Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
Have you ever wondered whether the presence of myoclonus helped to create or narrow your differential diagnosis? Have you ever been uncertain about whether or how to treat focal or diffuse myoclonus? If you have, then the following case vignette and discussion should prove useful.
The Importance of Identifying Myoclonus in the Setting of Mental Status Abnormalities:
Differential Diagnosis and Treatment

LESSONS LEARNED AT THE INTERFACE OF MEDICINE AND PSYCHIATRY
The Psychiatric Consultation Service at Massachusetts General Hospital (MGH) sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Drs Restrepo, Kochav, Goodheart, and Jain are residents in the Department of Medicine at Massachusetts General Hospital and clinical fellows of medicine at Harvard Medical School. Dr Stern is chief of the Avery D. Weisman Psychiatry Consultation Service at Massachusetts General Hospital and the Ned H. Cassem professor of psychiatry in the field of psychosomatic medicine/consultation at Harvard Medical School, Boston, Massachusetts.
Prim Care Companion CNS Disord 2016;18(5):doi:10.4088/PCC.16f01990
© Copyright 2016 Physicians Postgraduate Press, Inc.
Submitted: May 24, 2016; accepted June 27, 2016.
Published online: September 15, 2016.
Author contributions: Drs Restrepo, Kochav, Goodheart, and Jain contributed equally and are co-first authors.
Potential conflicts of interest: Dr Stern is an employee of the Academy of Psychosomatic Medicine, has served on the speaker’s board of Reed Elsevier, is a stock shareholder in WiFiMD (Tablet PC), and has received royalties from Mosby/Elsevier and the Massachusetts General Hospital Psychiatry Academy and McGraw Hill. Drs Restrepo, Kochav, Goodheart, and Jain report no conflicts of interest related to the subject of this article.
Funding/support: None.
Corresponding author: Theodore A. Stern, MD, Harvard Medical School Massachusetts General Hospital, Department of Psychiatry, Massachusetts General Hospital, Fruit St, WRN 605, Boston, MA 02114 ([email protected]).
Have you ever wondered whether the presence of myoclonus helped to create or narrow your differential diagnosis? Have you ever been uncertain about whether or how to treat focal or diffuse myoclonus? If you have, then the following case vignette and discussion should prove useful.
CASE VIGNETTE
Ms A, a 57-year-old woman, arrived at the emergency department (ED) with fever and an altered mental status described by her daughter as increased somnolence and confusion. She had a 3- to 4-week course of gradually worsening tremors and ataxia that resulted in difficulty feeding herself and walking. Her medical history was significant for schizophrenia, iatrogenic parkinsonism secondary to chronic antipsychotic therapy, type 2 diabetes mellitus, a nephrectomy for renal cell carcinoma, hypertension, and hyperlipidemia. Her psychotropic medications included amantadine, bupropion, trazodone, clonazepam, memantine, and perphenazine. Twelve days before her ED presentation, Ms A underwent an adrenalectomy (for a nonfunctional adrenaloma). Her vital signs in the ED were significant only for tachycardia. At admission to the general medical ward, a physical examination revealed a disheveled, chronically ill-appearing woman; her speech was rambling, and she was picking at the air. She was notably diaphoretic and exhibited prominent and diffuse myoclonus. The urinalysis was positive for pyuria; all other laboratory results were unremarkable (ie, metabolic function, lactate levels, and ammonia levels were within the normal range).
The initial differential diagnosis included serotonin syndrome, benzodiazepine withdrawal, Wernicke’s encephalopathy, and delirium secondary to a urinary tract infection. Her outpatient medications were discontinued, and she was started on high-dose thiamine. She underwent an empiric trial of lorazepam for potential benzodiazepine withdrawal. Given a lack of improvement, Ms A was transitioned to intramuscular olanzapine for the empiric treatment of delirium. The intramuscular route was chosen for consistent administration given Ms A’s mental status prohibiting consistent oral administration. Due to concern for rhabdomyolysis from continuous muscle contraction, she received intravenous fluid resuscitation. Given her lack of response to these interventions, additional consideration was given to an encephalitis (from infectious or paraneoplastic etiologies) as well as to a neurodegenerative process (such as Creutzfeldt-Jakob disease). As a result, more diagnostic tests were obtained.
