Postpartum depression (PPD) affects up to 20% of birthing parents and has a significant negative impact on birthing parent infant dyads.1,2 Cognitive-behavioral therapy (CBT) is established as an effective evidence-based treatment for PPD,3,4 but no studies have examined if infant temperament can predict parental treatment outcomes. Temperamental distress to limitation, which refers to infants’ distress when restricted from activities,5 is particularly significant. Infants high in this trait are likely to display defiance,6 and their fussiness and frustration in response to restrictions demand consistent parental attention, making distress to limitation a tangible component of dyadic interactions for parents.7,8 Indeed, distress to limitation has been shown to explain unique variance in bonding and attachment security.9,10 Therefore, this study examines if infant distress to limitation predicts greater maternal depressive symptoms following CBT for PPD. We hypothesized that greater baseline infant distress to limitation will predict increased maternal PPD symptoms posttreatment. Understanding how infant temperament associates with maternal treatment response could aid treatment selection and optimization of interventions for dyads.
Methods
Forty birthing parent-infant dyads were recruited during March 2016–July 2019 from Ontario, Canada. Participants must have had a primary MDD diagnosis confirmed by a psychiatrist using DSM-5 criteria; been free of bipolar disorder, schizophrenia, or substance use disorders; been fluent in English; and had infants <12 months old. Participants received a 9-week in person group CBT for PPD in weekly 2-hour sessions delivered by psychotherapists in pairs.11 Each session’s first half covered core CBT content, while the second half included discussions on relevant topics co-led by patients and therapists. Data were collected at 3 points: postfirst session (T1), posttreatment (T2), and 3 months later (T3). The Hamilton Integrated Research Ethics Board approved the study (#0912), and all participants gave informed consent.
Birthing parents completed both the Edinburgh Postnatal Depression Scale (EPDS)12 assessing their PPD symptoms (Cronbach α = 0.85) and the distress-to-limitation subdomain of the Infant Behavior Questionnaire Revised Short-Form13 to assess infant distress (α = 0.68). Distress to limitation was chosen a priori based on evidence indicating that this stable infant characteristic14 may be especially challenging for parents,6–10 potentially hindering their improvements after treatment.
Descriptive statistics summarized participant characteristics. Linear regression models were used to determine if baseline infant distress to limitation predicted parent depressive symptoms at T2 and T3. Results were considered significant at P < .05, using RStudio for analysis.
Results
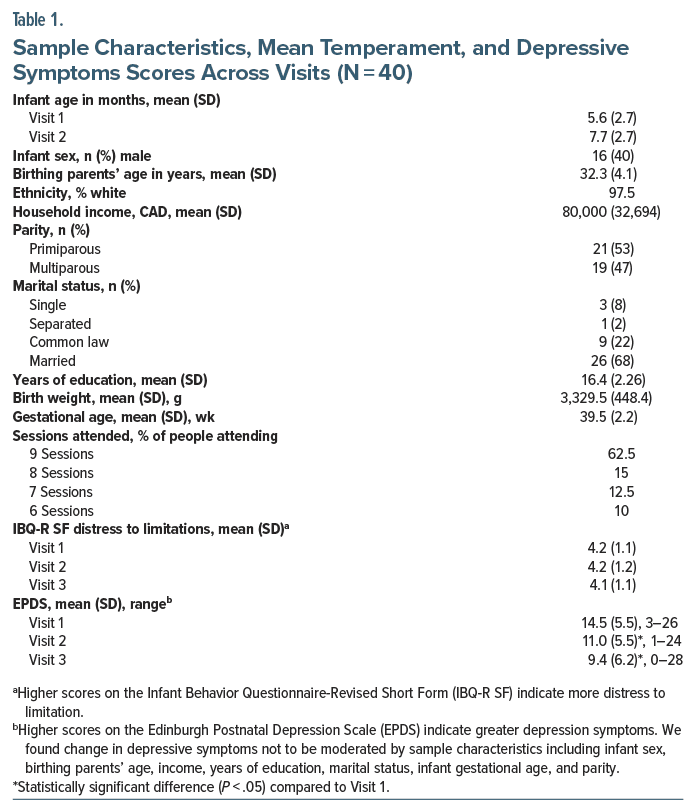
At T1, maternal age was 32.3 years, and infants were 5.6 months, all carried to term. Most participants were White, had a high school education or greater, and were married.
Paired samples t-tests showed a significant decrease in EPDS scores from T1 to T2 (P < .01) and T1 to T3 (P < .01) (See Table 1). Baseline infant distress did not correlate with baseline (T1) EPDS scores (R = 0.25, P = .14) but was associated with higher depression scores at T2 (β = 0.38, R = 0.38, P = .02) and T3 (β = 0.50, R = 0.49, P < .01). Results remained statistically significant after adjusting for parity, infant age marital status, and education, with no moderation by infant age.
Discussion
Higher infant distress to limitation predicted elevated PPD symptoms both at posttreatment and 3 months after treatment ended.
