The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), introduced a dissociative subtype of posttraumatic stress disorder (DS-PTSD), which is characterized by depersonalization and derealization, greater symptom complexity and comorbidity, and poorer engagement or response to standard trauma-focused therapies.1–4 A recent meta-analysis found that 48.1% (95% CI =35.0%–61.3%) of individuals with PTSD have DS-PTSD,2 suggesting that dissociative symptoms may be more central to PTSD than previously understood. Although veterans with dissociative symptoms have higher prevalence of co-occurring depression, anxiety, substance use, and suicidal thoughts and behaviors,3,4 DS-PTSD can often go undetected, as widely used self-report tools such as the PTSD Checklist for DSM-5 (PCL-5) do not assess dissociative symptoms.
Using data from a nationally representative sample of US veterans, we examined the prevalence and clinical characteristics of DS-PTSD. Based on prior literature,1–3 we hypothesized that approximately 50% of veterans with PTSD would have DS-PTSD and that veterans with DS-PTSD would report more traumas and higher levels of co-occurring depression and anxiety symptoms.
Methods
Sample. Data were analyzed from the National Health and Resilience in Veterans Study (NHRVS),6 which surveyed a nationally representative sample of 4,069 US veterans. Participants were drawn from Ipsos’ KnowledgePanel, a probability-based panel covering 98% of US households. Poststratification weights7 were applied in inferential analyses. The VA Connecticut Healthcare System Human Subjects Committee approved all procedures, and participants gave electronic informed consent.
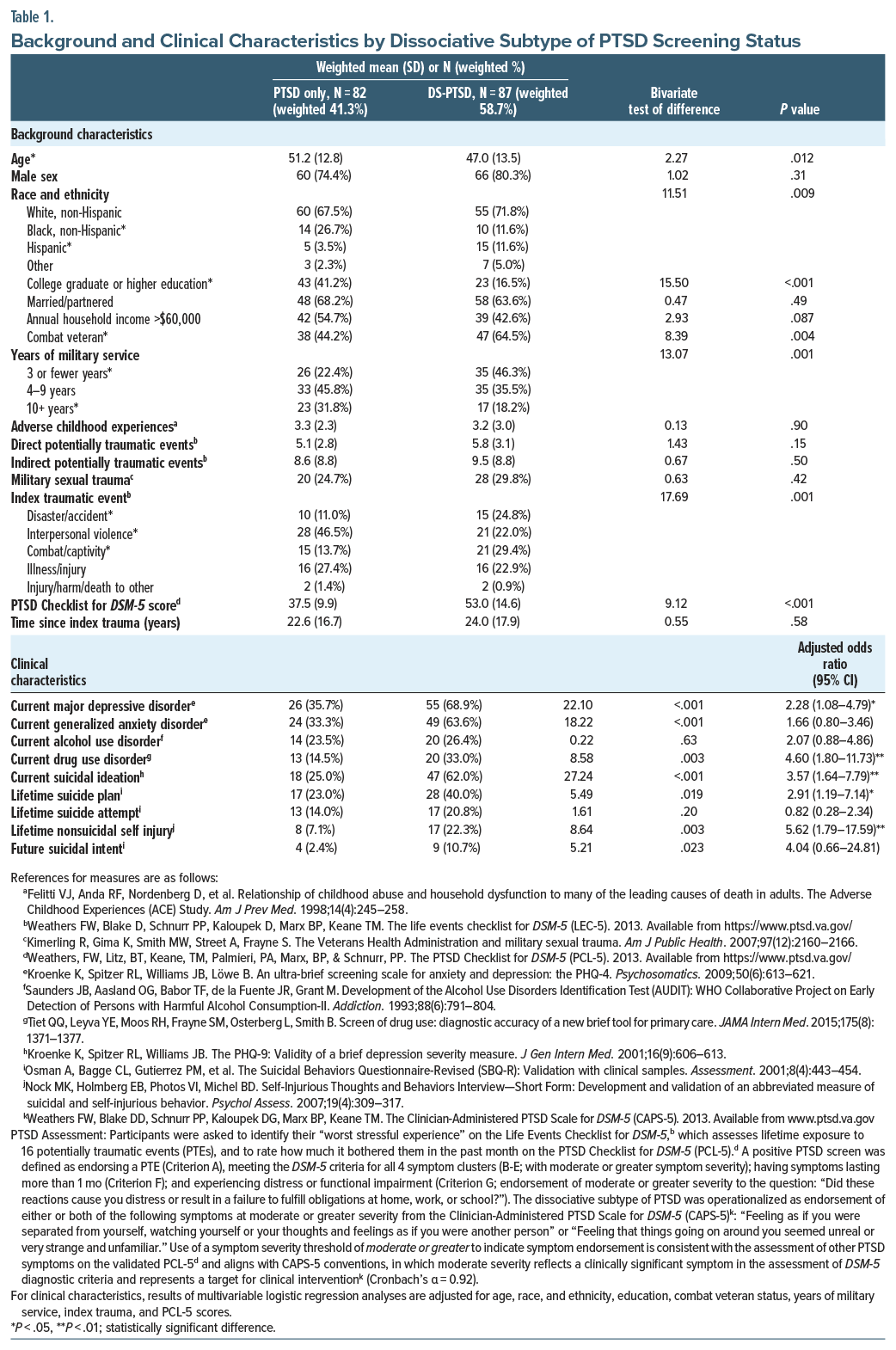
Measures. PTSD symptoms were assessed using a modified PCL-5,5,8 which included an assessment of dissociative symptoms using items from the Clinician-Administered PTSD Scale for DSM-5 (Table 1).
Data analysis. Independent-samples t tests and χ2 tests were used to compare sample characteristics by DS-PTSD status. Multivariable logistic regression analyses were conducted to examine associations between DS-PTSD status and clinical correlates while adjusting for relevant covariates.
Results
Of 169 veterans who screened positive for past-month PTSD, 87 (weighted 58.7%, 95% CI =48.4%–68.3%) screened positive for DS-PTSD. After adjusting for covariates, veterans with DS-PTSD had elevated odds of current major depressive and drug use disorders, suicidal ideation, and lifetime suicide plan and nonsuicidal self-injury (Table 1).