An electroencephalogram (EEG) revealed generalized low-voltage theta waves with no evidence of epileptiform discharges, which was not suggestive of primary central nervous system pathology. Due to her severe myoclonus, she was intubated and sedated for a magnetic resonance imaging (MRI) scan; the findings were unremarkable. A lumbar puncture revealed a mildly elevated opening pressure (35 cm H2O) and cerebrospinal fluid (CSF) protein level (63 mg/dL; reference range, 5-55). A paraneoplastic antibody panel was negative, as was a 14-3-3 Gambetti protein for Creutzfeldt-Jakob disease. A computed tomography scan of the abdomen, looking for postoperative intra-abdominal infection, was significant only for expected postadrenalectomy changes.
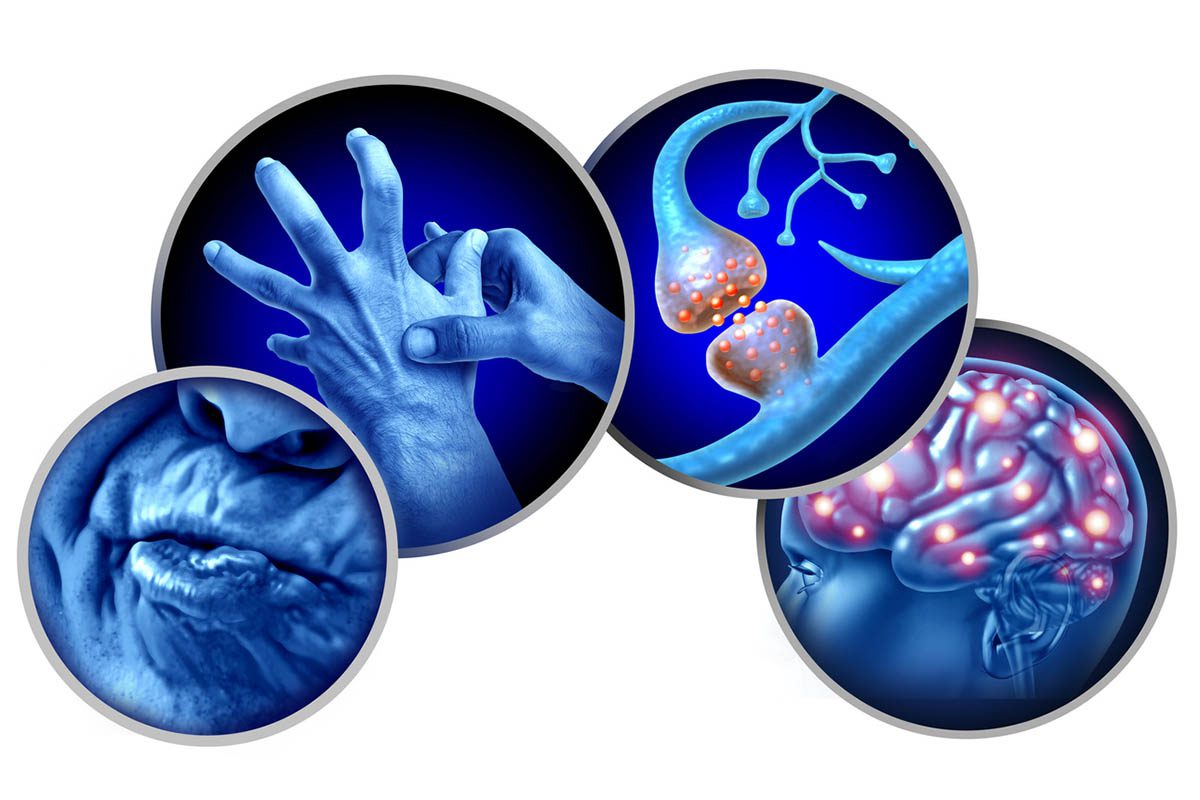
WHAT IS MYOCLONUS
Myoclonus is defined as brief, involuntary movements caused by temporary muscle fiber activation or inhibition. Neuroanatomic localization of this phenomenon is often difficult, as lesions throughout the entire neuraxis have been known to cause its characteristic jerking. Myoclonus can be classified into several subcategories on the basis of its features, etiology, and distribution. Primary myoclonus, which refers to an idiopathic phenomenon that accompanies seizure disorders, is most often hereditary and is seen more frequently in the pediatric population. Also, it often exists with no changes in mental status; thus, it will not be discussed here. As such, we will focus our attention on the discussion of secondary etiologies. Additionally, the movements can be further classified on the basis of their timing: jerks that occur at rest are known as positive myoclonus, while those that occur during contraction are known as negative myoclonus. The latter is epitomized by asterixis and is seen predominantly in metabolic encephalopathies (secondary to renal, hepatic, and respiratory failure). When the movement disorder extends beyond one muscle group or extremity, it is referred to as generalized or multifocal myoclonus.