Distress to limitation heightens infant defiance6 and strains mother infant bonding,9,10 and caring for such temperaments can reduce parenting self-efficacy,15 leading to burnout.9 These challenges might have reduced parental engagement during CBT, limiting the use of learned strategies.
This study was comprised of mostly White, middle-class, married participants and lacked a control group, limiting generalizability and causal conclusions. Future research should use randomized controlled trials and larger, more diverse samples to examine how different temperamental subdomains affect parental treatment outcomes, including whether the effects of infant temperament on maternal post treatment symptoms are moderated by partner support and/or mediated by mother-infant bonding. The current study’s findings highlight the need to consider infant temperament’s impact on parental PPD treatment outcomes.
Article Information
Published Online: March 19, 2025. https://doi.org/10.4088/JCP.24br15503
© 2025 Physicians Postgraduate Press, Inc. J Clin Psychiatry 2025;86(2):24br15503
Submitted: July 24, 2024; accepted January 16, 2025.
To Cite: Yousefi Kousha K, Krzeczkowski JE, Van Lieshout RJ. The association between infant distress to limitation and postpartum depression treatment response. J Clin Psychiatry 2025;86(2):24br15503.
Author Affiliations: Faculty of Health Sciences, Department of Psychology, Neuroscience, and Behaviour, Neuroscience Graduate Program, McMaster University, Hamilton, Ontario, Canada (Kousha); Department of Health Sciences, Brock University, St. Catharines, Ontario, Canada (Krzeczkowski); Department of Psychiatry and Behavioural Neurosciences, McMaster University, Hamilton, Ontario, Canada (Van Lieshout).
Corresponding Author: Kian Yousefi Kousha, MSc, Faculty of Health Sciences, Department of Psychology, Neuroscience, and Behaviour, Neuroscience Graduate Program, McMaster University, 1280 Main St West, Hamilton, Ontario, Canada, L8S0A2 ([email protected]).
Relevant Financial Relationships: The authors report no potential conflict of interest.
Funding/Support: Funding was received from the Brain and Behavior Research Foundation: Grant #23595. Mr Kousha was funded by the CIHR’s Canada Graduate Scholarship. Dr Krzeczkowski was funded by the Government of Canada’s Vanier Graduate Program. Dr Van Lieshout is supported by the Canada Research Chairs program.
Role of the Funders: The funding sources had no involvement in the study design, collection, analysis, and interpretation of data; writing the manuscript; and the decision to submit the article for publication.
Previous Presentation: Results of the study were presented at The Centre for Addiction and Mental Health’s Womenmind Conference; April 2024; Toronto, Ontario, Canada.
Acknowledgment: The authors thank all participants for their contributions to this study.
References (15)

- Gavin NI, Gaynes BN, Lohr KN, et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Pt 1):1071–1083. PubMed CrossRef
- Racine N, Hetherington E, McArthur BA, et al. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry. 2021;8(5):405–415. CrossRef
- Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36(1):60–69. PubMed CrossRef
- MacQueen GM, Frey BN, Ismail Z, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 6. Special populations: youth, women, and the elderly. Can J Psychiatry. 2016;61(9):588–603.
- Rothbart MK. Measurement of temperament in infancy. Child Dev. 1981;52(2):569. CrossRef
- Lorber MF, Del Vecchio T, Slep AMS. Infant externalizing behavior as a self-organizing construct. Dev Psychol. 2014;50(7):1854–1861. PubMed CrossRef PubMed
- Radesky JS, Zuckerman B, Silverstein M, et al. Inconsolable infant crying and maternal postpartum depressive symptoms. Pediatrics. 2013;131(6):e1857–e1864. PubMed CrossRef
- Yim IS, Tanner Stapleton LR, Guardino CM, et al. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137. PubMed CrossRef
- Nolvi S, Karlsson L, Bridgett DJ, et al. Maternal postnatal psychiatric symptoms and infant temperament affect early mother-infant bonding. Infant Behav Dev. 2016;43:13–23. PubMed CrossRef
- Seifer R, Schiller M, Sameroff AJ, et al. Attachment, maternal sensitivity, and infant temperament during the first year of life. Dev Psychol. 1996;32(1):12–25. CrossRef
- Van Lieshout RJ, Yang L, Haber E, et al. Evaluating the effectiveness of a brief group cognitive behavioural therapy intervention for perinatal depression. Arch Womens Ment Health. 2017;20(1):225–228. PubMed CrossRef
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. PubMed CrossRef
- Putnam SP, Helbig AL, Gartstein MA, et al. Development and assessment of short and very short forms of the infant behavior questionnaire-revised. J Pers Assess. 2014;96(4):445–458. PubMed CrossRef
- Goldsmith HH, Lemery KS, Buss KA, et al. Genetic analyses of focal aspects of infant temperament. Dev Psychol. 1999;35(4):972–985. PubMed CrossRef
- Porter CL, Hsu HC. First-time mothers’ perceptions of efficacy during the transition to motherhood: links to infant temperament. J Fam Psychol. 2003;17(1):54–64. PubMed CrossRef
This PDF is free for all visitors!