Abstract
Objective: Current therapies for multiple sclerosis (MS) often have limited efficacy and side effects, necessitating alternative approaches. Noninvasive brain stimulation (NIBS), such as transcranial direct current stimulation and transcranial magnetic stimulation (TMS), offers potential solutions. Among NIBS techniques, theta burst stimulation (TBS) is notable for its ability to modulate cortical activity. The objective of this systematic review is to assess the impact of TBS on MS symptoms.
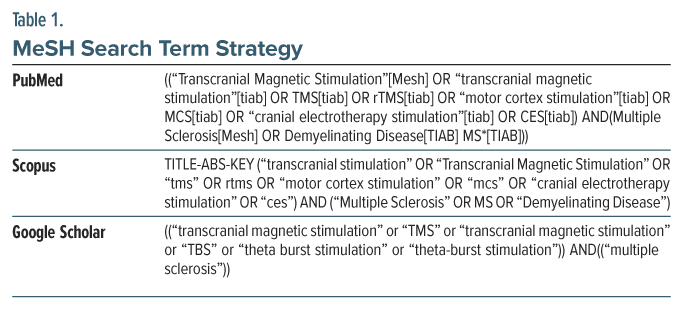
Data Sources: The study conducted rigorous systematic searches in PubMed, Google Scholar, and Scopus databases up to June 2023, using specific Medical Subject Headings terms related to NIBS and MS, such as TMS and TBS, in conjunction with terms like MS or demyelinating disease. Additionally, the bibliographic references of included studies, book chapters, and original articles were manually reviewed.
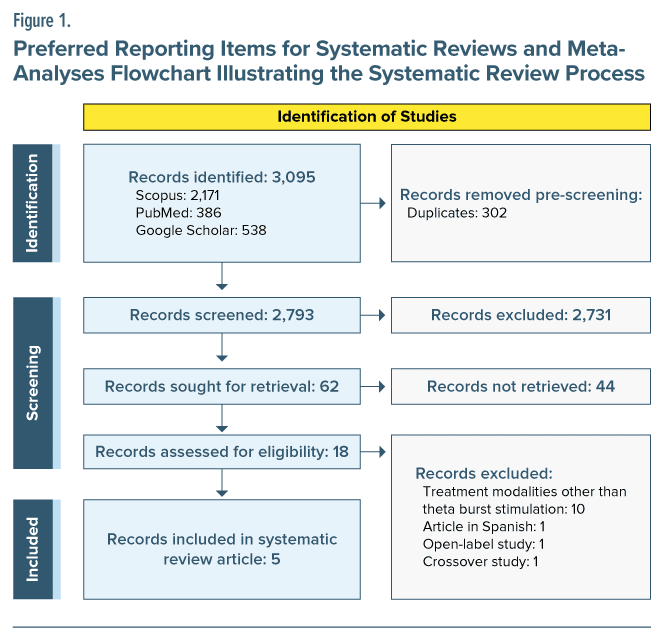
Study Selection: The study selection process involved a 2-tiered screening mechanism, beginning with an evaluation of titles and abstracts, followed by a full-text review of selected articles. Inclusion criteria incorporated randomized controlled trials (RCTs) focusing on TBS with MS patients. Exclusion criteria included non-qualitative, non-MS, and non-TBS studies. Risk of bias assessment was conducted using the 2008 Cochrane Risk of Bias 2 Scale for RCTs.
Data Extraction: Data extraction was conducted by thoroughly reviewing each research article and systematically recording the relevant information using a standardized data extraction form, ensuring consistency and accuracy throughout the process.
Results: In a systematic review encompassing 5 randomized controlled trials involving 117 individuals with relapsing-remitting or secondary progressive MS across Italy, France, and Russia, various forms of TBS were applied. These interventions ranged from intermittent TBS (iTBS) to continuous intermittent TBS (c-iTBS) that demonstrated favorable outcomes. Notably, TBS interventions led to significant reductions in spasticity, fatigue, and pain, with c-iTBS combined with vestibular rehabilitation showing additional improvements in vestibular-ocular reflexes, gait, and balance. While specific protocols varied among the studies, collectively, the results suggest promise for TBS approaches in alleviating MS-related symptoms.
Conclusions: The findings of this review suggest that TBS may hold promise in addressing specific MS symptoms, notably fatigue and spasticity. Future research should include a more diverse participant pool to explore TBS effects across different MS subtypes and aim for larger sample sizes to enhance statistical power and result reliability.
