This week, we hear a critique of a recent FDA panel on antidepressant use during pregnancy and cover the latest salvo in the competition between ketamine and esketamine.
Experts Warn Misinformation Fuels Stigma, Risks
A recent U.S. Food and Drug Administration (FDA) panel on antidepressant use in pregnancy has sparked sharp criticism from experts who claim that it spreads misinformation while reinforcing lingering stigma around mental illness.
Writing in the Journal of Clinical Psychiatry, reproductive psychiatrist Jennifer L. Payne, MD, of the University of Virginia warned that the July 2025 gathering lacked perinatal mental health expertise. It also featured panelists who questioned the validity of major depressive disorder (MDD) itself.
Instead of addressing the real risks and benefits of psychiatric treatment during pregnancy, Payne argues, panelists conflated everyday sadness with clinical depression and dismissed evidence of MDD’s biological underpinnings.
One speaker claimed depression had “no operational definition,” ignoring the clear criteria set forth in the “Diagnostic and Statistical Manual of Mental Disorders.”
Another asserted that mental health conditions lack pathophysiology, despite substantial evidence of genetic, neuroimaging, and biomarker-based correlates.
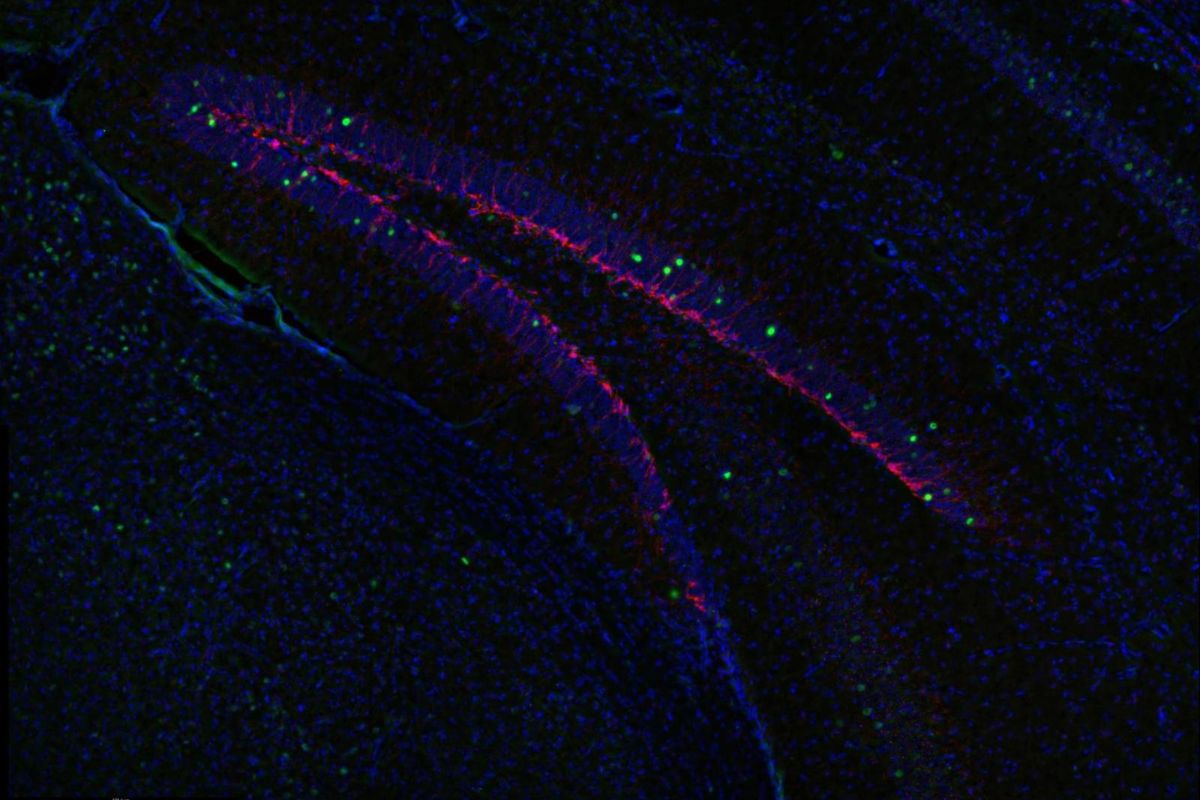
Payne emphasized that untreated depression carries serious risks for both mother and baby. Postpartum depression, which affects up to 15% of new mothers, offers a unique glimpse of MDD’s biology. Earlier studies have identified predictive biomarkers, disrupted cellular recycling processes, and neuroactive steroid changes that influence stress response.
Such findings, she noted, demonstrate the disorder’s biological roots and pave the way for more targeted therapies. Dismissing these realities, Payne warned, fuels stigma, delays treatment, and ultimately harms families.
“Precision in how we discuss major depression matters,” she concluded, urging policymakers to ground decisions in evidence rather than ideology.
IN OTHER PSYCHIATRY AND NEUROLOGY NEWS
- In a promising first, a 19-year-old woman with Turner syndrome and clozapine-resistant schizophrenia achieved stable relief from years of refractory auditory hallucinations through maintenance electroconvulsive therapy.
- A JCP commentary argues that clinicians remain uncertain whether ketamine or esketamine is more effective for treatment-resistant depression, even though esketamine is considered safer.
- In a letter to the editor, researchers propose that naltrexone might help treat prolonged grief disorder by targeting the brain’s reward system, though its use raises debate over medicalizing grief.
- A risk-benefit analysis in JCP found that adding bupropion to antidepressant therapy generally outperforms switching or augmenting with aripiprazole for treatment-resistant depression.
- Finally, catch the last (for now) installment of our yearlong look into “Emerging Approaches in Schizophrenia.”