Discussion
In this nationally representative study, 58.7% of US veterans with current PTSD screened positive for DSM-5 DS-PTSD, consistent with the 48.1% (95% CI =35.0–61.3%) prevalence reported in a recent meta-analysis.2 Results corroborate prior work3,4 emphasizing the clinical significance of DS-PTSD, as those with this subtype of PTSD had markedly greater psychiatric burden.
DS-PTSD was associated with a 3-fold greater odds of lifetime suicide plan and current suicidal ideation, and 5-fold greater odds of lifetime nonsuicidal self-injury. Given that veterans have a 41%–61% higher suicide risk than civilians9 and accounted for 13% of suicides in 2022 despite representing only 6% of the population,10,11 these findings underscore the urgent need for routine screening for dissociative symptoms in veterans with PTSD, particularly those presenting with elevated suicide risk. Incorporating brief dissociation screeners into standard PTSD assessments may help identify high-risk individuals who could benefit from tailored treatment approaches that emphasize stabilization, grounding, and emotion regulation.2,4,12–15
Limitations of the study include its cross-sectional design, use of self-report measures and a nonvalidated assessment of dissociative symptoms, and potential limitations in generalizability to nonveteran populations. However, these limitations are offset by several strengths, including the use of a conservative, DSM-5–based assessment of PTSD and dissociative symptoms, and the recruitment of a nationally representative sample of veterans.
Overall, results of this study highlight the importance of assessing, monitoring, and treating dissociative symptoms in veterans with PTSD, as they are prevalent and linked to elevated psychiatric burden and suicide risk. Further research is warranted to refine screening tools and develop targeted interventions for DS-PTSD.
Article Information
Published Online: February 4, 2026. https://doi.org/10.4088/JCP.25br15977
© 2026 Physicians Postgraduate Press, Inc.
J Clin Psychiatry 2026;87(1):25br15977
Submitted: May 28, 2025; accepted December 18, 2025.
To Cite: Fogle BM, Fischer IC, Na PJ, et al. Dissociative subtype of posttraumatic stress disorder in US military veterans: prevalence, correlates, and clinical characteristics. J Clin Psychiatry 2026;87(1):25br15977.