- Myoclonus often accompanies changes in mental status that may be useful in guiding the differential diagnosis and workup.
- Clinical information, such as the time course, accompanying cognitive deficits, medical history, and current medications, provides a useful framework for narrowing the differential diagnosis.
- Laboratory work should be tailored to assess for the presence of organ dysfunction that may account for metabolic encephalopathies; intracranial imaging, electroencephalography, and lumbar puncture are adjunctive diagnostics that can also be considered.
WHO GETS MYOCLONUS?
There are minimal data regarding the incidence and prevalence of secondary generalized myoclonus.1 Most patients with myoclonus have additional neurologic or systemic manifestations of their underlying pathology. Underlying pathologies include neurologic processes as well as toxic-metabolic, autoimmune, infectious, drug, toxin, and paraneoplastic processes.
Neurologic causes include neurodegenerative disorders, spinocerebellar ataxias, and liposomal storage diseases. For patients who gradually develop myoclonus earlier in life, non-secondary causes such as dystonias, epilepsy, and ataxias should be considered. Myoclonus in neurodegenerative diseases can be multifocal or generalized. Myoclonus in Alzheimer’s disease develops late in its course in about one-fourth of patients.2 Myoclonus in Parkinson’s disease may be frequent enough to resemble action tremors, and myoclonus in Lewy body dementia tends to be more common and more severe than in Parkinson’s disease.3 Myoclonus can also be present in multiple system atrophy, progressive supranuclear palsy, and frontotemporal dementia. Notably, myoclonus is unique in Creutzfeldt-Jakob disease, since it tends to be generalized and provoked by loud noises ("startle myoclonus").
Toxic-metabolic causes tend to present acutely, and these may include electrolyte or acid-base abnormalities, renal or hepatic dysfunction, and posthypoxic insults. Many neurologic infections have been implicated, as have some autoimmune causes such as celiac disease and Hashimoto’s disease. Drug-induced causes are many and will be discussed in further detail elsewhere in this article. Most notable of the paraneoplastic causes is a variation known as opsoclonus-myoclonus syndrome, which causes saccadic orbital movements in addition to myoclonus. This variation is commonly associated with neuroblastomas in children but is also associated with carcinomas in adults, particularly breast and small cell lung carcinomas.4 Finally, psychogenic cases have occurred, and the major differentiating factors for this entity are found with routine testing in the evaluation of myoclonus.
WHY DOES MYOCLONUS DEVELOP?
