Prim Care Companion CNS Disord 2022;24(4):21br03156
To cite: Mansuri Z, Patel K, Parekh T, et al. Frequency of psychiatric disorders in adult patients hospitalized with marital problems. Prim Care Companion CNS Disord. 2022;24(4):21br03156.
To share: https://doi.org/10.4088/PCC.21br03156
© 2022 Physicians Postgraduate Press, Inc.
aDepartment of Psychiatry, Boston Children’s Hospital/Harvard Medical School, Boston, Massachusetts
bAvalon University School of Medicine, Willemstad, Curaçao, Netherlands Antilles
cDepartment of Health Administration and Policy, George Mason University, Fairfax, Virginia
dDepartment of Psychiatry, Texas Tech University Health Science Center at Odessa/Permian Basin, Odessa, Texas
eDepartment of Epidemiology, New York University, New York, New York
fDepartment of Psychiatry, Brookdale University Hospital Medical Center, Brooklyn, New York
gDepartment of Psychiatry, The University of Texas Rio Grande Valley, Harlingen, Texas
hDepartment of Psychiatry, Virginia Tech Carilion School of Medicine, Roanoke, Virginia
iDepartment of Psychiatry, Penn State Health Hershey Medical Center, Hershey, Pennsylvania
‡Drs Mansuri and Patel share equal contributions as first authors. Drs Reddy and Baweja share equal contributions as senior authors.
*Corresponding author: Zeeshan Mansuri, MD, MPH, Boston Children’s Hospital/Harvard Medical School, 300 Longwood Ave, Boston, MA 02115 ([email protected]).
Marriage is acknowledged as a demographic factor associated with both mental and physical health. It has been shown that married individuals have a longer life expectancy, lower death rates and self-reported morbidity, and better psychological well-being than those who are unmarried.1 Although studies on marriage and mental health tend to focus on the average effect of marriage, the positive association may not hold across different contexts, particularly for marital problems. For instance, research has shown that low-quality, long-term marriages have significant negative effects on health.2 However, to our knowledge, studies have not investigated the burden of psychiatric disorders and substance abuse in individuals hospitalized with marital problems. Our research evaluated trends in US hospitalizations with psychiatric disorders and substance abuse with marital problems from 2007 to 2014.
METHODS
