Abstract
Objective: This study examined the relationships between body fat mass percentage and mental health (depression and anxiety symptoms) during pregnancy, while assessing the moderating effects of physical activity and diet quality.
Methods: A prospective cohort of 219 pregnant women was recruited for a longitudinal study of maternal health during pregnancy and offspring outcomes. Pregnant participants were assessed at ∼12 and ∼36 weeks of pregnancy. Body composition was measured using air displacement plethysmography, physical activity was measured with ActiGraph wearables, and diet was measured using the National Institute of Health Diet History Questionnaire-III. Depression and anxiety symptoms were also evaluated using the Beck Depression Inventory-II and State-Trait Anxiety Inventory, respectively, at each study visits. Multivariable mixed linear models adjusted for demographic and socioeconomic factors were used to analyze relationships among these parameters. The study period is from October 2019 to August 2024.
Results: Higher body fat mass percentage was significantly associated with increased depression (β= 0.246, P=.014) and anxiety scores (β= 0.241, P=.002). Physical activity moderated the effect of body fat on depression (interaction β=–0.001, P=.017), while diet quality moderated the effect of body fat on anxiety (interaction β=–0.002, P=.047).
Conclusion: Higher body fat mass during pregnancy is associated with more symptoms of depression and anxiety. However, increased physical activity and adherence to high-quality diets can attenuate these effects, indicating that lifestyle interventions during pregnancy may improve mental health of pregnant women, particularly for those with obesity.
J Clin Psychiatry 2025;86(4):25m15822
Author affiliations are listed at the end of this article.
Obesity during pregnancy is a growing public health concern worldwide. The prevalence of pre-pregnancy obesity has risen sharply over the last few decades, which has significant implications for maternal and fetal health outcomes.1 The latest report from the National Health and Nutrition Examination Survey shows that approximately one-third of women of childbearing age in the United States are obese (body mass index [BMI]≥30), and more than half of pregnant women are overweight or obese. Obesity during pregnancy has been linked to various health complications, including gestational diabetes, hypertensive disorders such as preeclampsia, increased rates of emergency cesarean delivery, and a higher likelihood of preterm birth.2,3 Maternal obesity during pregnancy is also a significant risk factor for childhood obesity and is associated with an increased risk of diabetes, metabolic syndrome, and adverse cardio metabolic conditions in children.4–8 These findings suggest that obesity during pregnancy may have negative impacts on both pregnancy and offspring outcomes.
Meanwhile, mental health issues such as depression and anxiety are also highly prevalent among pregnant women, affecting up to 20% of pregnancies globally.9 Using data from the National Health Interview Survey (2010–2019) of pregnant women aged 18–44, prenatal depression prevalence was 40.6% in White, 28.5% in Black, and 27.2% in other racial groups. It was 58.1% for those without regular prenatal care and 46.9% for those without paid sick leave.10 Similarly, anxiety disorders during pregnancy have been reported in approximately 15% to 20% of pregnant individuals.11 Existing literature has consistently reported associations between obesity and increased mental health issues during pregnancy.
Higher pre-pregnancy BMI has been linked to increased risks of prenatal depression and anxiety, which may persist into the postpartum period, leading to long-lasting mental health issues. Early interventions, such as psychological support and behavioral modifications, are crucial to alleviate symptoms during pregnancy and prevent postpartum mental health sequelae.12 The associations between obesity and increased prevalence of anxiety and depression during and after pregnancy warrant targeted mental health support for women with obesity.13,14
It is important to consider the potential bidirectional relationship between body weight and mental health. Existing evidence suggests that higher body mass index or body fat percentage is significantly associated with an increased risk of depression and anxiety. Epidemiological and longitudinal studies have shown that individuals with overweight or obesity are more likely to experience depressive symptoms, while depression itself may contribute to subsequent weight gain, thus creating a reinforcing cycle.15,16 Moreover, specific components of body composition—such as the ratio of fat mass to lean mass—may influence neurobiological processes via metabolic and endocrine mechanisms, including chronic inflammation, insulin resistance, and hormonal dysregulation, all of which may affect emotional regulation and mental well-being.17
Most existing studies have utilized BMI as the primary measure of obesity to examine the relationships between obesity and mental health during pregnancy. However, this approach may not be ideal, as BMI does not sufficiently account for the unique physiological changes occurring during pregnancy. For instance, even women with a normal pre-pregnancy weight typically experience substantial gestational weight gain, potentially differing in fluid retention, fat mass, and lean mass changes compared to women with obesity. Such variations may confound the true relationships between obesity and mental health—particularly if BMI is measured only at later stages of pregnancy.18 In contrast, body composition parameters (eg, body fat mass percentage) may more accurately capture changes in adiposity during pregnancy. By differentiating between fat mass, lean tissue, and fluid compartments, these measures offer a more nuanced understanding of how obesity evolves throughout pregnancy and how it might impact mental health. Therefore, assessing body composition rather than relying solely on BMI could be better suited to elucidate the potential effects of obesity on mental health in pregnant populations.
Physical activity and diet interventions are both common, effective, and noninvasive intervention strategies for obesity. Physical activity during pregnancy is an important modifiable factor that can influence both physical and mental health of pregnant women. Regular exercise has been shown to reduce symptoms of anxiety and depression in this population, potentially through mechanisms such as enhanced endorphin release, improved circulation, and stress reduction.19 In addition, adherence to dietary guidelines during pregnancy, characterized by nutrient-rich and balanced eating patterns, has been associated with improved mental health in pregnant women. For instance, diets high in omega-3 fatty acids, antioxidants, and micronutrients have been linked to lower risks of depressive symptoms.20 Studies have also shown that the Mediterranean diet helps reduce stress, improve well-being, and enhance sleep quality of pregnant women.21 While previous studies have explored the relationships between physical activity, body composition, and mental health in some populations,22–24 there is a paucity in literature regarding how physical activity and diet interact with body composition to influence mental health during pregnancy.
