After more than 50 years, a global initiative has picked up momentum in its bid to transform the way we look at traumatic brain injuries (TBIs). This new proposal includes an updated assessment protocol that leaves the legacy Glasgow Coma Scale (GCS) behind in favor of a more nuanced approach.
Historically, clinicians have rated the severity of a TBI using the GCS. It’s a scale that scores a patient’s level of consciousness from 3 to 15.
- 13-15 – Mild.
- 9-12 – Moderate.
- 3-8 – Severe.
But a growing segment of academics and clinicians claim that this system suffers from serious shortcomings, such as:
- It oversimplifies just how complicated that brain injuries can be.
- It depends on a single clinical indicator.
- And the scoring system can stigmatize patients based on labels that don’t necessarily (or even reliably) predict recovery.
“There are patients diagnosed with concussion whose symptoms are dismissed and receive no follow-up because it’s ‘only’ a concussion, and they go on to live with debilitating symptoms that destroy their quality of life,” corresponding author Geoffrey Manley, MD, PhD, professor of neurosurgery at UC San Francisco and a member of the UCSF Weill Institute for Neurosciences, said. “On the other hand, there are patients diagnosed with ‘severe TBI’ who were eventually able to live full lives after their families were asked to consider removing life-sustaining treatment.”
Frustrated with these constraints, the U.S. National Institute of Neurological Disorders and Stroke (NINDS) launched a plan in 2022 to overhaul how clinicians characterize acute TBIs. The project brought together nearly 100 experts from more than a dozen countries to draft this new system.
So, they developed the “CBI-M framework,” a model that integrates four separate assessment pillars: Clinical, Biomarker, Imaging, and Modifier.
A New Framework
“The proposed framework marks a major step forward,” co-senior author Michael McCrea, PhD, professor of neurosurgery and co-director of the Center for Neurotrauma Research at the Medical College of Wisconsin in Milwaukee, explained. “We will be much better equipped to match patients to treatments that give them the best chance of survival, recovery, and return to normal life function.”
- Clinical Pillar: This component retains the GCS while adding other elements, such as pupillary reactivity, post-traumatic amnesia, and symptom assessments. While the GCS remains crucial, the new framework discourages summarizing it into simplified categories. Instead, it promotes detailed documentation of the scale’s three components: eye, verbal, and motor responses. “This pillar should be assessed as first priority in all patients,” said co-senior author Andrew Maas, MD, PhD, emeritus professor of neurosurgery at the Antwerp University Hospital and University. “Research has shown that the elements of this pillar are highly predictive of injury severity and patient outcome.”
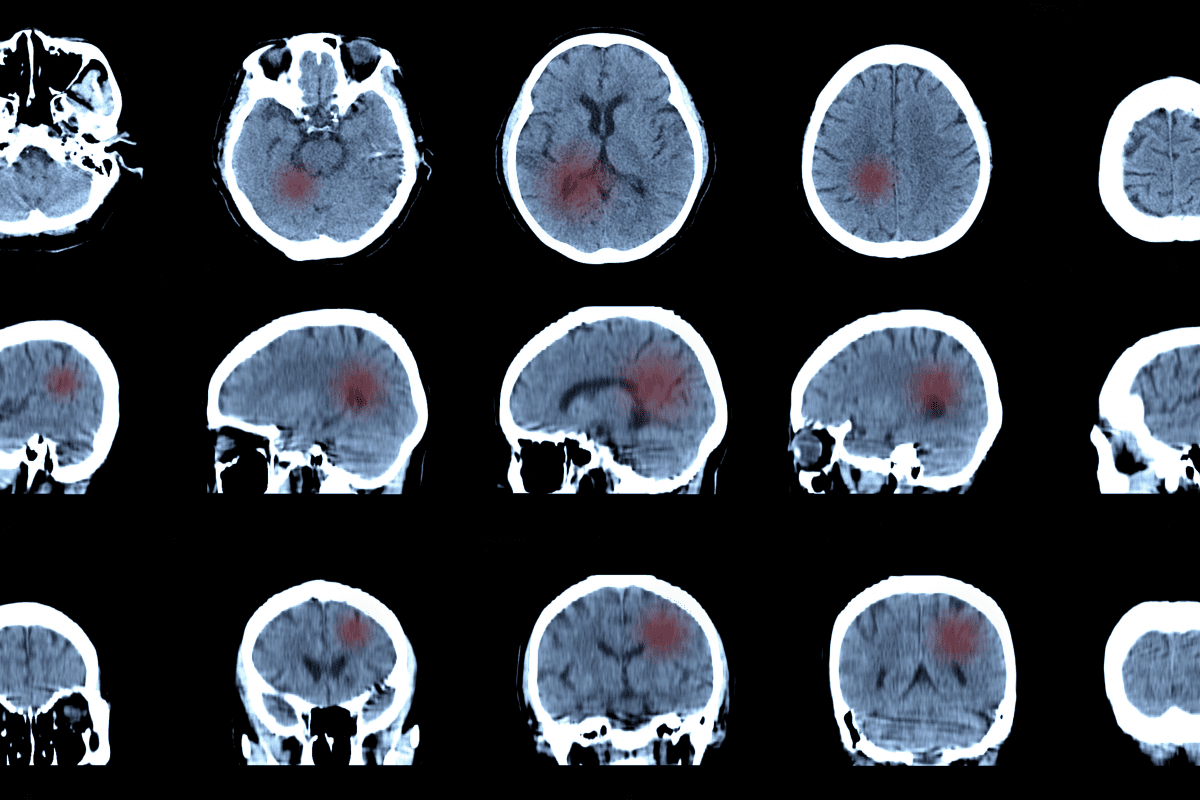
- Biomarker Pillar: Leveraging advances in blood-based diagnostics, this leg of the proposed protocol recommends early analysis of glial fibrillary acidic protein (GFAP), ubiquitin C-terminal hydrolase L1 (UCH-L1), and S100B levels. These biomarkers can signal the presence and severity of brain injury. Even when the CT scans appear normal. “In the past, we couldn’t tell the difference between a knock on the head and a TBI,” Manley added. “Thanks to biomarkers, we can make this distinction and ensure that it’s the TBI patient who enrolls in the trial.”
