Brain magnetic resonance imaging (MRI) is essential in the process of dating and staging cerebral ischemic lesions.1–4 Classical findings include restriction in diffusion-weighted sequences. Characteristic patterns are also found in other sequences, such as contrast-enhanced T1-weighted.3 Usually 3 types of contrast enhancement are described: intravascular, meningeal, and parenchymal.3 While intravascular enhancement is occasionally seen in the acute phase when there is vessel occlusion, parenchymal enhancement usually occurs during the subacute phase.4 Interpretation of imaging findings may prove challenging when there is an unclear history or atypical symptoms.
Case Report 1
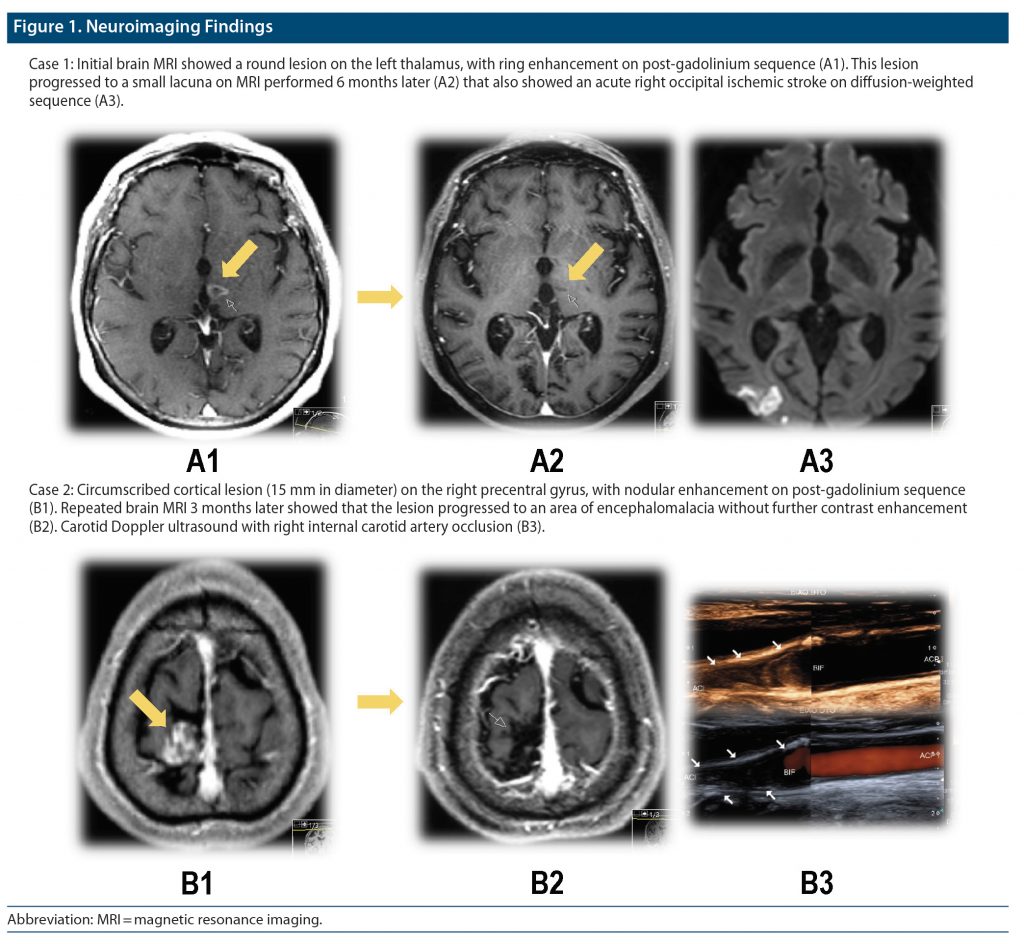
An 80-year-old woman presented new-onset bilateral horizontal diplopia and gait instability. She had a past medical history of hypertension and diabetes mellitus type 2. Timing of symptom onset was unclear. Brain computed tomography (CT) revealed a left thalamic round lesion. MRI (first week of admission) showed no evidence of restriction on diffusion-weighted sequences but showed contrast enhancement on contrast-enhanced T1-weighted sequence (Figure 1). Considering the possibility of brain metastasis, the patient was referred to the oncology department for a full diagnostic workup and was started on dexamethasone (15 mg/d). Six months later, the patient presented acute confusion and left homonymous hemianopsia. MRI showed evidence of an acute ischemic stroke in the right posterior cerebral artery territory. The previous thalamic lesion had evolved to a small lacuna. After detection of atrial fibrillation, the patient was started on anticoagulation therapy.
