A Case of Cerebral Venous Thrombosis in a 77-Year-Old White Man
To the Editor: We present a case of cerebral venous thrombosis in a 77-year-old otherwise healthy man with a recent diagnosis of otitis media.
Case report. Mr A, a 77-year-old white, otherwise healthy man, was brought by his sister in 2010 to a tertiary hospital emergency department having experienced worsening headache with confusion and decreased vision for 7 days. Review of records showed that the patient had presented to an urgent care center with headache and earache 2 and a half weeks earlier, at which time he was diagnosed with otitis media by an ear, nose, and throat surgeon. He was treated with cephalexin for 5 days and experienced complete resolution of symptoms prior to the current presentation.
Mr A saw an ophthalmologist for worsening headache and decreased vision; the ophthalmologist found papilledema (bilateral disc edema) with associated lateral rectus palsy, which was presumed due to increased intracranial pressure. The ophthalmology department requested a neurologic consult. Neurologic examination assessed this patient as alert and oriented. The patient was found to have severe deafness, bilateral papilledema, and right sixth cranial nerve palsy. There was no facial asymmetry, pronator drift, gross motor weakness in extremities, or incoordination. The patient was able to stand from sitting using support with a walker.
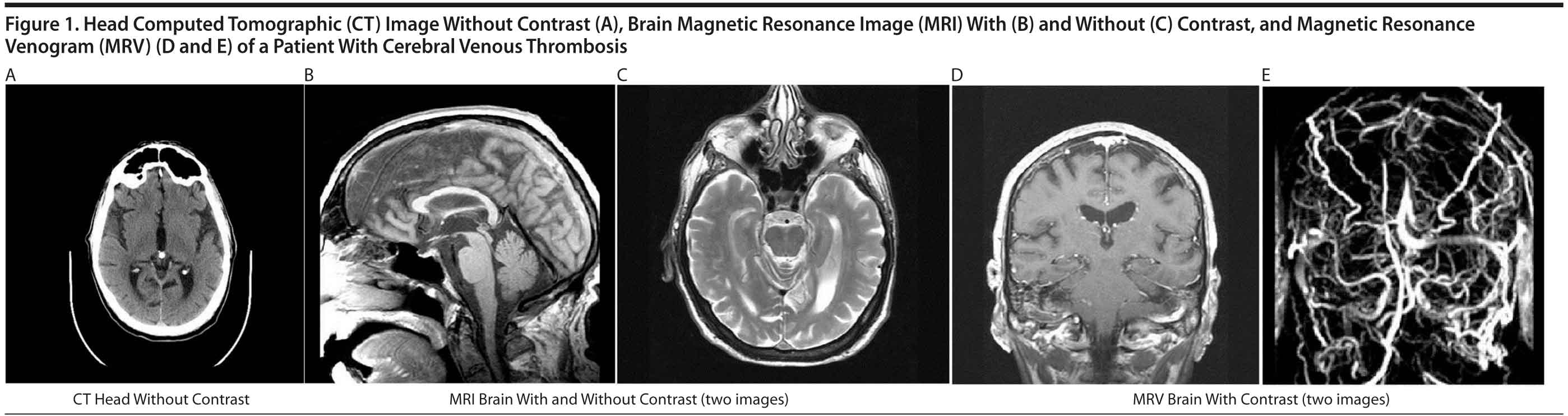
Clinical symptoms were highly suspicious for right temporal lobe abscess secondary to mastoiditis on the right. Computed tomography (CT) of the head (Figure 1A) was negative for abscess or mass effect. Differential diagnosis at that point included possible meningeal malignancy or idiopathic intracranial hypertension. Lumbar puncture, which was performed in light of chronic meningitis, revealed clear cerebrospinal fluid (CSF) with raised pressure (> 55 cm water), a white blood cell count of 11 ×— 109/L with predominant lymphocytes, a minimally raised serum protein level of 47 g/L, a glucose level within normal limits, and no India ink; gram stain was negative and revealed no bacterial organisms. Findings of cytology and other chronic meningitis workup were negative.
Thus, the patient was presumably diagnosed with idiopathic intracranial hypertension in light of CSF results and no evidence of definite etiology. A possible spread for infection to involve the venous sinuses and venous thrombosis was suspected given recent history of otitis media and mastoiditis, which can rarely cause idiopathic intracranial hypertension. Magnetic resonance imaging (MRI) (Figure 1B and 1C) and magnetic resonance venogram (MRV) (Figure 1D and 1E) were specifically ordered to rule out cerebral venous thrombosis. The patient was empirically started on treatment with mannitol, intravenous ceftriaxone, and acetazolamide. MRI/MRV of the brain showed complete thrombosis of superior sagittal sinus and right transverse sinus, which explained the patient’s raised intracranial pressure. The patient was treated with intravenous heparin and was later transferred to a university hospital for further management of progressive headache on day 15 of hospitalization.
Upon transfer to the university hospital, the patient was continued on intravenous heparin. The patient’s condition improved initially but was later complicated by heparin-induced thrombocytopenia, which required the use of low molecular weight heparin. The patient’s condition further worsened with impairment of vision requiring lumboperitoneal shunt and stopping of anticoagulation treatment. Anticoagulation treatment was subsequently restarted, but Mr A developed cerebellar hemorrhage, which resulted in his demise.