Prim Care Companion CNS Disord 2024;26(2):23r03645
Author affiliations are listed at the end of this article.
Multiple sclerosis (MS) is a prevalent autoimmune inflammatory disorder affecting the central nervous system, characterized by the involvement of multiple white matter tracts and gray matter atrophy.1 Its profound impact on young adults, serving as the leading nontraumatic cause of neurological disability, underscores its clinical significance.2 The diverse array of symptoms arising from MS includes motor and sensory deficits, pain, vision issues, cognitive impairment, fatigue, psychiatric manifestations, and spasticity. These symptoms are contingent upon the extent and localization of neural damage.3 In the quest for efficacious treatments with minimal adverse effects, the challenge is substantial.1,2
While current disease-modifying therapies often yield unsatisfactory results with notable side effects in many patients, the need for alternative treatments is apparent. Consequently, a multidisciplinary approach and nonpharmacologic interventions have been advocated to manage MS symptoms.4,5 Within this context, noninvasive brain stimulation (NIBS) has emerged as a potential avenue for counteracting maladaptive plasticity.6 The therapeutic potential of NIBS extends across various neurological and psychiatric conditions.7 Prominent among the NIBS techniques are transcranial direct current stimulation (tDCS), transcranial magnetic stimulation (TMS), transcranial random noise stimulation, transcranial alternating current stimulation, and cranial electrotherapy stimulation.8,9 While tDCS applies weak electrical currents between scalp electrodes to modulate neuronal transmembrane potential in a polarity-dependent manner, TMS employs a magnetic field to induce electrical changes in the brain. These techniques exhibit distinct modes of action to influence neural activity.8–11
Of note, among these techniques, theta burst stimulation (TBS) has emerged as a compelling method for cortical modulation. TBS, a form of high-frequency repetitive TMS (rTMS), introduces an alternative to conventional rTMS protocols, allowing more rapid delivery of pulses with comparable outcomes. TBS comprises 2 primary types: intermittent TBS (iTBS), characterized by an interval pattern that facilitates cortical activity, and continuous intermittent TBS (c-iTBS), featuring a continuous pattern that suppresses cortical excitability.12,13 Both tDCS and TMS exhibit sensitivity to various parameters including stimulus region, intensity, duration, and neural network state.14,15 This state-dependent nature mandates a well-designed therapeutic approach to drive neuroplasticity.16
Several studies have delved into the various NIBS techniques on MS including 3 systematic reviews.17–19 Despite that, there have been no articles specifically investigating TBS in MS patients. The existing literature presents conflicting outcomes on distinct MS symptoms such as pain, fatigue, cognitive impairment, motor ability, and spasticity.3 Discrepancies in methodologies across studies and variations in sample sizes contribute to this inconsistency. The resulting lack of consensus impedes the establishment of TBS as a definitive therapeutic strategy for MS symptoms. Addressing this knowledge gap is imperative for advancing TBS use as a viable approach in the management of MS symptoms.
METHODS
This systematic review meticulously followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines; however, the limited availability of clinical studies rendered the execution of a meta-analysis impractical. The procedures of this review were carried out in strict accordance with the 2015 PRISMA recommendations.20 This is depicted in Figure 1.
Search Methodology
In a rigorous and comprehensive manner, we conducted systematic searches across multiple databases, including PubMed, Scopus, and Google Scholar. This search encompassed the period until June 2023, and it was guided by a meticulously crafted search strategy featuring specific Medical Subject Headings (MeSH) terms such as TMS and TBS, in conjunction with terms like MS or demyelinating disease. For detailed insight into the complete research strategy, refer to Table 1.
In addition to electronic database searches, we extended our exploration by manually scrutinizing the bibliographic references of the studies included, along with perusing relevant book chapters and original articles, as a supplementary effort following the primary search. Prior to progressing to the selection phase, a standardized approach was established through consensus between 2 reviewers (D.F.L and M.P.). Moving forward, the titles and abstracts of potential studies were meticulously evaluated by these reviewers independently. In the event of any disparities, resolutions were achieved through comprehensive discussions or consultation with a third author (A.G.). Subsequently, primary reviewers independently evaluated the full texts of the studies.
