Prescription opioids1 and benzodiazepines2 are each associated with health risks, which are heightened when the 2 are used concurrently.3 The Centers for Disease Control and Prevention recommends caution when coprescribing these medications.4 Still, little is known about the early warning signs, such as nonmedical use (NMU) and substance use disorder (SUD) symptoms, that often precede overdose and injuries. This study examined NMU and SUD symptoms among US adults prescribed opioids and benzodiazepines.
Methods
Longitudinal data were from 22 nationally representative cohorts of US 12th graders (N=53,679; baseline years 1976–1997) followed prospectively through adulthood in the Monitoring the Future Panel study (retention rate=51.0%).5 Between ages 40–60 (follow-up years 1998–2019), participants were surveyed at 5-year intervals. The analytic sample for SUDs included respondents aged 40–55 for follow-up years 2007–2016. The analytic sample for NMU included respondents aged 40–60 for follow-up years 2007–2019.
Surveys assessed medical use of prescription opioids (ie, “narcotics other than heroin”) and benzodiazepines (ie, “tranquilizers”), with examples of generic and brand name medications provided. A 4-category variable was constructed to indicate past-5-year medical use of (1) neither opioids nor benzodiazepines (ie, population controls), (2) opioids only, (3) benzodiazepines only, or (4) both opioids and benzodiazepines (ie, co-use).
Respondents reported past-5-year NMU of opioids or benzodiazepines (ie, “without a doctor telling you to take them”). Past-5-year SUD symptoms were measured using 8 DSM-IV and DSM-5 criteria (failure to fulfill role obligations, use in physically hazardous situations, social/ interpersonal problems, tolerance, withdrawal, desire to cut down, physical/psychological problems, cravings). For consistency with DSM-5 SUD recommendations, ≥2 alcohol, ≥2 cannabis, or ≥2 other drug use criteria were independently coded; ≥2 symptoms for at least 1 substance indicated multiple SUD symptoms.
Analyses were weighted for sampling and attrition. Missing data were handled using listwise deletion. Logistic regression models with clustering at the individual level to account for repeated measures were fitted to assess within-wave associations of medical use with NMU and SUD symptoms, controlling for relevant covariates.
Results
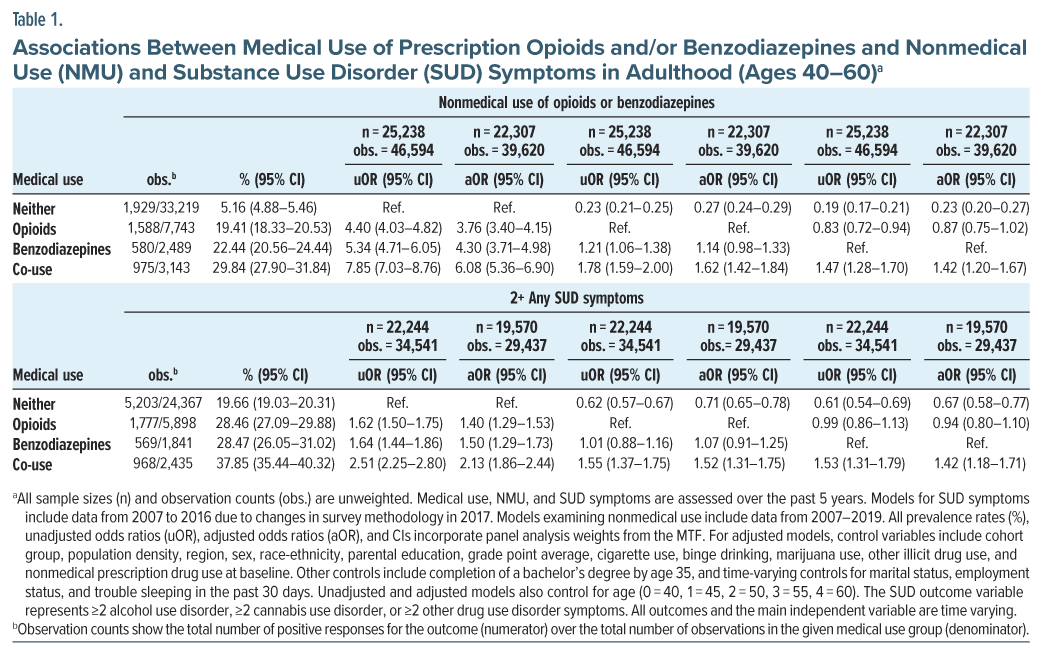
Participants were 50.7% female and 76.8% White, 10.8% Black, 6.1% Hispanic, and 6.2% another race-ethnicity. One-third (38.6%; 95% CI, 38.0%–39.2%) reported past-5-year medical use of prescription opioids or benzodiazepines, and 10.4% (95% CI, 10.0%–10.7%) reported co-use (Supplementary Table 1). Adults who used opioids and benzodiazepines had greater adjusted odds of NMU and SUD symptoms relative to population controls (Table 1). Adults with co-use had greater adjusted odds of NMU relative to those who used opioids only (adjusted odds ratio [aOR = 1.62, 95% CI, 1.42-1.84]) and benzodiazepines only (aOR = 1.42, 95% CI, 1.20–1.67). Similarly, adults with co-use had greater adjusted odds of SUD symptoms relative to those who used opioids only (aOR = 1.52, 95% CI, 1.31-1.75) and benzodiazepines only (aOR = 1.42, 95% CI, 1.18–1.71). A sensitivity analysis assessed past-year medical and NMU, and results were substantively the same (Supplementary Table 2). SUD results held when examining other drug use disorder symptoms only (Supplementary Tables 3–4).