In this study, we hypothesized that body composition during pregnancy significantly impacts mental health in pregnant women, and these effects are moderated by physical activity and diet during pregnancy. Specifically, we hypothesized that higher body fat mass percentage in pregnant women is associated with poorer mental health outcomes as reflected by higher depression and anxiety symptom scores. Furthermore, these relationships are attenuated by greater physical activity level measured by wearable devices and better adherence to dietary recommendations such as those outlined in the Dietary Guidelines for Americans. To test this hypothesis, we utilized pregnancy data from the ongoing Maternal Obesity and Offspring Neurodevelopment (MOON) study, which includes comprehensive measurements of body composition, physical activity, diet, and mental health throughout pregnancy in a cohort of healthy pregnant women. We aim to identify the relationships between body fat percentage and depression/anxiety symptoms scores, as well as the moderating effects by physical activity level and diet quality.
METHODS
Study Participants
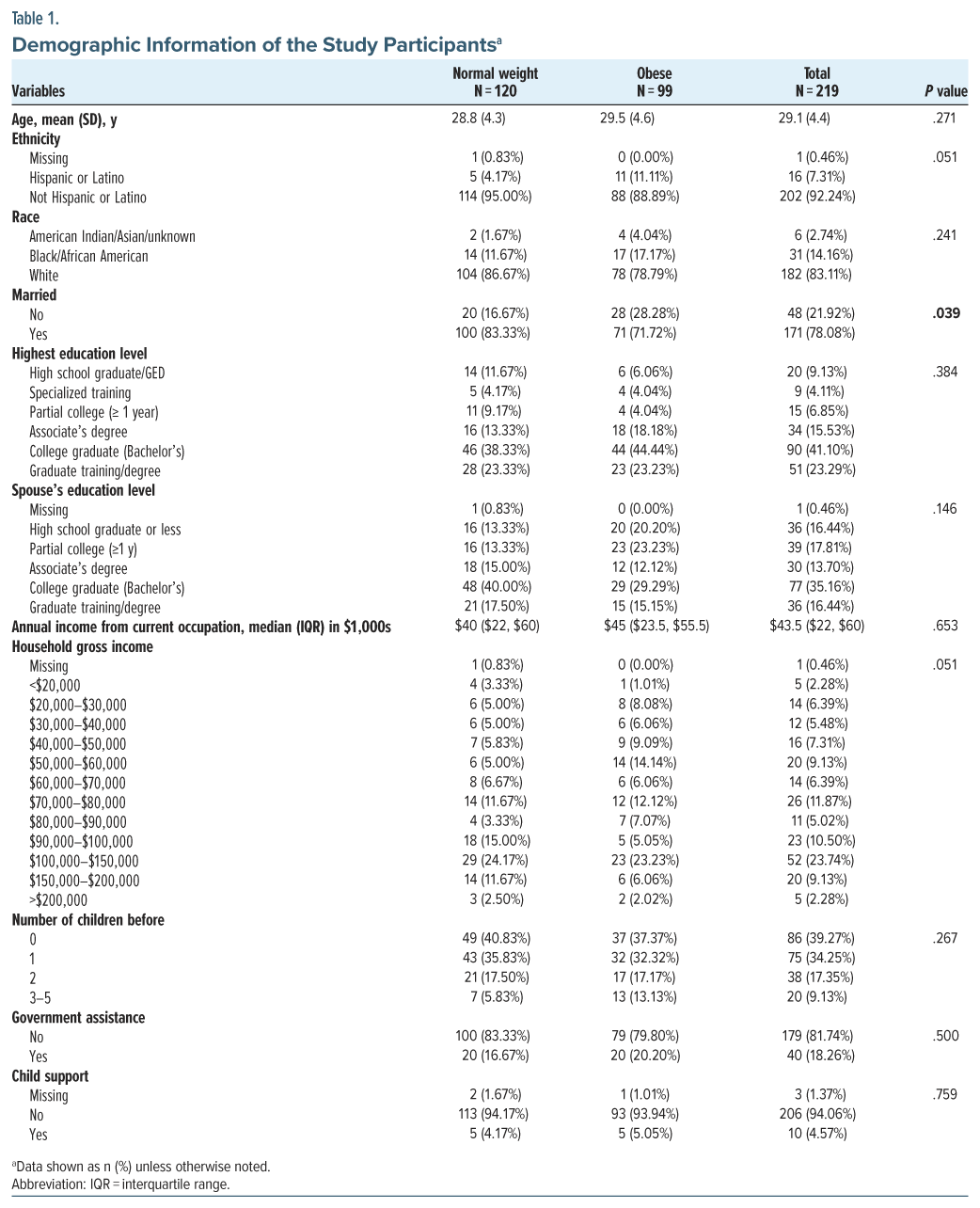
A total of 219 pregnant women were enrolled in the MOON study during the first trimester of pregnancy and completed assessments of body composition, physical activity, diet, and mental health throughout pregnancy and were included for this study. Among them, 120 participants were normal weight (BMI 18.5–25), and 99 participants were obese (BMI 30–50) at the time of enrollment. Participants were recruited using established methods at the Arkansas Children’s Nutrition Center. The inclusion criteria were singleton pregnancy, 11–13 weeks of gestation, ≥18 years of age, and BMI ≤25 or ≥30. The exclusion criteria were BMI <18.5 or >50, pre-existing medical conditions or medications known or suspected to influence fetal growth (eg, hypertension, diabetes), medical complications developed during pregnancy known or suspected to influence fetal growth (eg, gestational diabetes, preeclampsia), family history of psychological or neurogenetic disorders, use of substances (eg, recreational drugs, nicotine, alcohol) during pregnancy, and preterm delivery at <37 weeks of gestation. The demographic information of the study participants is listed in Table 1. Each participant had an onsite study visit at ∼12 weeks and again at ∼36 weeks of pregnancy for the measurements of body composition, physical activity, and mental health. In addition, each participant was asked to complete a dietary assessment online at ∼12, ∼24, and ∼36 weeks of pregnancy. The mean ± SD of their gestational age at the three visits were 12.40 ± 0.87, 24.29 ± 1.27, and 36.19 ± 0.62 weeks.