Although myoclonus has myriad etiologies, anatomic pathologies, clinical manifestations, and classifications (eg, physiologic, essential, epileptic, secondary),5 2 basic mechanisms account for the onset of myoclonus: involuntary muscular contractions (positive myoclonus) and muscular inhibition (negative myoclonus or asterixis). When characterizing myoclonus by its anatomic and physiologic characteristics, 5 broad categories (cortical, cortical-subcortical, subcortical-supraspinal [nonsegmental], spinal [segmental], and peripheral) exist that represent territories from which electrical discharges can arise. Each of them will be discussed here, along with their common EEG and electromyography (EMG) findings and with examples of their clinical manifestations.5
Cortical myoclonus is caused by an electrical discharge that occurs within the sensorimotor cortex and that corresponds to a body part (eg, face, arm). The electrical discharge that ensues can be a response to a stimulus, as is seen in cortical reflex myoclonus. The cortical discharge has the ability to spread in a somatotopic pattern within the somatosensory cortex via corticocortical pathways. Spread can also occur through callosal pathways to the opposite hemisphere; this accounts for its potential to generate generalized seizures.6 Cortical reflex myoclonus has variable EEG findings, but if an EEG sharp wave is seen, it will typically arise 10-40 ms before the myoclonic jerk develops. On the EMG, bursts are < 75 ms.5 Cortical myoclonus can be negative, which corresponds to a silent period on the EMG.7 Examples include drug- or toxin-induced myoclonus, posthypoxic action myoclonus, myoclonus due to a neurodegenerative disease with cortical involvement, progressive myoclonic epilepsies and ataxia, and cortical reflex myoclonus.5,6
Cortical-subcortical myoclonus refers to an abnormal bidirectional electrical oscillation between cortical and subcortical areas.5 It is characterized by a generalized spike and wave pattern on the EEG and bursts that are < 100 ms on the EMG.5 This type of myoclonus is often secondary to primary generalized myoclonic seizures or absence seizures.5
Subcortical-supraspinal (nonsegmental) myoclonus is due to a discharge arising from a subcortical focus that can spread to pyramidal or extrapyramidal tracts.8 This type of myoclonus has variable EEG and EMG findings.5 Examples of this type of myoclonus include essential myoclonus and opsoclonus-myoclonus.5
Spinal (segmental) myoclonus can refer to myoclonus that originates from the brain stem or the spinal cord. The brain stem typically produces axial myoclonus that is often provoked by certain stimuli, particularly auditory stimuli. Spinal segmental myoclonus stems from hyperexcitability of a segment of the spinal cord (secondary to viral irritation, ischemia, or a mass effect from glioma or syringomyelia). The propriospinal system leads mainly to axial myoclonus that spares the face (in contrast to myoclonus that originates from the brain stem).5 EMG bursts are characteristically > 100 ms and are usually accompanied by a normal EEG,5 as might occur with palatal myoclonus.8
Peripheral myoclonus is also associated with a normal EEG; the EMG reveals variable burst duration.5 One cause of peripheral myoclonus is hemifacial spasm.8
Drug-Induced Myoclonus
Several drugs (eg, antibiotics [quinolones, penicillins, and cephalosporins], antidepressants [particularly cyclic antidepressants, selective serotonin reuptake inhibitors, monoamine oxidase inhibitors, and lithium], benzodiazepines [eg, with benzodiazepine withdrawal], opiates, and dopamine agonists and dopamine blockers [neuroleptics], as well as cholinesterase inhibitors, antiepileptics, bismuth salts, general anesthetics, antiarrhythmics, calcium channel blockers, and others)8-10 have been associated with the onset of myoclonus. Level II evidence exists for levodopa, cyclic antidepressants, and bismuth salts; there is less evidence that implicates other drugs as causative agents in myoclonus.10 The etiology of drug-induced myoclonus is poorly understood. However, it has been postulated that increased levels of serotonin may be etiologically responsible. The 2 neurotransmitter systems most frequently implicated in the pathophysiology of myoclonus are the serotonergic and γ-aminobutyric acid (GABA)-ergic systems. Drug-specific approaches have been studied in certain toxidromes, such as the use of benzodiazepines11 or the serotonin receptor antagonist antihistamine cyproheptadine12 in cases of suspected serotonin syndrome or the use of the serotonin receptor antagonist methysergide in levodopa toxicity.13 Removal of the offending agent usually results in a gradual resolution of the myoclonus.
HOW SHOULD MYOCLONUS BE EVALUATED AND TREATED?