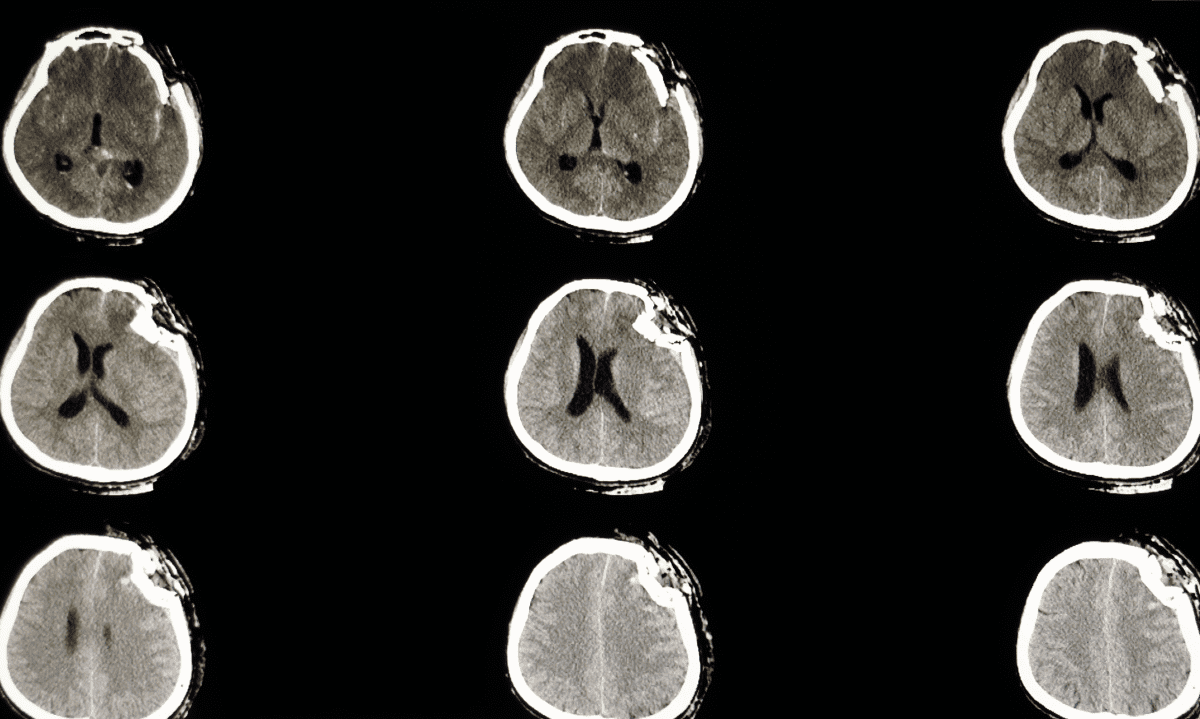
- Imaging Pillar: This aspect of the new proposal focuses on common CT abnormalities, including skull fractures, subarachnoid hemorrhaging, and subdural hematomas. It also introduces a new term – “traumatic axonal” or “microvascular injury” – to better articulate findings that once fell under the category of “diffuse axonal injury.” (It’s worth noting that this pillar relies on the integration of structured reporting in electronic medical records.)
- Modifier Pillar: The most novel component of the revamped classification system considers psychosocial and environmental factors that help shape injury outcomes, such as age, gender, comorbidities, and socioeconomic status. These elements play a crucial role in forecasting long-term recovery while addressing disparities in care. “This pillar summarizes the factors that research tells us need to be considered when we interpret a patient’s clinical, blood biomarker, and neuroimaging exams,” said co-first author Kristen Dams-O’Connor, PhD, professor of rehabilitation and human performance, and neurology, at the Icahn School of Medicine at Mount Sinai in New York. “One example is a patient with underlying cognitive impairment, who may require acute monitoring for risk of clinical deterioration, regardless of findings on the initial clinical exam.”
Addressing Gaps and Charting Future Research
The CBI-M framework marks a huge pivot from the static labels of the past toward a more dynamic, personal approach. But its authors conceded that implementation will take time and planning. The model’s flexibility – which allows it accommodate a wide range of TBIs – remains under investigation. The researchers add that more data could validate this while affirming the cost-effectiveness of its biomarker components.
Others are also working on plans to assimilate the model into clinical and research settings. Implementation efforts will demand targeted outreach, professional training, and electronic health record systems upgrades. Researchers are also working to ensure this can serve places that might not have access to advanced imaging or testing.
This initiative builds on more than two decades of research, including efforts to standardize data collection and integrate bioinformatics. But it also reflects a growing recognition that effective care must consider more than just the initial injury. It must keep in mind the broader context of recovery.
Further Reading
Could Our Brains Be Steering Our Politics?