Measurement of Body Composition
Body composition of the pregnant women was assessed at approximately 12 and 36 weeks of gestation using air displacement plethysmography (ADP) via a BodPod system (Cosmed, Concord, CA). ADP is a noninvasive, reliable technique based on whole-body densitometry. The method estimates body volume by measuring air displacement while the subject is seated in a closed chamber and subsequently calculates body density from body mass and volume. Fat mass and fat-free mass are then derived using a 2-compartment model. This technique provides accurate assessments of obesity-related parameters such as body fat mass percentage. Previous studies have demonstrated that ADP is a valid method for assessing body composition in pregnant women, even in the presence of gestational physiological changes such as increased plasma volume or amniotic fluid fluctuations.25,26 To complement body composition assessment, standardized anthropometric measurements were also conducted, including weight (using a digital standing scale), height (using a wall-mounted stadiometer), and waist and hip circumferences (using a flexible tape measure).
Measurement of Physical Activity
Physical activity of the pregnant women was measured at ∼12 weeks and ∼36 weeks of pregnancy using an ActiGraph watch (Pensacola, FL), which the participants wore on their wrist for 1 week following each study visit. The ActiGraph watch recorded daily movement activity and provided an objective estimate of physical activity levels of the subjects. After the watches were returned, the data were downloaded; recorded parameters included daily steps, activity counts, sedentary time, time spent in light and moderate activity, and maximum step count per minute.
Measurement of Diet
Dietary intakes of the pregnant women were measured at ∼12 weeks, ∼24 weeks, and ∼36 weeks of pregnancy using the National Institute of Health (NIH) web-based Diet History Questionnaire, Third Edition (DHQ-III). The DHQ-III is a freely available food frequency questionnaire for use with adults 19 years or older. The version assessing food intake “in the past month with portion size” was used. It consists of 135 food and beverage line items and 26 dietary supplement questions. After completion, a healthy eating index (HEI) score was calculated based on subject responses. The HEI score is a measure of diet quality, specifically, how well the set of foods the participants consumed aligns with key recommendations and dietary patterns published in the Dietary Guidelines for Americans. A higher HEI score represents better alignment with the dietary guidelines. In addition to the composite total HEI score, component scores were calculated for vegetables, greens and beans, fruits, grains, dairy, plant protein, total protein, fatty acids, saturated fats, seafood, sodium, and added sugar.
Measurement of Mental Health
Mental health of the pregnant women, specifically, their depression and anxiety symptoms, was assessed at ∼12 weeks and ∼36 weeks of pregnancy by trained psychological examiners. Using the Beck Depression Inventory-II (BDI-II) and the State-Trait Anxiety Inventory (STAI), participants’ symptoms were evaluated in a standardized manner. The BDI-II is a validated and commonly used tool to measure depression symptoms and was used in this study.27 It is a 21-item self-report questionnaire, and each question is scored 0–3. The total BDI score ranges from 0 to 63, and a higher BDI score indicates greater depression symptoms. The STAI is a validated and commonly used tool to measure anxiety symptoms and was used in the study.28 It is a 20-item self-report assessment device which includes separate measures of state and trait anxiety. Each item is scored 1–4, so the total STAI score ranges from 20 to 80. A higher STAI score indicates greater anxiety symptoms.
Statistical Analysis
We first examined the extent and patterns of missing data across primary outcome variables (BDI-II, STAI-S, STAI-T) and relevant covariates (body fat %, steps max count, age, and total HEI). Descriptive statistics were first computed to determine the proportion of missing values. To investigate the mechanism of missing data, we performed logistic regression analyses (Type 3 analysis of effects), modeling the probability of missing data as a function of relevant observed variables. Across all models, none of the predictors were significantly associated with missing data (all P > .05), suggesting that the data were missing completely at random. Given this result, the subsequent analyses were considered unbiased by the observed patterns of missing data.
Continuous variables were summarized as mean and standard deviation (SD) or median and interquartile range, depending on the normality of their distribution, which was assessed using the Shapiro-Wilk test. Categorical variables were described using frequency counts and percentages. Influential outliers were identified through diagnostic plots such as Cook D and excluded if they were determined to exert undue influence on model estimates. As a result, only 3 participants were excluded from the analyses. Univariate mixed linear models were employed to analyze repeated measures of depression and anxiety scores at ∼12 and ∼36 weeks, with careful assessment of model assumptions, including normality, homogeneity of variances, and appropriate specification of random effects. Variables with a P value <.2 in univariate analyses and no evidence of multicollinearity were included in the multivariable mixed models, adjusting for baseline fat mass percentage as a covariate. Individual differences at baseline were controlled with random intercept model. Intercept is used as a random effect. Body fat mass percentage, baseline body fat mass percentage, body fat mass percentage and physical activity (maximum steps count) interaction, and time variables were used as fixed effects. Statistical significance was determined using a 2-sided α level of 0.05. All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC).