The evaluation and treatment of myoclonus begins with a detailed history and physical examination, targeted diagnostic studies, and, often, empiric therapeutics, which in and of themselves have diagnostic value. The key to the initial evaluation is to identify whether the myoclonus is most likely a primary process, epileptic in etiology, or secondary to another medical process.
History and Physical
The history and physical examination should be used to delineate the distribution (eg, focal, multifocal, generalized), temporality (eg, acuity of onset, continuous versus intermittent, frequency of episodes, progression of symptoms), and triggers for myoclonus (eg, spontaneous, induced by reflex, induced by action).
Associated symptoms should be placed in the context of signs of infection, toxic-metabolic derangements, or neurologic derangements (eg, ataxia, cognitive decline). The medical history should be assessed for seizure disorder, known neurodegenerative processes, or chronic medical conditions, which if not well controlled can lead to metabolic disarray and to secondary myoclonus (eg, from hepatic failure, renal failure, pulmonary disease, thyroid disease, or diabetes). The family history should also screen for rare causes of hereditary myoclonus or neurodegenerative disease. A patient’s medication history should be scrutinized, paying particular attention to medications recently started and recently discontinued, as well as for use of illicit agents and possible toxic exposures.
Diagnostic Studies
If the etiology of myoclonus is not immediately revealed by the history and physical examination, selected diagnostic tests should be performed in a step-wise fashion, guided by the differential diagnosis.
All patients should be tested for basic chemistries (eg, electrolytes, renal function tests, calcium, and magnesium) to assess for electrolyte abnormalities or uremia as potential metabolic etiologies. The serum blood glucose level should also be checked, as both hypoglycemic and hyperglycemic states are associated with myoclonus. If any degree of encephalopathy is detected, it is also reasonable to screen for hepatic failure (with liver function tests and a serum ammonia level) and for hyperthyroidism and hypothyroidism (with screening thyroid function tests). Exacerbation of lung disease should raise concern for hypercapnia and lead to consideration of blood gas determination. There should be a low threshold for screening for drugs and toxins if there is any suspicion of undisclosed ingestions or use of illicit or nonillicit psychoactive medication. A basic infectious workup (with complete blood count, urinalysis, chest x-ray, and blood cultures) should be pursued if there are localizing signs of infection, fever, leukocytosis, or encephalopathy.
The next tier of diagnostic testing comprises dedicated central nervous system testing. This testing includes EEG, brain imaging, and CSF analysis. The EEG can identify both ictal and interictal discharges in epileptic myoclonus or characteristic disease-specific abnormalities (eg, periodic sharp-wave complexes in Creutzfeldt-Jakob disease). The EMG, together with the EEG, can assist in differentiating among different mechanisms of myoclonus. Brain, with or without spinal, imaging may reveal lesions or patterns involving atrophy that support a specific etiology for myoclonus. MRI is preferred over computed tomography (CT) screening due to its increased sensitivity in identifying specific lesions. Clinicians should have a low threshold for performing a lumbar puncture and CSF analysis in cases in which infection, inflammation, or certain neurodegenerative processes are being considered. The CSF analysis should include an opening pressure, cell count, gram stain/bacterial culture, and protein/glucose levels, with additional testing obtained for specific infectious agents and conditions (eg, herpes simplex virus, varicella zoster virus, Cryptococcus, syphilis, Lyme disease, or Arboviridae), inflammatory processes (eg, with a paraneoplastic antibody panel), or neurodegenerative processes (eg, 14-3-3 protein) on the basis of clinical suspicion.
A substantial amount of time may pass between initiation of the above diagnostic testing and determination of a definitive etiology. During this period, a patient’s ongoing myoclonus may be distressing to the patient and may actually interfere with diagnostic testing. Under these circumstances, empiric therapeutic trials (which often have diagnostic value) should be started.
Treatment
The treatment for myoclonus is predicated on its underlying etiology. In instances in which the myoclonus is a primary process or the underlying etiology cannot be easily reversed, treatments are directed toward the underlying mechanism of the myoclonus (ie, cortical, cortical-subcortical, subcortical nonsegmental, segmental, or peripheral myoclonus). Due to the frequent lack of efficacy of initial therapeutic options, polyphamarcy and its consequences frequently complicate the management of chronic myoclonus.