Weighted discharges from the largest nationwide inpatient database, the National Inpatient Sample (NIS) (2007–2014), were queried addressing over 95% of the US inpatient population. The NIS contains approximately 8 million annual discharges from over 1,050 hospitals, which represents a 20% stratified sample of all nonfederal acute care hospitals from 45 states, excluding long-term care and rehabilitation facilities.3 Adult patients with a history of marital problems were identified using ICD-9 CM codes V61.1x (counseling for marital and partner problems and spousal/partner abuse), V61.03 (family disruption due to divorce), and V61.04 (estrangement). From those without a history of marital problems, a 1:2 sample of controls was selected. Trends in psychiatric comorbidities were analyzed utilizing previously used codes.4 Categorical variables were compared using the χ2 test in SPSS v24.0 (IBM, Armonk, New York). P < .05 was considered clinically significant.
RESULTS
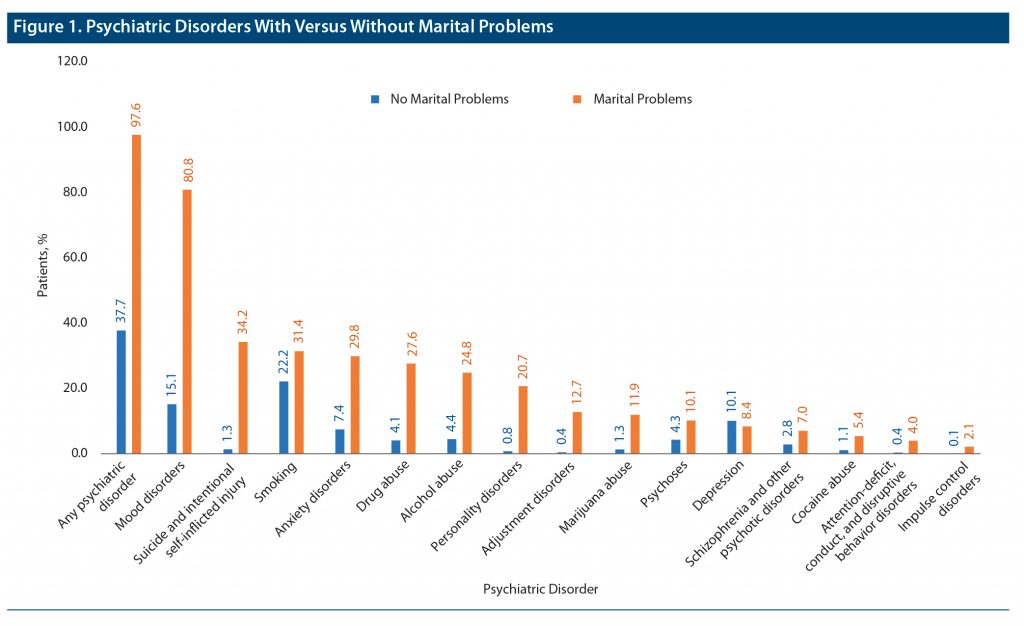
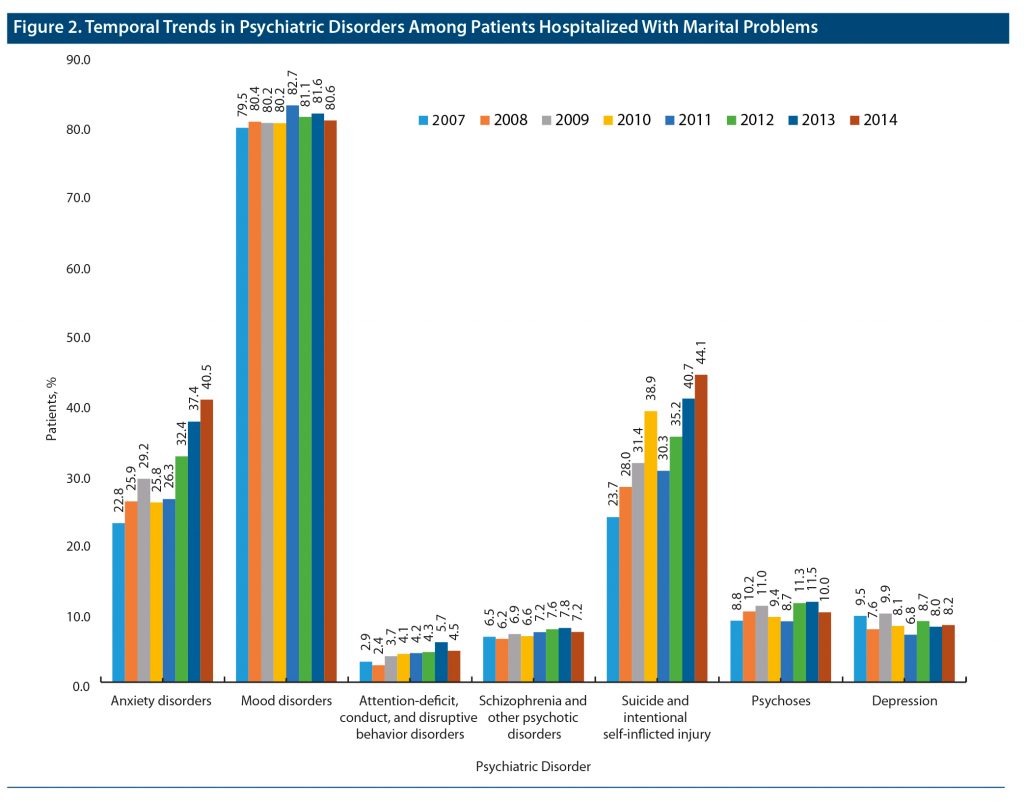
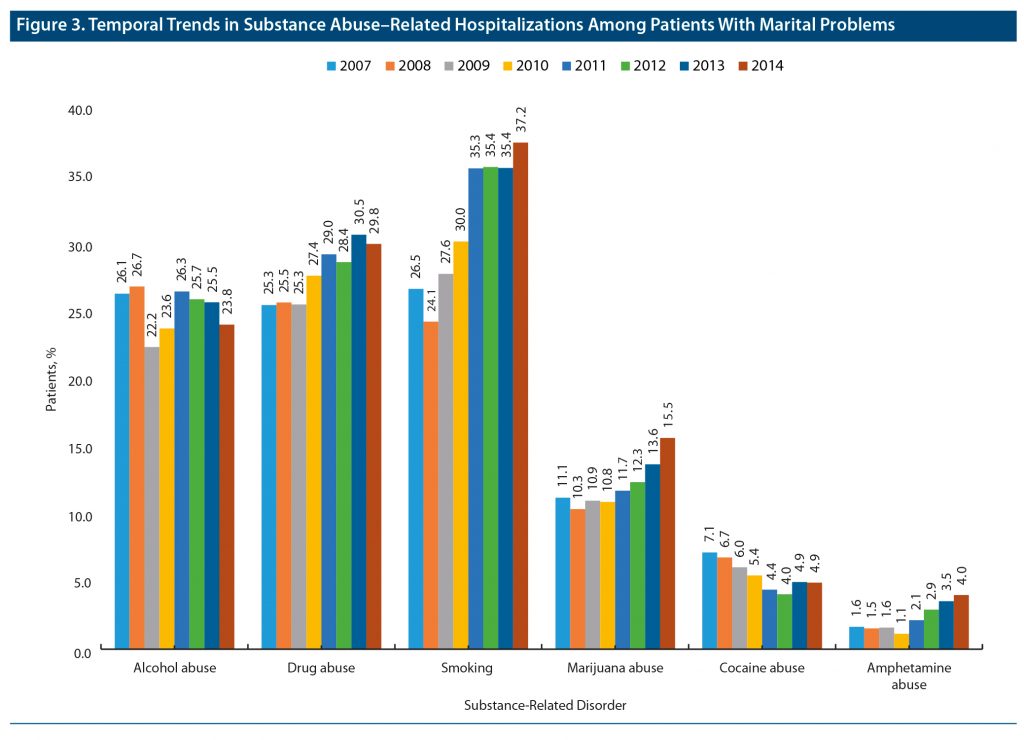
Hospitalized adult patients who had marital problems (n = 120,990, 55.6% female) were more likely to be younger (18–44 years: 67% vs 29.8%, P < .001), male (44.4% vs 40.2%, P < .001), and White (79.8% vs 68.3%, P < .001); had private insurance coverage (44.6% vs 29.8%, P < .001) or self-pay/no-pay beneficiaries (21.40% vs 9.20%, P < .001); and belonged to the Midwest and Northeast regions compared to those without marital problems (n = 241,924). Figure 1 shows the prevalence of psychiatric disorders with marital problems compared to those without marital problems. The data showed that 97.6% of patients with marital problems had psychiatric disorders. Mood disorder was the most prevailing disorder (80.8%), followed by suicide/self-inflicted injury (34.2%), smoking (31.4%), and anxiety disorders (29.8%). From 2007 to 2014, the rate of screening and history of mental health and substance abuse in patients hospitalized with marital problems increased from 30.4% to 46.0%, whereas the anxiety rate increased from 22.8% to 40.5%, and suicide and the self-inflicted injury rate increased from 23.7% to 44.4% (Figure 2). Figure 3 shows the temporal trend of an increased burden of substance abuse (smoking: 26.5%–37.2%, drug abuse: 25.3%–29.8%, marijuana abuse: 11.1%–15.5%, and amphetamine abuse: 1.6%–4.0%) from 2007 to 2014 in patients hospitalized with a marital problem.