RESULTS
Participants classified as obese exhibited substantially greater adiposity than their nonobese counterparts (BMI 33.5 vs 22.4 kg m−2, P<.0001). The two groups were otherwise demographically comparable: mean age was virtually identical (29.5 vs 28.8 years, P=.27), and median household income did not differ (USD 45,000 vs 40,000, P=.65). Mental health status was also similar, with no significant between-group differences in depressive symptoms (BDI 8.7 vs 7.6, P=.16) or anxiety scores (STAI-State 26 vs 25; STAI-Total 30.5 vs 29; both P>.36). In contrast, lifestyle-related metabolic indices diverged: obese participants demonstrated higher daily energy expenditure (2,536 vs 1,492 kcal, P<.0001) and greater metabolic equivalents (1.566 vs 1.357, P<.0001), accompanied by modestly poorer diet quality as reflected by total HEI scores (60.6 vs 64.1, P =.006). Light and moderate physical-activity durations were comparable (1,107 vs 1,114 minute week−1 and 308 vs 315 minute week−1, respectively; both P>.53). Thus, apart from expected differences in body composition, diet quality, and energy metabolism, the study cohorts were well matched on sociodemographic and mental health characteristics, providing a balanced foundation for subsequent analyses. Details are shown in Supplementary Table 1.
Depression and anxiety symptom scores of all participants are presented in Figure 1. It depicts the mean and SD of depression (BDI) and anxiety (STAI-S, STAI-T) symptom scores for all participants, categorized by weight status (normal weight vs obese) and gestational time points (12 weeks vs 36 weeks). The bar plots compare the changes in symptom scores within each weight group over time. Notably, a significant difference (P < .05) is observed in STAI-S scores between 12 and 36 weeks among obese participants, indicating a change in state anxiety during pregnancy. No other significant differences are detected across time points within either weight group for BDI or STAI-T scores.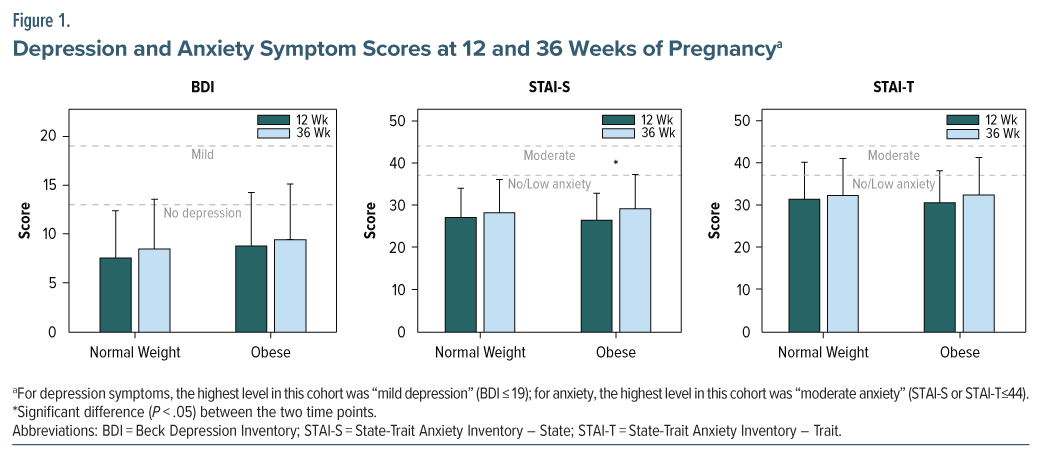
