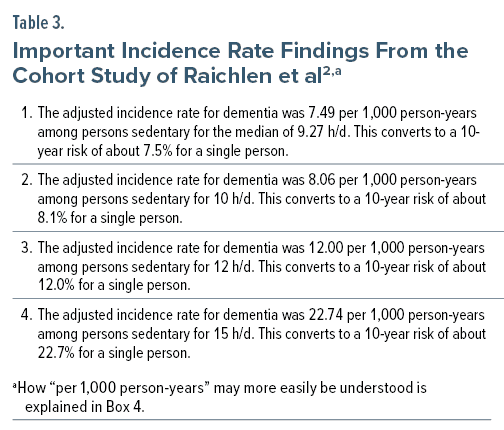
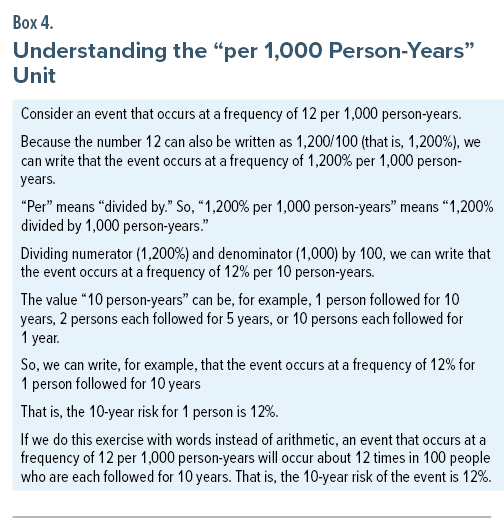
There were many important findings in this study; key findings are presented in Table 2 and Table 3, and translating “per 1,000 person-years” into a more meaningful unit is explained in Box 4.
Implications of the Study by Raichlen et al2
The study by Raichlen et al2 provides us with much food for thought. First, “median sedentariness” and not “least sedentariness” was the reference for the HRs presented in Table 2. Had “least sedentariness” been the reference, the risks of dementia (HR values) could have been much higher for progressively increasing levels of sedentariness.
Second, the adjusted 10-year risk of dementia showed a dose-dependent association with sedentariness (Table 3). It rose from about 8% with sedentariness at 10 h/d to about 23% with sedentariness at 15 h/d. Given that the average subject in the study was 67 years old, this means that, for the average person, the incidence of dementia, adjusted for confounds, would be 8% and 23% by age 77 years for sedentariness of 10 h/d and 15 h/d, respectively. The difference is large.
Third, the findings were consistent even in sensitivity analyses that addressed reverse causation by excluding subjects who developed dementia within 4 years of follow-up. Last, but not least, because the associations between sedentariness and dementia were statistically significant even after adjusting for time spent in moderate to vigorous physical activity, reduction in sedentariness assumes importance independent of engagement in physical activity.
Take-Home Message
Moderate to vigorous physical activity is associated with a reduced risk of dementia. Sedentariness, independent of levels of moderate to vigorous physical activity, is associated with an increased risk of dementia. These findings hold true even in analyses that attempt to address reverse causation as an explanation. Although residual confounding can explain the findings, and although no randomized controlled trials exist to demonstrate reduced dementia risk in persons who switch from sedentary to active lifestyle, it could be prudent to make the switch if only because sedentariness has been associated with many other adverse health outcomes, and physical activity, with favorable health outcomes.
Parting Notes
If physical activity protects against dementia, then, intuitively, people whose occupation requires physical activity should have a lower risk of dementia. However, studies have found that occupational physical activity is actually associated with higher risk of dementia.10,11 There are many possible explanations for this counterintuitive finding. The most obvious is inadequate adjustment for confounding; for example, people with lower baseline cognitive reserve are more likely to drift into labor-intensive jobs. Other explanations are that occupational physical activity might be associated with environmental hazards, high stress, low intellectual and social engagement, low autonomy, poor nutrition, short opportunities for recovery, and other factors that could be adverse to brain health and that are incompletely or not adjusted for in analyses.
Article Information
Published Online: Month 00, 2024. https://doi.org/10.4088/JCP.24f15270
© 2024 Physicians Postgraduate Press, Inc.
To Cite: Andrade C. Physical exercise and health, 6: sedentary time, independent of health-related physical activity, as a risk factor for dementia in older adults. J Clin Psychiatry. 2024;85(1):24f15270.
Author Affiliations: Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
 Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
Financial disclosure and more about Dr Andrade.
References (11)

- Andrade C. Physical exercise and health, 5: sedentary time, independent of health-related physical activity, as a risk factor for adverse physical health and mental health outcomes. J Clin Psychiatry. 2024;85(1):24f15261.
- Raichlen DA, Aslan DH, Sayre MK, et al. Sedentary behavior and incident dementia among older adults. JAMA. 2023;330(10):934–940. PubMed CrossRef
- De la Rosa A, Olaso-Gonzalez G, Arc-Chagnaud C, et al. Physical exercise in the prevention and treatment of Alzheimer’s disease. J Sport Health Sci. 2020;9(5):394–404. PubMed CrossRef
- Andrade C. Physical exercise and health, 1: an overview of terminology, guidance, benefits, and risks. J Clin Psychiatry. 2023;84(5):23f15099.
- Iso-Markku P, Kujala UM, Knittle K, et al. Physical activity as a protective factor for dementia and Alzheimer’s disease: systematic review, meta-analysis and quality assessment of cohort and case-control studies. Br J Sports Med. 2022;56(12):701–709. PubMed CrossRef
- Andrade C. Reverse causation, physical inactivity, and dementia. Indian J Psychol Med. 2020;42(2):205–206. PubMed CrossRef
- Kivimäki M, Singh-Manoux A, Pentti J, et al; IPD-Work consortium. Physical inactivity, cardiometabolic disease, and risk of dementia: an individual-participant meta-analysis. BMJ. 2019;365:l1495. PubMed CrossRef
- Veroniki AA, Seitidis G, Tsivgoulis G, et al. An introduction to individual participant data meta-analysis. Neurology. 2023;100(23):1102–1110. PubMed CrossRef
- Bakrania K, Edwardson CL, Khunti K, et al. Associations between sedentary behaviors and cognitive function: cross-sectional and prospective findings from the UK Biobank. Am J Epidemiol. 2018;187(3):441–454. PubMed CrossRef
- Nabe-Nielsen K, Holtermann A, Gyntelberg F, et al. The effect of occupational physical activity on dementia: results from the Copenhagen Male Study. Scand J Med Sci Sports. 2021;31(2):446–455. PubMed CrossRef
- Zotcheva E, Bratsberg B, Strand BH, et al. Trajectories of occupational physical activity and risk of later-life mild cognitive impairment and dementia: the HUNT4 70+ study. Lancet Reg Health Eur. 2023;34:100721. PubMed CrossRef
This PDF is free for all visitors!