Study Selection
The process of study selection followed a comprehensive 2-tiered screening approach. Initially, a meticulous examination was conducted on the titles and abstracts of relevant articles. Any inconsistencies were rigorously reviewed and resolved through discussion. In cases where disagreements persisted, the publications in question advanced to the full-text review phase. Subsequently, the full texts of articles that successfully passed the initial screening were subjected to in-depth analysis by 2 independent reviewers. Any remaining disparities were thoroughly discussed, and if necessary, a third reviewer was engaged to mediate and resolve any lingering disagreements.
Inclusion Criteria
Our article selection criteria were designed to ensure the quality and relevance of our chosen studies. We prioritized randomized controlled trials (RCTs) for their rigorous methodology. Studies had to incorporate TBS as an essential part of their research. Additionally, participants were required to have a diagnosis of MS, regardless of the subtype. This approach allowed us to include a broad spectrum of MS cases. These strict criteria aimed to guarantee methodological soundness and direct relevance to MS in the selected research, enhancing the quality and applicability of our analysis. A restriction based on language led to the inclusion of solely English studies.
Exclusion Criteria
Our exclusion criteria were employed to refine our selection process further. We excluded studies that deviated from qualitative methodologies, as our primary focus was on rigorous, evidence-based research. Additionally, we eliminated studies that did not involve participants diagnosed with MS, as our analysis was geared towards understanding MS-related factors. Studies that did not have a clear emphasis on TBS were also excluded to maintain the specificity of our review. Finally, non-RCTs were not included to ensure the highest methodological quality in the selected articles. These exclusion criteria were essential to maintain the coherence and relevance of our study selection.
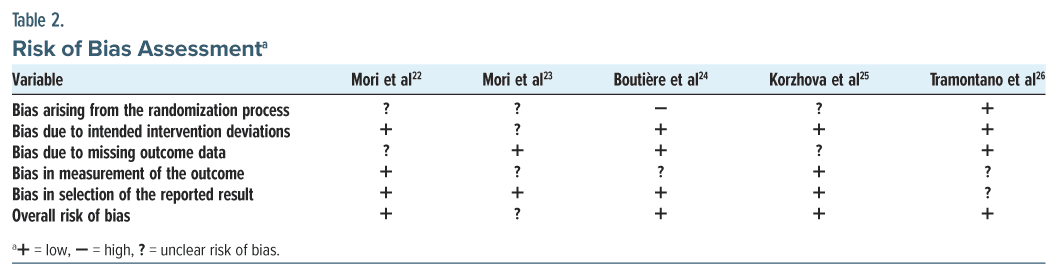
Assessment of Risk of Bias
Following the removal of duplicates, items were assessed for relevance based on title and abstract. Full text appraisal and risk of bias were conducted by 2 reviewers (D.F.L. and M.P.) on studies deemed potentially eligible using the updated 2008 Cochrane Risk of Bias 2 Scale for Randomized Controlled Trials.21 We used specific criteria (low, some concerns, and high) to classify the risk of bias shown in Table 2. In the event of debate, a third reviewer (A.G.) made the final determination; however, this was not necessary in the case of this systematic review. Eligible studies were then subjected to data extraction.
RESULTS
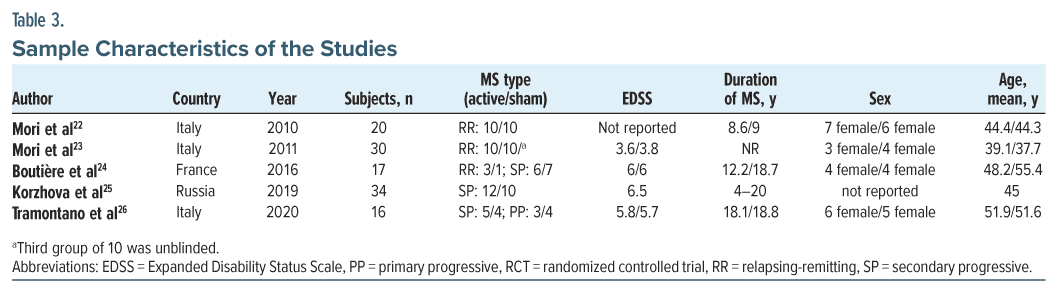
A total of 5 RCTs met the established inclusion criteria and became part of the comprehensive systematic review. Among these, 3 studies occurred in Italy with the rest in France and Russia. The cumulative studies encompassed 117 individuals, with individual study samples ranging from 16 to 34 participants. The focal demographic across all the included publications was a specific population aged 33–59 years, all of whom had been diagnosed with relapsing-remitting MS (RR-MS) or secondary progressive (SP) MS. A condensed overview of the incorporated studies is shown in Table 3.