Univariate Analysis
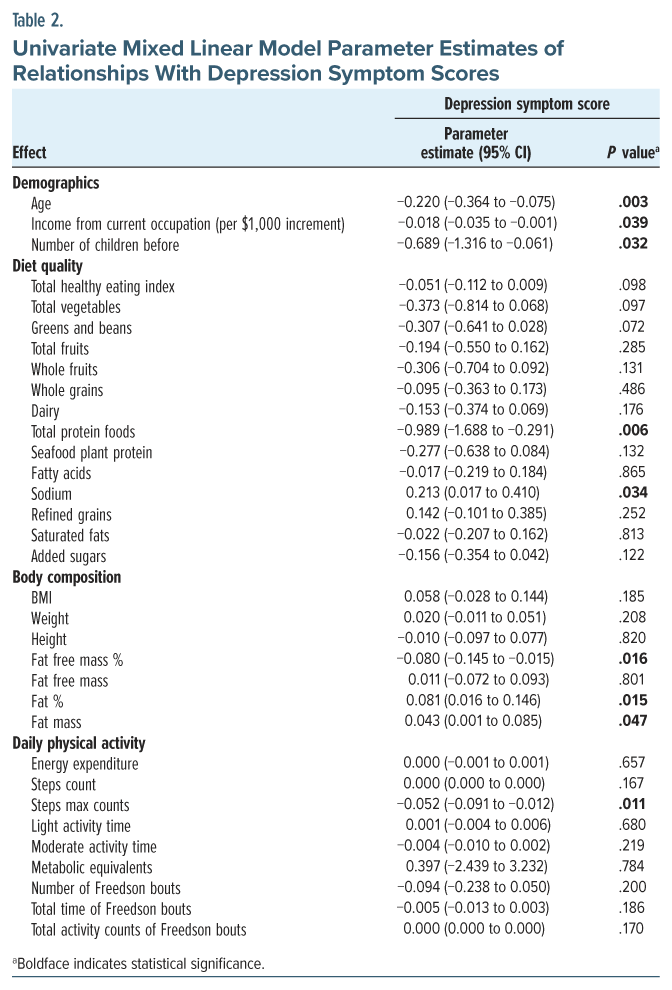
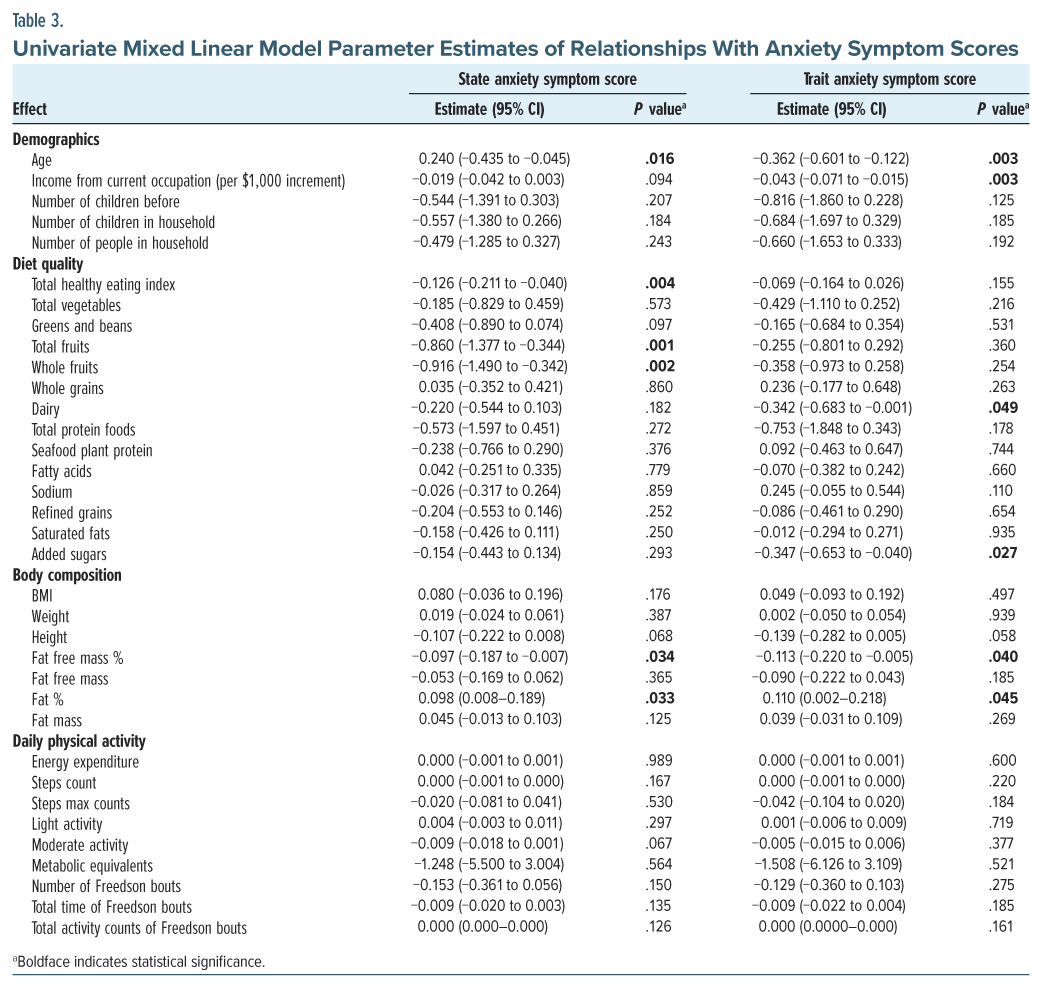
The results of the univariate mixed linear model analyses for factors associated with depression and anxiety symptom scores are presented in Tables 2 and 3, respectively. These analyses identify potential demographic, socioeconomic, dietary, and physiological factors that may contribute to variations in mental health outcomes among pregnant women.
Specifically, the univariate mixed linear model analyses results for relationships with the depression symptom scores are presented in Table 2. A number of parameters showed significant relationships with depression symptom scores during pregnancy. These include demographic and socioeconomic factors such as age, number of children before, and income from current occupation; diet measures such as total protein intake and total sodium intake; body composition parameters such as fat mass percentage and fat free mass percentage; and physical activity measures such as maximum steps count.
The univariate mixed linear model analyses results for the relationships with the anxiety symptom scores are presented in Table 3. Again, a number of parameters (many overlapping with findings in Table 2) showed significant relationships with anxiety symptom scores during pregnancy. These include demographic and socioeconomic factors such as age and income from current occupation; body composition parameters such as fat mass percentage and fat free mass percentage; and diet quality measures such as total HEI, total fruit and whole fruit intake, total dairy, and total added sugar.
Multivariate Analysis
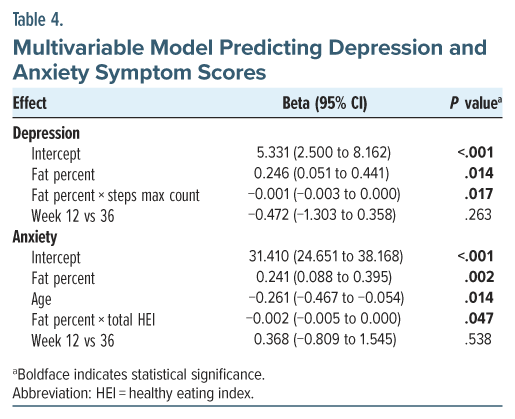
Parameters with P < .2 in the univariate analyses were further examined in the multivariable mixed model analyses, as presented in Table 4.