Cortical myoclonus. Cortical myoclonus is the etiologic mechanism of the overwhelming majority of myoclonic processes (including systemic infectious and metabolic etiologies, drug/toxin, and neurodegenerative disease with cortical involvement) seen in hospital settings. Accepted therapies for cortical myoclonus include levetiracetam,14,15 piracetam,16,17 clonazepam, and valproic acid.18
Given their relatively favorable side effect profiles, levetiracetam and piracetam are the preferred initial agents for chronic cortical myoclonus, although multiple agents (in combination) are often needed to achieve the desired effect.
Cortical-subcortical myoclonus. This is the mechanism of myoclonus in the primary generalized epilepsy syndromes. The treatments for these conditions are complex and syndrome-dependent.
Subcortical-supraspinal (nonsegmental) myoclonus. This mechanism underlies a heterogeneous group of etiologies of myoclonus, including essential myoclonus and opsoclonus-myoclonus. Evidence for treatment of these syndromes varies based on the underlying diagnosis, but therapies predominantly involve targeting the GABAergic pathways through medications such as clonazepam. The myoclonus-dystonia syndrome has at its mechanistic root circuit abnormality in the basal ganglia, which is possibly the reason for this syndromes’ responsiveness to anticholinergic medications such as benztropine and trihexyphenidyl. Several alternative medication classes and agents (including antiepileptics, neuroleptics, serotonergic agents, and levodopa)19 have been used with some success.
Spinal (segmental) myoclonus. This is the mechanism of myoclonus seen in palatal myoclonus. Spinal myoclonus is characteristically difficult to treat. Options include local botulinum toxin injections20,21 or pharmacologic management. Clonazepam is often used as a first-line agent, and several alternative antiepileptic agents have also been used with success.22
Peripheral myoclonus. This is the mechanism of myoclonus seen in hemifascial spasm and spinal segmental myoclonus. It is best treated with localized botulinum toxin injections.23 Systemic medications have shown only limited benefit in this subcategory.
CASE CONCLUSION
Several days after her psychotropic agents were withheld and supportive care delivered, Ms A’s tremors and myoclonus subsided, and she gradually regained her baseline (conversant and pleasant) mental status. On the day of discharge, she was ambulating with physical therapy and felt much improved, with no recollection of the preceding days. Given that a unifying, primary diagnosis could not be made, her mental status changes and generalized myoclonus were thought to be due to profound encephalopathy from a urinary tract infection in the setting of multiple neuroleptic and psychotropic medications.
REFERENCES
1. Caviness JN, Alving LI, Maraganore DM, et al. The incidence and prevalence of myoclonus in Olmsted County, Minnesota. Mayo Clin Proc. 1999;74(6):565-569. PubMed doi:10.4065/74.6.565
2. Portet F, Scarmeas N, Cosentino S, et al. Extrapyramidal signs before and after diagnosis of incident Alzheimer disease in a prospective population study. Arch Neurol. 2009;66(9):1120-1126. PubMed doi:10.1001/archneurol.2009.196
3. Caviness JN, Adler CH, Beach TG, et al. Myoclonus in Lewy body disorders. Adv Neurol. 2002;89:23-30. PubMed
4. Honnorat J. New findings in adult opsoclonus-myoclonus syndrome. JAMA Neurol. 2016;73(4):381-382. PubMed doi:10.1001/jamaneurol.2015.4757
5. Caviness JN, Brown P. Myoclonus: current concepts and recent advances. Lancet Neurol. 2004;3(10):598-607. PubMed doi:10.1016/S1474-4422(04)00880-4
6. Brown P, Day BL, Rothwell JC, et al. Intrahemispheric and interhemispheric spread of cerebral cortical myoclonic activity and its relevance to epilepsy. Brain. 1991;114(pt 5):2333-2351. PubMed doi:10.1093/brain/114.5.2333
7. Shibasaki H, Hallett M. Electrophysiological studies of myoclonus. Muscle Nerve. 2005;31(2):157-174. PubMed doi:10.1002/mus.20234
8. Caviness JN, Truong DD. Myoclonus. In: Weiner WJ, Tolosa E, eds. Handbook of Clinical Neurology. Amsterdam, The Netherlands: Elsevier; 2011:399-420.