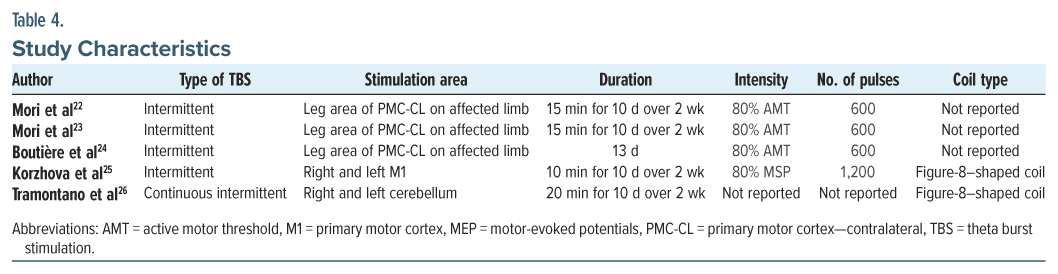
In both 2010 and 2011, Mori et al22,23 employed iTBS targeting the leg area of the primary motor cortex contralateral to the affected limb. This stimulation was administered for 15 minutes daily over 10 days spanning 2 weeks, with an intensity set at 80% of the individual’s active motor threshold. Both studies used a total of 600 pulses that included concomitant exercise therapy (ET). Similarly, Boutière et al24 utilized iTBS, focusing on the leg area of the primary motor cortex contralateral to the affected limb. However, their stimulation protocol spanned 13 days, maintaining the same intensity and pulse count. Korzhova et al25 adopted iTBS targeting the right and left primary motor cortex for 10 minutes daily over 10 days distributed across 2 weeks. Their stimulation intensity was set at 80% of the motor threshold for motor-evoked potentials, employing 1,200 pulses and concomitant physical therapy. In contrast, Tramontano et al26 implemented c-iTBS, targeting the right and left cerebellum for 20 minutes daily over 10 days in 2 weeks, without specifying intensity or pulse count. Their concomitant therapy consisted of vestibular rehabilitation (VR). This diversity in stimulation protocols reflects the heterogeneity among the included studies, offering valuable insights into the variations in approaches to TBS interventions for MS. The characteristics of all the studies are summarized in Table 4.
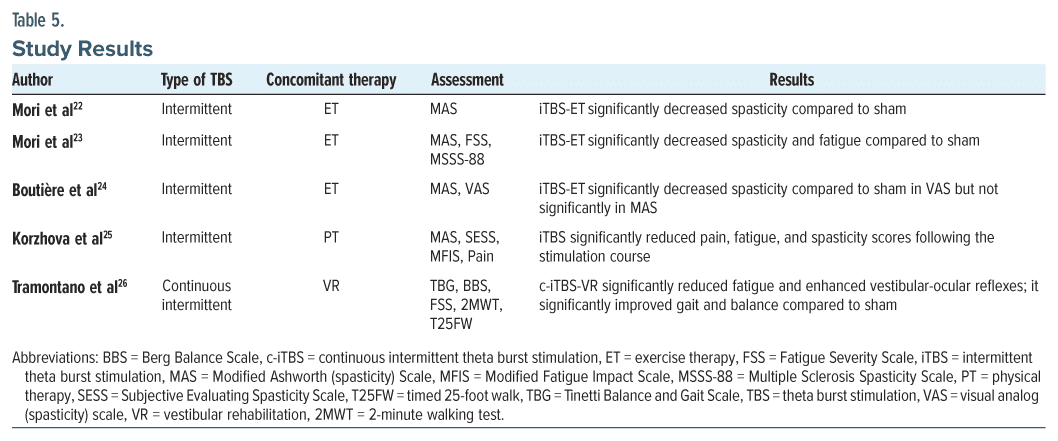
Mori et al22 utilized iTBS-ET and found a significant reduction in spasticity scores, as assessed by the Modified Ashworth Scale (MAS), compared to the sham group. In 2011, the same authors23 reported positive outcomes with iTBS-ET, demonstrating significant decreases in both spasticity (MAS) and fatigue (Fatigue Severity Scale) scores compared to sham. Similarly, Boutière et al24 observed that the iTBS group exhibited significant improvements or reductions in spasticity, assessed by the visual analog scale (VAS), in comparison with the sham iTBS group. Korzhova et al25 showed that iTBS significantly reduced spasticity, fatigue, and pain scores compared to sham. Lastly, Tramontano et al26 implemented c-iTBS-VR and noted significant enhancements in vestibular-ocular reflexes, gait, and balance compared to those who received sham iTBS-VR treatment. Table 5 summarizes the results of all the included studies, providing insights into the impact of different types of TBS on various assessments related to MS symptoms.