Specifically, the multivariable analysis showed that the effect of body fat mass percentage on the BDI score was significant, with a positive association observed (β = 0.246, 95% CI, [0.051 to 0.441], P = .014), indicating that higher fat percentage was associated with an increase in the BDI score. Notably, this relationship was moderated by physical activity (ie, maximum steps count), as evidenced by a significant interaction between fat percentage and physical activity (β = −0.001, 95% CI, [–0.003 to 0.000], P = .017). Specifically, the negative estimate for the interaction term suggests that the effect of fat percentage on the BDI score decreases as the maximum steps count increases. Interaction plot of body fat percentage and maximum steps count on BDI scores is shown in Supplementary Figure 1. These findings highlight the potential modifying role of physical activity, as measured by maximum steps count, in mitigating the impact of fat percentage on the BDI score.
Similar as with depression, the results showed that body fat mass percentage was significantly associated with state anxiety scores, with higher fat percentage corresponding to an increase in state anxiety scores (β=0.241, 95% CI, [0.088 to 0.395], P=.002). Age also demonstrated a significant negative association with state anxiety scores (β=−0.261, 95% CI, [0.467 to −0.054], P=.014), indicating that older individuals tended to have lower state anxiety scores. The interaction between fat percentage and total HEI was also significant (β=−0.002, 95% CI, [−0.005 to 0.000], P=.047). The negative estimate suggests that as total HEI increases, the effect of fat percentage on state anxiety scores diminishes, highlighting the potential moderating role of diet quality in mitigating the impact of body fat percentage on state anxiety levels. Interaction plot of body fat percentage and HEI on state anxiety scores (stratified by age) is shown in Supplementary Figure 2. Analogous to the moderating role of physical activity on the BDI scores, these findings indicate that diet quality appears to moderate the role of body fat on state anxiety score.
DISCUSSION
This study investigated the relationships between body composition and mental health during pregnancy, measured by depression and anxiety symptom scores, while evaluating the moderating roles of physical activity and diet quality. Two key findings resulted from the analysis: First, higher fat mass percentage was positively associated with higher depression symptom scores, indicating that increased body fat (ie, as a result of obesity) may lead to increased risk of depression during the prenatal period. Notably, physical activity level (particularly as measured by maximum steps count) attenuated this relationship, suggesting that higher levels of physical activity may mitigate the potential adverse effects of fat mass on depressive symptoms. Second, higher fat percentage was also positively associated with higher anxiety scores, indicating that increased body fat (ie, as a result of obesity) may also lead to increased risk of anxiety. Notably, diet quality (as measured by the HEI) moderated the relationship between fat percentage and anxiety scores, with higher diet quality reducing the potential adverse impacts of fat mass on anxiety symptoms.
The associations between increased fat mass and elevated depression scores align with existing literature emphasizing the negative impact of excess fat on mental health. Obesity and high fat mass are thought to influence depression symptoms through systemic inflammation and hormonal dysregulation, including changes in cortisol and leptin levels.29 Furthermore, the protective role of physical activity observed in this study concurs with prior research, which highlights that exercise enhances mental health by improving endorphin release and reducing inflammation.19 Other studies have also underscored the role of physical activity in alleviating depressive symptoms, further supporting our findings.30 Collectively, these studies and our results suggest that lifestyle interventions targeting physical activity may effectively reduce the psychological burden imposed by depression in patients with high fat mass during pregnancy.
Similar to its effect on depression, obesity also increases the incidence of anxiety due to the degree of metabolic dysfunction. A diet high in saturated fats and added sugar may lead to metabolic dysfunction, neuroinflammation, and consequently mental health disorders. Neuroinflammation alters the structure, excitability, and connectivity of the corticolimbic network, which controls mood, motivation, and emotion.31 While sugar may have a short-term positive effect on anxiety, its long-term impact is generally negative, suggesting the need for moderation and balanced dietary habits.32 Diet quality may be a critical moderating factor in this relationship. High-quality diets, characterized by nutrient-dense foods, have been shown to reduce inflammation and promote mental well-being. A previous study has demonstrated a significant inverse association between diet quality and anxiety levels, underscoring the protective effects of a healthy diet on psychological outcomes.33 Another study reported that dietary improvements, such as increasing fruit, vegetable, and whole grain intake, can alleviate anxiety symptoms, possibly by improving gut-brain interactions and reducing systemic inflammation.34 These findings resonate with our results, highlighting that improved diet quality may mitigate the adverse impacts of fat mass on anxiety symptoms during pregnancy.
The findings of this study are consistent with existing research on the mental health benefits of physical activity and specific dietary patterns. Previous evidence has shown that moderate and regular exercise, along with a healthy diet—rich in high-quality proteins, unsaturated fatty acids, and a variety of fruits and vegetables—can help prevent and alleviate symptoms of depression and anxiety.35–37 During pregnancy, a unique physiological stage, women face an increased risk of mental health challenges. However, research suggests that physical activity and a balanced diet remain effective interventions during this period.38–40 Our findings further indicate that despite substantial changes in weight and body composition during pregnancy, appropriate exercise and nutritional intake are still associated with reduction of depressive and anxiety symptoms, suggesting their potential as preventive strategies. Therefore, incorporating appropriate physical activity and nutritional guidance into routine maternal health management as a supplementary approach to prevent perinatal and postpartum mental health problems may be important. Future research may explore the specific mechanisms by which different types of exercise or dietary patterns influence mental health during pregnancy, in order to refine and optimize personalized intervention strategies.