9. Brefel-Courbon C, Gardette V, Ory F, et al. Drug-induced myoclonus: a French pharmacovigilance database study. Neurophysiol Clin. 2006;36(5-6):333-336. PubMed doi:10.1016/j.neucli.2006.12.003
10. Jiménez-Jiménez FJ, Puertas I, de Toledo-Heras M. Drug-induced myoclonus: frequency, mechanisms and management. CNS Drugs. 2004;18(2):93-104. PubMed doi:10.2165/00023210-200418020-00003
11. Nisijima K, Shioda K, Yoshino T, et al. Diazepam and chlormethiazole attenuate the development of hyperthermia in an animal model of the serotonin syndrome. Neurochem Int. 2003;43(2):155-164. PubMed doi:10.1016/S0197-0186(02)00213-9
12. Gillman PK. The serotonin syndrome and its treatment. J Psychopharmacol. 1999;13(1):100-109. PubMed doi:10.1177/026988119901300111
13. Hirschorn KA, Greenberg HS. Successful treatment of levodopa-induced myoclonus and levodopa withdrawal-induced neuroleptic malignant syndrome: a case report. Clin Neuropharmacol. 1988;11(3):278-281. PubMed doi:10.1097/00002826-198806000-00011
14. Genton P, Gélisse P. Antimyoclonic effect of levetiracetam. Epileptic Disord. 2000;2(4):209-212. PubMed
15. Striano P, Manganelli F, Boccella P, et al. Levetiracetam in patients with cortical myoclonus: a clinical and electrophysiological study. Mov Disord. 2005;20(12):1610-1614. PubMed doi:10.1002/mds.20530
16. Koskiniemi M, Van Vleymen B, Hakamies L, et al. Piracetam relieves symptoms in progressive myoclonus epilepsy: a multicentre, randomised, double blind, crossover study comparing the efficacy and safety of three dosages of oral piracetam with placebo. J Neurol Neurosurg Psychiatry. 1998;64(3):344-348. PubMed doi:10.1136/jnnp.64.3.344
17. Brown P, Steiger MJ, Thompson PD, et al. Effectiveness of piracetam in cortical myoclonus. Mov Disord. 1993;8(1):63-68. PubMed doi:10.1002/mds.870080112
18. Obeso JA, Artieda J, Rothwell JC, et al. The treatment of severe action myoclonus. Brain. 1989;112(pt 3):765-777. PubMed doi:10.1093/brain/112.3.765
19. Kinugawa K, Vidailhet M, Clot F, et al. Myoclonus-dystonia: an update. Mov Disord. 2009;24(4):479-489. PubMed doi:10.1002/mds.22425
20. Penney SE, Bruce IA, Saeed SR. Botulinum toxin is effective and safe for palatal tremor: a report of five cases and a review of the literature. J Neurol. 2006;253(7):857-860. PubMed doi:10.1007/s00415-006-0039-9
21. Lagueny A, Tison F, Burbaud P, et al. Stimulus-sensitive spinal segmental myoclonus improved with injections of botulinum toxin type A. Mov Disord. 1999;14(1):182-185. PubMed doi:10.1002/1531-8257(199901)14:1<182::AID-MDS1040>3.0.CO;2-8
22. Caviness JN. Treatment of myoclonus. Neurotherapeutics. 2014;11(1):188-200. PubMed doi:10.1007/s13311-013-0216-3
23. Costa J, Esp×rito-Santo C, Borges A, et al. Botulinum toxin type A therapy for hemifacial spasm. Cochrane Database Syst Rev. 2005;(1):CD004899. PubMed
Enjoy this premium PDF as part of your membership benefits!