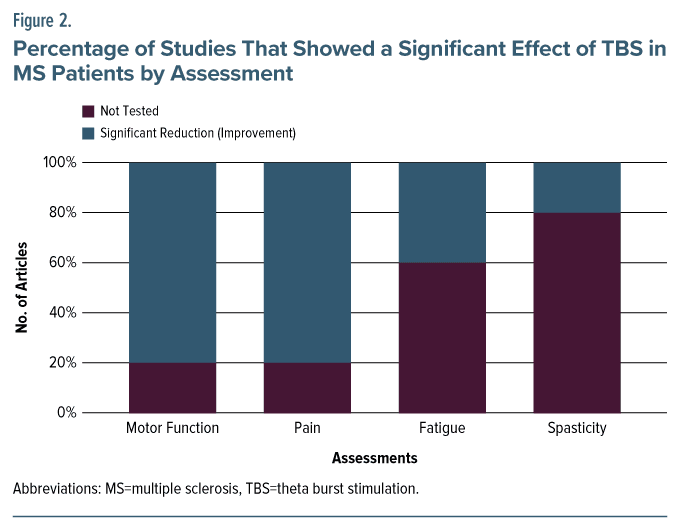
Overall, in terms of TBS effects on fatigue, 80 patients were evaluated through 3 studies.23,25,26 There was a significant decrease in fatigue in favor of TBS intervention compared with sham. There was only 1 study that used c-iTBS and 2 studies that used iTBS.23,25,26 For motor performance, there was only 1 study with 16 patients26 that used iTBS and evaluated the motor performance by T25FW (timed 25-foot walk) and 9HPT (9-hole peg test). There was no strong evidence showing iTBS effectiveness on motor performance. On spasticity, 4 studies of 101 patients investigated the TBS effects, and all 4 showed a significant effect of TBS on spasticity improvement as summarized in Figure 2.22–25
DISCUSSION
In summary, the study’s findings indicate that TBS holds promise for the reduction of fatigue and spasticity in MS. Additionally, a multidisciplinary approach, combining TBS with other therapeutic modalities, may offer comprehensive benefits for MS patients, emphasizing the importance of tailored treatment strategies. However, these positive outcomes are primarily observed in the context of RR-MS, and further research is needed to understand TBS’s effects on other MS subtypes.
Clinical Care of Patients
The findings of this systematic review indicate a significant reduction in fatigue among individuals with MS following TBS interventions. Notably, the evidence supporting the positive impact of TBS on fatigue is primarily observed in patients with RR-MS. The included studies demonstrated consistent and favorable outcomes, emphasizing the potential clinical implications of TBS in managing fatigue in this specific subtype of MS. The effective TBS protocols for addressing fatigue varied among the studies. Mori et al23 utilized iTBS targeting the leg area of the primary motor cortex contralateral to the affected limb. The stimulation was administered for 15 minutes daily over 10 days, with an intensity set at 80% of the individual’s active motor threshold. This protocol, combined with concomitant ET, resulted in significant decreases in both spasticity and fatigue scores compared to sham interventions. The positive outcomes highlight the potential of iTBS as a promising approach for managing fatigue in RR-MS patients.
The findings of this systematic review also revealed a significant reduction in spasticity among individuals with MS, particularly in the context of RR-MS. The evidence suggests that RR-MS patients experienced notable improvements in muscle spasticity following TBS interventions. The effective TBS protocols for addressing spasticity were heterogeneous across the studies. Mori et al,22,23 Boutière et al,24 and Korzhova et al25 all employed iTBS targeting various areas such as the leg area of the primary motor cortex contralateral to the affected limb or the right and left primary motor cortex. The stimulation durations varied from 10 to 15 minutes daily over 10 to 13 days. The intensity was set at 80% of the motor threshold, with pulse counts ranging from 600 to 1,200. These iTBS protocols consistently led to significant reductions in spasticity scores, emphasizing the potential efficacy of iTBS in addressing spasticity in RR-MS patients. It is noteworthy that c-iTBS applied to the cerebellum in the study by Tramontano et al26 did not show significant improvements in spasticity but demonstrated enhancements in motor functioning, suggesting potential protocol-specific effects.