Case Report 2
A 60-year-old man was admitted to the hospital due to brief episodes of involuntary movements of his left foot. His medical history revealed several cardiovascular risk factors (smoker, hypertension, diabetes mellitus type 2) and HIV infection (CD4 cell count > 250 cell/mm3). Brain CT was unremarkable. The patient was started on levetiracetam (2 g/d) following a presumptive diagnosis of focal motor seizures. MRI (3 weeks after symptom onset) revealed a cortical round lesion in the right precentral gyrus (15 mm in diameter) without vasogenic edema—hyperintense on T2, fluid-attenuated inversion recovery, and post-gadolinium without restricted diffusion (Figure 1). Due to possible opportunistic infection, a lumbar puncture was performed, and the patient was started on empirical antibiotics and antiviral and antifungal medication. Laboratory results were all negative. Electroencephalogram revealed right frontal epileptogenic activity that remitted with antiepileptic therapy. A follow-up brain MRI 3 months later revealed that the lesion progressed to an area of encephalomalacia without contrast enhancement. Vascular studies revealed right internal carotid artery occlusion that had been detected in the first MRI. The patient successfully underwent carotid endarterectomy.
Discussion
Although both patients presented cardiovascular risk factors, presentation and neuroimaging findings were less typical of acute stroke. In case 1, there was uncertainty about the onset of the symptoms. In case 2, paroxysmal episodes with history of HIV suggested a possible secondary infection. Imaging findings consisted of lesions without restricted diffusion or a clearly defined vascular territory with the presence of contrast enhancement. Contrast-enhancement patterns in brain ischemic lesions may result from vessel occlusion, flow impairment, disturbance of the blood-brain barrier, altered local hemodynamics, and luxury perfusion.2–4 While arterial and meningeal enhancement appear early during the first week after stroke, parenchymal enhancement usually begins in the second week, around the time when collateral flow is established and immature capillaries of granulation tissue allow contrast accumulation in the area.2,3 After 8–12 weeks, contrast enhancement is undetectable, and other causes should be considered.2 During the subacute phase, enhancement occurs when diffusion-weighted imaging may be normal due to pseudonormalization of the diffusion coefficient.4 Infarct enhancement can be heterogeneous, sometimes showing bizarre parenchymal patterns, further complicating the diagnosis.4 Parenchymal enhancement may lead to misdiagnosis with future deleterious outcomes, delaying an adequate approach to the underlying cerebrovascular disease. There is a lack of knowledge about the normal presence of contrast enhancement in ischemic lesions. Moreover, contrast is not part of typical MRI stroke protocols. Our report highlights the normal presence of contrast enhancement in the subacute phase of ischemic stroke that can be misleading without the knowledge of different contrast-enhancement patterns in these lesions.
Article Information
Published Online: June 20, 2023. https://doi.org/10.4088/PCC.22cr03422
© 2023 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord. 2023;25(3):22cr03422
To Cite: Oliveira R, Mendonça M, Teodoro T, et al. Revisiting magnetic resonance imaging gadolinium contrast enhancement in subacute cerebral infarction: two cases leading to misdiagnosis. Prim Care Companion CNS Disord. 2023;25(3):22cr03422.
Author Affiliations: Department of Neurology and Headache Centre, Hospital da Luz Lisboa, Lisbon, Portugal (Oliveira); Department of Neurosciences and Mental Health, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, Portugal (Oliveira); CHRC–Health Research Centre, NOVA University Lisbon, Portugal (Oliveira, Teodora); Department of Neuroimaging, Hospital de Santa Maria, Centro Hospitalar Lisboa Norte, Lisbon, Portugal (Mendonça, Morgado); Centro Hospitalar Psiquiátrico de Lisboa, Lisbon, Portugal (Teodoro); Adult ADHD and Neurodevelopmental Disorders Outpatient Service, Centro Hospitalar Psiquiátrico de Lisboa, Lisbon, Portugal (Teodoro); Department of Imaging, Faculdade de Medicina, Universidade de Lisboa, Lisbon, Portugal (Morgado).
Corresponding Author: Renato Oliveira, MD, MSc, Department of Neurology, Hospital da Luz Lisboa, Avenida Lusíada 100, 1500-650 Lisbon, Portugal ([email protected]).
Relevant Financial Relationships: None.
Funding source/support: None.
Patient Consent: Consent was obtained from the patient to publish the case report, and information was de-identified to protect anonymity.
ORCID: Renato Oliveira: https://orcid.org/0000-0003-1181-1418; Tomás Teodoro: https://orcid.org/0000-0002-4603-3946
References (4)

- Xu XQ, Cheng QG, Zu QQ, et al. Comparative study of the relative signal intensity on DWI, FLAIR, and T2 images in identifying the onset time of stroke in an embolic canine model. Neurol Sci. 2014;35(7):1059–1065. PubMed CrossRef
- Merten CL, Knitelius HO, Assheuer J, et al. MRI of acute cerebral infarcts, increased contrast enhancement with continuous infusion of gadolinium. Neuroradiology. 1999;41(4):242–248. PubMed CrossRef
- Allen LM, Hasso AN, Handwerker J, et al. Sequence-specific MR imaging findings that are useful in dating ischemic stroke. Radiographics. 2012;32(5):1285–1297, discussion 1297–1299. PubMed CrossRef
- Karonen JO, Partanen PL, Vanninen RL, et al. Evolution of MR contrast enhancement patterns during the first week after acute ischemic stroke. AJNR Am J Neuroradiol. 2001;22(1):103–111. PubMed
Enjoy this premium PDF as part of your membership benefits!