Our patient lacked peculiar demographics of patients with idiopathic intracranial hypertension. Also, initial negative noncontrast CT scan was not sufficient and is often misleading in patients with cerebral venous thrombosis. We document a rare case of cerebral venous thrombosis in a 77-year-old man with initial normal noncontrast brain CT. Although rare, cerebral venous thrombosis can present in an elderly man with recent history of otitis media and with negative brain CT. This case also explains the need for MRI and MRV of the brain in patients with persistent headache of unknown origin with increased intracranial hypertension and negative brain CT. MRI alone is 64% and MRI with MRV is 100% specific for diagnosis of cerebral venous thrombosis.
Idiopathic intracranial hypertension is an infrequent and enigmatic condition almost always encountered in overweight or obese women of childbearing age.1 Idiopathic intracranial hypertension requires the demonstration of an intracranial hypertensive status not associated with CSF abnormalities or with any other detectable intracranial pathology.1 Differential diagnosis with cerebral venous thrombosis may be challenging since an isolated intracranial hypertension may be the only presenting sign in about one-third of cerebral venous thrombosis cases,2 and a cerebral venous thrombosis has been found in 11.4% of patients who were presumed to have idiopathic intracranial hypertension.3 It is much more common in females, whose cases comprise about 75% of adult cases.4
Cerebral venous thrombosis is a relatively uncommon but serious neurologic disorder that is potentially reversible with prompt diagnosis and appropriate medical care.5 The predisposing factors to this condition are mainly genetic and acquired prothrombotic states and infection. It usually presents in a puzzling way. The frequency of infectious sinus thrombosis has declined and varies from 6% to 12% in large series of adults with sinus thrombosis.4,6 In view of nonspecific and varied symptomatology and presentation, cerebral venous thrombosis is often misdiagnosed (70% of cases) or diagnosis is delayed (40% of cases). The clinical picture of cerebral venous thrombosis is nonspecific and highly variable and can mimic several other clinical conditions.7 Sinus thrombosis may occur as part of the intracranial hypertension syndrome and should be excluded with detailed imaging (MRI and MRV or CT venography) in all patients with such manifestations.5 Magnetic resonance imaging alone is 64% sensitive and in conjunction with magnetic resonance venography is a 100% sensitive examination technique.8 The key imaging finding of cerebral venous thrombosis on MRI is the absence of normal flow void on T1- and T2-weighted images.9 The combination of acutely increased intracranial pressure and large deep venous infarcts is dangerous, and patients may die within hours from cerebral herniation.10
References
1. Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59(10):1492-1495. PubMed
2. Biousse V, Ameri A, Bousser MG. Isolated intracranial hypertension as the only sign of cerebral venous thrombosis. Neurology. 1999;53(7):1537-1542. PubMed
3. Agarwal P, Kumar M, Arora V. Clinical profile of cerebral venous sinus thrombosis and the role of imaging in its diagnosis in patients with presumed idiopathic intracranial hypertension. Indian J Ophthalmol. 2010;58(2):153-155. PubMed doi:10.4103/0301-4738.60092
4. Ferro JM, Canh×£o P, Stam J, et al; ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004;35(3):664-670. PubMed doi:10.1161/01.STR.0000117571.76197.26
5. Leach JL, Fortuna RB, Jones BV, et al. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006;26(suppl 1):S19-S41, discussion S42-S43. PubMed doi:10.1148/rg.26si055174
6. Bousser M-G, Ross Russell RW. Cerebral Venous Thrombosis. London, UK: WB Saunders; 1997.
7. Filippidis A, Kapsalaki E, Patramani G, et al. Cerebral venous sinus thrombosis: review of the demographics, pathophysiology, current diagnosis, and treatment. Neurosurg Focus. 2009;27(5):E3. PubMed doi:10.3171/2009.8.FOCUS09167
8. Lafitte F, Boukobza M, Guichard JP, et al. MRI and MRA for diagnosis and follow-up of cerebral venous thrombosis (CVT). Clin Radiol. 1997;52(9):672-679. PubMed doi:10.1016/S0009-9260(97)80030-X
9. Hinman JM, Provenzale JM. Hypointense thrombus on T2-weighted MR imaging: a potential pitfall in the diagnosis of dural sinus thrombosis. Eur J Radiol. 2002;41(2):147-152. PubMed doi:10.1016/S0720-048X(01)00365-5
10. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;352(17):1791-1798. PubMed doi:10.1056/NEJMra042354
Author affiliations: Department of Neurology, Veterans’ Affairs Medical Center, Salem (Dr Gullapalli); Carilion Clinic, Virginia Tech School of Medicine, Roanoke (Dr Sharma), Virginia; Mountain State University, Beckley, West Virginia (Mr Duncan); and Pandit Deendayal Upadhyay Medical College, Rajkot, Gujarat, India (Dr Shah).
Potential conflicts of interest: None reported.
Funding/support: None reported.
Published online: November 10, 2011.
Prim Care Companion CNS Disord 2011;13(6):doi:10.4088/PCC.11l01217
© Copyright 2011 Physicians Postgraduate Press, Inc.