Limitations
This review possesses several strengths, such as the consistent and positive outcomes observed in managing fatigue and spasticity using TBS interventions among MS patients. However, it is not without its limitations. The review primarily focused on the RR-MS subtype, limiting our understanding of TBS’s effects on other MS subtypes. The influence of disease-modifying therapies on TBS effects remains challenging to estimate, highlighting the need for future studies to control for these therapies. Additionally, inclusion of only English language studies may limit the generalizability of the findings to non–English-speaking populations. The small sample sizes in most studies may also restrict the generalizability of the results. To enhance the statistical power and reliability of future investigations, researchers should aim for larger sample sizes.
CONCLUSION
While TBS has gained attention as a promising therapeutic approach for individuals with MS, this review underscores the need for further research to harness its full clinical potential. The findings of this review suggest that TBS may hold promise in addressing specific MS symptoms, notably fatigue and spasticity. The observed reduction in fatigue levels and improvements in spasticity following TBS interventions are encouraging developments. However, it is crucial to recognize that the existing evidence is primarily derived from studies focusing on RR-MS and involves relatively small sample sizes. This limitation emphasizes the necessity for broader investigations encompassing different MS subtypes and larger, more diverse patient populations.
Article Information
Published Online: April 18, 2024. https://doi.org/10.4088/PCC.23r03645
© 2024 Physicians Postgraduate Press, Inc.
Submitted: September 16, 2023; accepted December 4, 2023.
To Cite: Lo DF, Palhang M, Gawash A, et al. Unlocking therapeutic potential: impact of theta burst stimulation on multiple sclerosis. Prim Care Companion CNS Disord. 2024;26(2):23r03645.
Author Affiliations: New Jersey Institute for Successful Aging, Rowan-Virtua School of Osteopathic Medicine, Stratford, New Jersey (Lo, Palhang, Gawash, Goodwin, Patel, White); American Preventive Screening & Education Association, Stratford, New Jersey (Lo, Gawash, Zia); Department of Biology, Rutgers, The State University of New Jersey, New Brunswick, New Jersey (Lo, Zia); Lumina Institute, Cream Ridge, New Jersey (Lo, Zia, Goodwin); Futures Forward Research Institute, Toms River, New Jersey (Lo, Zia, Goodwin).
Corresponding Author: David F. Lo, MBS, Department of Medicine, Rowan School of Osteopathic Medicine, 1 Medical Center Dr, Stratford, NJ 08084 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
ORCID: David F. Lo: https://orcid.org/0000-0003-2408-9735; Ahmed Gawash: https://orcid.org/0000-0002-6044-6958; Hasan Zia: https://orcid.org/0000-0001-6304-5888; Brandon J. Goodwin: https://orcid.org/0000-0002-3965-4664
Clinical Points
- Theta burst stimulation (TBS) interventions hold promise in reducing fatigue, a common and debilitating symptom in multiple sclerosis (MS).
- Specific TBS techniques have shown effectiveness in reducing spasticity, especially in cases of relapsing remitting MS.
- A multidisciplinary approach, combining TBS with other therapies, may offer comprehensive benefits in managing various MS symptoms.