DISCUSSION
This study provides first-ever evidence of hospitalization rates for psychiatric disorders and substance abuse in individuals with marital problems. Historical data also indicate the rising need for health care in the context of the relationship between marriage and health.5 Individuals who reported having marital problems exhibited an overall significant burden of psychiatric disorders. One possible explanation could be that mental health issues and subsequent hospitalizations result in strain on marital life. Another explanation is that individuals experiencing marital problems can have subsequent worsening of mental health issues due to added stress. Furthermore, the alarming rise in suicide and self-inflicted injury along with marijuana and amphetamine abuse requires special attention and highlights the need to improve marital well-being.
The study’s focus on primary diagnoses minimized misclassification. However, we may have missed cases of hospitalizations due to secondary diagnoses. Furthermore, it is unclear how marital problems lead to hospitalization. Nevertheless, future research is warranted for marital health checkup by investigating the association between various marital characteristics and other potential risk factors for psychiatric conditions leading to hospitalizations.
Submitted: September 26, 2021; accepted January 19, 2022.
Published online: August 18, 2022.
Relevant financial relationships: None.
Funding/support: None.
References (5)

- Wyke S, Ford G. Competing explanations for associations between marital status and health. Soc Sci Med. 1992;34(5):523–532. PubMed CrossRef
- Hawkins DN, Booth A. Unhappily ever after: effects of long-term, low-quality marriages on well-being. Soc Forces. 2005;84(1):451–471. CrossRef
- HCUP Databases. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality website. Rockville, MD. Accessed June 22, 2022. www.hcup-us.ahrq.gov/nisoverview.jsp
- Becerra BJ, Banta JE, Ghamsary M, et al. Burden of mental illness on hospital and patient outcomes among asthma hospitalizations. J Asthma. 2016;53(4):392–397. PubMed CrossRef
- Somers AR. Marital status, health, and use of health services. an old relationship revisited. JAMA. 1979;241(17):1818–1822. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!