Discussion
Despite increased attention to the risks associated with concurrent use of opioids and benzodiazepines,4 coprescribing remains a concern.6 While most adults with co-use reported no NMU, they demonstrated increased odds of NMU and SUD symptoms relative to those prescribed opioids only, benzodiazepines only, and population controls. Early detection of NMU and SUD symptoms is critical for preventing overdose and related harms. Study limitations include self-report bias and measurement constraints. SUD symptoms were assessed using 8 of 11 SUD criteria, which likely underestimated the prevalence of SUD. Future research should employ more frequent data collection intervals to clarify temporality and examine how associations between co-use and NMU and SUD have shifted over time. Findings indicate a need to carefully counsel, screen, monitor, and treat adults prescribed opioids and benzodiazepines, particularly in combination, for comorbid SUD.
Article Information
Published Online: September 8, 2025. https://doi.org/10.4088/JCP.25br15937
© 2025 Physicians Postgraduate Press, Inc.
J Clin Psychiatry 2025;86(4):25br15937
Submitted: April 28, 2025; accepted June 23, 2025.
To Cite: Pasman E, Veliz P, Hoffman E, et al. Nonmedical use and substance use disorder symptoms among US adults co-prescribed opioids and benzodiazepines. J Clin Psychiatry 2025;86(4):25br15937.
Author Affiliations: Jane Addams College of Social Work, University of Illinois Chicago, Chicago, Illinois (Pasman); Center for the Study of Drugs, Alcohol, Smoking and Health, University of Michigan, Ann Arbor, Michigan (Pasman, Veliz, Hoffman, Evans-Polce, Schepis, Patrick, Truchan, Wilens, Jardine, V. McCabe, S. McCabe); Institute for Social Research, University of Michigan, Ann Arbor, Michigan (Veliz, Evans-Polce, Patrick, S. McCabe); Institute for Research on Women and Gender, University of Michigan, Ann Arbor, Michigan (Veliz, S. McCabe); Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor, Michigan (Veliz, S. McCabe); Department of Psychiatry, University of Michigan, Ann Arbor, Michigan (Hoffman, V. McCabe); Department of Psychology, Texas State University, San Marcos, Texas (Schepis); Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts (Wilens); Harvard Medical School, Harvard University, Boston, Massachusetts (Wilens).
Corresponding Author: Emily Pasman, PhD, Jane Addams College of Social Work, University of Illinois Chicago, 1040 W. Harrison St, Chicago, Illinois 60607 ([email protected]).
Relevant Financial Interests: Dr. Wilens reported receiving grant funding from 3D Therapeutics during the conduct of the study; serving as a consultant for 3D Therapeutics, the Gavin Foundation, Bay Cove Human Services, US Minor League Baseball, and US Major League Baseball outside the submitted work; having a shared IP with 3D Therapeutics and Mass General Brigham for a product unrelated to the current study; and receiving royalties from Guilford Press and Cambridge University Press outside the submitted work. No disclosures were reported by the other authors.
Funding/Support: This study was supported by research awards from the National Institute on Drug Abuse (NIDA) of the National Institute of Health (NIH) (R01DA031160, R01DA001411, and R01DA016575).
Role of the Sponsor: NIH/NIDA had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Information: Monitoring the Future Panel data are available through the National Addiction and HIV Data Archive Program at https://www.icpsr.umich.edu/web/NAHDAP/series/2520.
Supplementary Material: Available at Psychiatrist.com.
References (6)

- Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a national Institutes of Health Pathways to Prevention workshop. Ann Intern Med. 2015;162(4):276–286. PubMed CrossRef
- Edinoff AN, Nix CA, Hollier J, et al. Benzodiazepines: uses, dangers, and clinical considerations. Neurol Int. 2021;13(4):594–607. PubMed CrossRef
- Boon M, Van Dorp E, Broens S, et al. Combining opioids and benzodiazepines: effects on mortality and severe adverse respiratory events. Ann Palliat Med. 2020;9(2):542–557. PubMed CrossRef
- Dowell D, Ragan KR, Jones CM, et al. CDC clinical practice guideline for prescribing opioids for pain - United States, 2022. MMWR Recomm Rep. 2022;71(3):1–95. PubMed CrossRef
- Patrick ME, Miech RA, Johnston LD, et al. Monitoring the Future Panel Study Annual Report: National Data on Substance Use among Adults Ages 19 to 65, 1976–2023. University of Michigan; 2024. https://monitoringthefuture.org/results/annual-reports/
- Taha SA, Westra JR, Tacker DH, et al. Trends in co prescribed opioids and benzodiazepines, non prescribed opioids and benzodiazepines, and schedule-I drugs in the United States, 2013–2019. Prev Med Rep. 2024;38:102584. PubMed CrossRef
This PDF is free for all visitors!