References (26)

- Reich DS, Lucchinetti CF, Calabresi PA. Multiple sclerosis. N Engl J Med. 2018;378(2):169–180. PubMed CrossRef
- Dobson R, Giovannoni G. Multiple sclerosis – a review. Eur J Neurol. 2019;26(1):27–40. PubMed CrossRef
- Zhou X, Li K, Chen S, et al. Clinical application of transcranial magnetic stimulation in multiple sclerosis. Front Immunol. 2022;13:902658. PubMed CrossRef
- Talanki Manjunatha R, Habib S, Sangaraju SL, et al. Multiple sclerosis: therapeutic strategies on the horizon. Cureus. 2022;14(5):e24895. PubMed CrossRef
- Gajofatto A, Benedetti MD. Treatment strategies for multiple sclerosis: when to start, when to change, when to stop? World J Clin Cases. 2015;3(7):545–555. PubMed CrossRef
- Naro A, Milardi D, Russo M, et al. Non-invasive brain stimulation, a tool to revert maladaptive plasticity in neuropathic pain. Front Hum Neurosci. 2016;10:376. PubMed CrossRef
- Ghosh S. Improvement of gait and balance by non-invasive brain stimulation: its use in rehabilitation. Expert Rev Neurother. 2019;19(2):133–144. PubMed CrossRef
- O’Connell NE, Marston L, Spencer S, et al. Non-invasive brain stimulation techniques for chronic pain. Cochrane Database Syst Rev. 2018;3(3):CD008208. PubMed
- Tavakoli AV, Yun K. Transcranial alternating current stimulation (tACS) mechanisms and protocols. Front Cell Neurosci. 2017;11:214. PubMed CrossRef
- Thair H, Holloway AL, Newport R, et al. Transcranial direct current stimulation (tDCS): a beginner’s guide for design and implementation. Front Neurosci. 2017;11:641. PubMed CrossRef
- Chung CLH, Mak MKY, Hallett M. Transcranial magnetic stimulation promotes gait training in Parkinson disease. Ann Neurol. 2020;88(5):933–945. PubMed CrossRef
- Stoby KS, Rafique SA, Oeltzschner G, et al. Continuous and intermittent theta burst stimulation to the visual cortex do not alter GABA and glutamate concentrations measured by magnetic resonance spectroscopy. Brain Behav. 2022;12(2):e2478. PubMed CrossRef
- Huang YZ, Edwards MJ, Rounis E, et al. Theta burst stimulation of the human motor cortex. Neuron. 2005;45(2):201–206. PubMed CrossRef
- Siebner HR, Funke K, Aberra AS, et al. Transcranial magnetic stimulation of the brain: what is stimulated? – a consensus and critical position paper. Clin Neurophysiol. 2022;140:59–97. PubMed CrossRef
- Reithler J, Peters JC, Sack AT. Multimodal transcranial magnetic stimulation: using concurrent neuroimaging to reveal the neural network dynamics of noninvasive brain stimulation. Prog Neurobiol. 2011;94(2):149–165. PubMed CrossRef
- Kricheldorff J, Göke K, Kiebs M, et al. Evidence of neuroplastic changes after transcranial magnetic, electric, and deep brain stimulation. Brain Sci. 2022;12(7):929. PubMed CrossRef
- Li S, Zhang Q, Zheng S, et al. Efficacy of non-invasive brain stimulation on cognitive and motor functions in multiple sclerosis: a systematic review and meta-analysis. Front Neurol. 2023;14:1091252. PubMed CrossRef
- Alashram AR, Janada Q, Ghrear T. Noninvasive brain stimulation for spasticity rehabilitation in multiple sclerosis: a systematic review of randomized controlled trials. PM R. 2024;16(3):268–277. PubMed CrossRef
- Su D, Wang A, Zhu M, et al. Repetitive transcranial magnetic stimulation for treatment of limb spasticity following multiple sclerosis: a systematic review and meta-analysis. Braz J Med Biol Res. 2023;56:e12708. PubMed CrossRef
- Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. PubMed CrossRef
- Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2008:187–241. CrossRef
- Mori F, Codecà C, Kusayanagi H, et al. Effects of intermittent theta burst stimulation on spasticity in patients with multiple sclerosis. Eur J Neurol. 2010;17(2):295–300. PubMed CrossRef
- Mori F, Ljoka C, Magni E, et al. Transcranial magnetic stimulation primes the effects of exercise therapy in multiple sclerosis. J Neurol. 2011;258(7):1281–1287. PubMed CrossRef
- Boutière C, Rey C, Zaaraoui W, et al. Improvement of spasticity following intermittent theta burst stimulation in multiple sclerosis is associated with modulation of resting-state functional connectivity of the primary motor cortices. Mult Scler. 2017;23(6):855–863. PubMed
- Korzhova J, Bakulin I, Sinitsyn D, et al. High-frequency repetitive transcranial magnetic stimulation and intermittent theta-burst stimulation for spasticity management in secondary progressive multiple sclerosis. Eur J Neurol. 2019;26(4):680-e44. PubMed CrossRef
- Tramontano M, Grasso MG, Soldi S, et al. Cerebellar intermittent theta-burst stimulation combined with vestibular rehabilitation improves gait and balance in patients with multiple sclerosis: a preliminary double-blind randomized controlled trial. Cerebellum. 2020;19(6):897–901. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!