While our study has many strengths such as its longitudinal and prospective design and comprehensive evaluation of body composition, physical activity, diet, and mental health, several limitations warrant consideration. First, despite its longitudinal design, causal relationships cannot be demonstrated based on its observational nature. Second, self-reported dietary data are subject to recall bias, particularly when assessing intake over a month-long period. While alternative methods such as multiday dietary record may offer improved accuracy, the NIH Food Frequency Questionnaire in this study has been validated across diverse populations and is widely applied in large-scale epidemiological research.41,42 Additionally, we acknowledge that pregnancy-related factors at different trimesters, such as nausea or concerns about fertility and pregnancy loss, could influence dietary patterns, mental health, and physical activity. Although we did not collect direct measures of these variables, the consistency of HEI scores across gestational weeks (12, 24, and 36) and similar trajectories between BMI groups suggests that their potential confounding effects may be limited. Our focus was on evaluating the moderating role of diet in the relationship between body composition and mental health, rather than identifying the determinants of dietary change. Third, the study population was relatively homogeneous in terms of demographic characteristics and was also relatively healthy with minimal to mild/ moderate mental health symptoms, which may limit the generalizability of the findings. Fourth, potential collinearity among body composition, physical activity, and diet variables may have influenced the interpretation of moderation effects. In addition, the study did not include data on pre-pregnancy mental health symptoms or body composition, which limits our ability to assess the directionality of the associations observed. The relationships may be bidirectional, and future research with preconception data is needed to clarify these dynamics.
CONCLUSIONS
In summary, our findings on a prospective and longitudinal study cohort indicate that body composition properties—specifically high fat mass percentage—are associated with high depression and anxiety symptoms scores during pregnancy. However, these relationships may be modifiable, as higher levels of physical activity and better diet quality may mitigate the potential negative impacts of fat mass on mental health during pregnancy. These results underscore the importance of promoting healthy lifestyle behaviors, including regular exercise and adherence to high-quality dietary patterns, as effective strategies for promoting mental health during pregnancy, particularly for women with obesity.
Article Information
Published Online: September 15, 2025. https://doi.org/10.4088/JCP.25m15822
© 2025 Physicians Postgraduate Press, Inc.
Submitted: February 3, 2025; accepted June 25, 2025.
To Cite: Huang Y, Akmyradov C, Keene MT, et al. Relationships between body composition and mental health during pregnancy are moderated by physical activity and diet. J Clin Psychiatry 2025;86(4):25m15822.
Author Affiliations: Department of Radiology, University of Arkansas for Medical Sciences, Little Rock, Arkansas (Huang, Na, Ou); Arkansas Children’s Research Institute, Little Rock, Arkansas (Akmyradov, Ou); Arkansas Children’s Nutrition Center, Little Rock, Arkansas (Keene, Chambers, Durey, Ou); Department of Pediatrics, University of Arkansas for Medical Sciences, Little Rock, Arkansas (Bellando, Ou).
Corresponding Author: Xiawei Ou, PhD, 1 Children’s Way, Slot 105, Little Rock, AR 72202 ([email protected]).
Relevant Financial Relationships: All authors declare no relevant financial relationships or conflicts of interest.
Funding/Support: This study was supported in part by the National Institute of Health (NIH R01HD099099) and the Agriculture Research Service of US Department of Agriculture (USDA-ARS 6026-10700-001-000D).
Role of the Funder: The NIH grant supported personnel efforts and experimental costs; the USDA grant provided supplemental effort support and facilities and resources.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the US Department of Agriculture.
ORCID: Yali Huang: https://orcid.org/0000-0001-8263-6368;
Chary Akmyradov: https://orcid.org/0000-0002-2579-7146;
Xiaoxu Na: https://orcid.org/0000-0001-7714-1344;
Jayne Bellando: https://orcid.org/0000-0003-1986-6288;
Xiawei Ou: https://orcid.org/0000-0001-9815-0127
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Mental health in pregnant women with obesity may be impacted by physical activity and diet, but more studies are needed to delineate relationships between these factors.
- Higher body fat was associated with increased depression and anxiety symptoms. Physical activity moderated the effect of body fat on depression, while diet quality moderated the effect of body fat on anxiety.
Editor’s Note: We encourage authors to submit papers for consideration as a part of our Focus on Women’s Mental Health section. Please contact Marlene P. Freeman, MD, at Psychiatrist.com/contact/freeman.
References (42)

- Catalano PM, Shankar K. Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ. 2017:356.