Author Affiliations: University of Houston, Department of Psychology, Houston, Texas (Fogle); US Department of Veterans Affairs National Center for PTSD, VA Connecticut Healthcare System, West Haven, Connecticut (Fischer, Na, Pietrzak); Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut (Fischer, Na, Pietrzak); Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, Connecticut (Pietrzak).
Corresponding Author: Robert H. Pietrzak, PhD, MPH, National Center for PTSD, VA Connecticut Healthcare System, 950 Campbell Ave 151E, West Haven, CT 06516 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgments: The authors thank the veterans who participated in the National Health and Resilience in Veterans Study and the Ipsos staff who coordinated data collection.
References (15)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR. 5th ed. American Psychiatric Association Publishing; 2022.
- White WF, Burgess A, Dalgleish T, et al. Prevalence of the dissociative subtype of post-traumatic stress disorder: a systematic review and meta-analysis. Psychol Med. 2022;52(9):1629–1644. PubMed CrossRef
- Tsai J, Armour C, Southwick SM, et al. Dissociative subtype of DSM-5 posttraumatic stress disorder in U.S. veterans. J Psychiatr Res. 2015;66-67:67–74. PubMed CrossRef
- Herzog S, Fogle BM, Harpaz-Rotem I, et al. Dissociative symptoms in a nationally representative sample of trauma-exposed U.S. military veterans: prevalence, comorbidities, and suicidality. J Affect Disord. 2020;272:138–145. PubMed CrossRef
- Fischer IC, Na PJ, Harpaz-Rotem I, et al. Prevalence, correlates, and burden of subthreshold PTSD in US veterans. J Clin Psychiatr. 2024;85(4):24m15465. PubMed CrossRef
- Pietrzak RH, Levy BR, Tsai J, et al. Successful aging in older US veterans: results from the 2019–2020 National Health and Resilience in Veterans Study. Am J Geriatr Psychiatr. 2021;29(3):251–256. PubMed CrossRef
- US Census Bureau. Current Population Survey, Veterans Supplement; 2019. Accessed May 1, 2025. https://www2.census.gov/programs-surveys/cps/techdocs/cpsaug19.pdf
- Weathers FW, Litz BT, Keane TM, et al. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD; 2013.
- Kang HK, Bullman TA, Smolenski DJ, et al. Suicide risk among 1.3 million veterans who were on active duty during the Iraq and Afghanistan wars. Ann Epidemiol. 2015;25(2):96–100. PubMed CrossRef
- US Department of Veterans Affairs. 2024 National Veteran Suicide Prevention Annual Report. Office of Suicide Prevention. Accessed May 1, 2025. https://mentalhealth.va.gov/docs/data-sheets/2024/2024-Annual-Report-Part-2-of-2_508.pdf
- US Census Bureau. S2101: Veteran Status. 2022: ACS 1-Year Estimates Subject Tables. American Community Survey; 2022. Accessed May 1, 2025. https://data.census.gov/table/ACSST1Y2022.S2101?q=Veterans&y=2022
- Burton MS, Feeny NC, Connell AM, et al. Exploring evidence of a dissociative subtype in PTSD: baseline symptom structure, etiology and treatment efficacy for those who dissociate. J Consult Clin Psychol. 2018;86(5):439–451. PubMed CrossRef
- Jarkas DA, Robillard R, Malenfant C-R, et al. Exploring the dissociative subtype of PTSD: the role of early-life trauma, cortisol, and inflammatory profiles. Psychoneuroendocrinology. 2025;175:107406. PubMed CrossRef
- Wolf EJ, Hawn SE, Sullivan DR, et al. Neurobiological and genetic correlates of the dissociative subtype of posttraumatic stress disorder. J Psychopathol Clin Sci. 2023;132(4):409–427. PubMed CrossRef
- Vancappel A, Chavigny C, Chami L, et al. Group dissociation-focused cognitive behavioral therapy (DF-CBT) in patients suffering from a dissociative subtype of PTSD: an exploratory study. J Trauma Dissociation. 2024:1–16. PubMed CrossRef
This PDF is free for all visitors!