- Poston L, Harthoorn LF, Van Der Beek EM, et al. Obesity in pregnancy: implications for the mother and lifelong health of the child. A consensus statement. Pediatr Res. 2011;69(2):175–180. PubMed CrossRef
- Yang Z, Feng G, Gao X, et al. Maternal adiposity and perinatal and offspring outcomes: an umbrella review. Nat Hum Behav. 2024;8(12):2406–2422. PubMed CrossRef
- O’callaghan M, Williams G, Andersen M, et al. Prediction of obesity in children at 5 years: a cohort study. J Paediatr Child Health. 1997;33(4):311–316. PubMed
- Whitaker RC. Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics. 2004;114(1):e29–e36. PubMed CrossRef
- Boney CM, Verma A, Tucker R, et al. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115(3):e290–e296. PubMed CrossRef
- Drake AJ, Reynolds RM. Focus on obesity: impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction. 2010;140(3):387–398. PubMed CrossRef
- Gaillard R, Steegers EA, Duijts L, et al. Childhood cardiometabolic outcomes of maternal obesity during pregnancy: the generation R study. Hypertension. 2014;63(4):683–691. PubMed CrossRef
- Fisher J, Cabral de Mello M, Patel V, et al. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139–149. PubMed CrossRef
- Sulley S, Adzrago D, Mamudu L, et al. Assessment of prenatal depression among US pregnant women without access to paid sick leave and regular place of care: National Health Interview Survey of US-born and non-US-born. Prev Med Rep. 2023;35:102322. PubMed CrossRef
- Fawcett EJ, Fairbrother N, Cox ML, et al. The prevalence of anxiety disorders during pregnancy and the postpartum period: a multivariate Bayesian meta-analysis. J Clin Psychiatry. 2019;80(4):18r12527. PubMed CrossRef
- Molyneaux E, Poston L, Ashurst-Williams S, et al. Obesity and mental disorders during pregnancy and postpartum: a systematic review and meta-analysis. Obstet Gynecol. 2014;123(4):857–867. PubMed CrossRef
- GriffithsShannonBrown AOMT, Davison MOM, Brown T, et al. Associations between anxiety, depression, and weight status during and after pregnancy: a systematic review and meta-analysis. Obes Rev. 2024;25(3):e13668. PubMed CrossRef
- Bąk-SosnowskaNaworska MB, Naworska B. Medical and psychological aspects of pregnancy in women with obesity and after bariatric surgery. Nutrients. 2023;15(19):4289. PubMed CrossRef
- Zhang J. The bidirectional relationship between body weight and depression across gender: a simultaneous equation approach. Int J Environ Res Public Health. 2021;18(14):7673. PubMed CrossRef
- Pan A, Sun Q, Czernichow S, et al. Bidirectional association between depression and obesity in middle-aged and older women. Int J Obes. 2012;36(4):595–602. PubMed CrossRef
- Rachubińska K, Mińko A, Rotter I, et al. The Association between obesity, chronic inflammation, metabolic disorders and mood disorders among patients up to 12 months after hospitalization for SARS-CoV-2. Diagnostics. 2024;14(21):2357. PubMed CrossRef
- Yaktine AL, Rasmussen KM. Weight gain during pregnancy: reexamining the guidelines. 2010.
- Davenport MH, Meah VL, Ruchat S-M, et al. Impact of prenatal exercise on neonatal and childhood outcomes: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1386–1396. PubMed CrossRef
- Baskin R, Hill B, Jacka FN, et al. The association between diet quality and mental health during the perinatal period. A systematic review. Appetite. 2015;91:41–47. PubMed CrossRef
- Casas I, Nakaki A, Pascal R, et al. Effects of a Mediterranean Diet intervention on maternal stress, Well-Being, and sleep quality throughout Gestation—The IMPACT-BCN trial. Nutrients. 2023;15(10):2362. PubMed CrossRef
- von Zimmermann C, Winkelmann M, Richter-Schmidinger T, et al. Physical activity and body composition are associated with severity and risk of depression, and serum lipids. Front Psychiatry. 2020;11:494. PubMed CrossRef
- Torres L, Caciula MC, Tomoiaga AS, et al. Correlations between mental health, physical activity, and body composition in American college students after the COVID-19 pandemic lockdown. Int J Environ Res Public Health. 2023;20(22):7045. PubMed CrossRef
- Roland CB, Seyedhosseini P, Knudsen SDP, et al. Effects of prenatal exercise interventions on maternal body composition: a secondary analysis of the FitMum randomized controlled trial. PLOS One. 2024;19(8):e0308214. PubMed CrossRef
- Most J, Marlatt KL, Altazan AD, et al. Advances in assessing body composition during pregnancy. Eur J Clin Nutr. 2018;72(5):645–656. PubMed CrossRef
- Butte NF, Ellis KJ, Wong WW, et al. Composition of gestational weight gain impacts maternal fat retention and infant birth weight. Am J Obstet Gynecol. 2003;189(5):1423–1432. PubMed CrossRef
- Beck AT, Steer RA, Brown G. Beck depression inventory–II. Psychol Assess. 1996.
- Speilberger CD, Gorsuch R, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists; 1983.
- Milaneschi Y, Simmons WK, van Rossum EF, et al. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24(1):18–33. PubMed CrossRef
- Stubbs B, Vancampfort D, Firth J, et al. Relationship between sedentary behavior and depression: a mediation analysis of influential factors across the lifespan among 42,469 people in low-and middle-income countries. J Affect Disord. 2018;229:231–238. PubMed CrossRef
- Fulton S, Décarie-Spain L, Fioramonti X, et al. The menace of obesity to depression and anxiety prevalence. Trends Endocrinol Metabolism. 2022;33(1):18–35.
- Zhang L, Sun H, Liu Z, et al. Association between dietary sugar intake and depression in US adults: a cross-sectional study using data from the National Health and Nutrition Examination Survey 2011–2018. BMC psychiatry. 2024;24(1):110. PubMed CrossRef
- Jacka FN, Mykletun A, Berk M, et al. The association between habitual diet quality and the common mental disorders in community-dwelling adults: the Hordaland Health study. Psychosom Med. 2011;73(6):483–490. PubMed CrossRef
- O’neil A, Quirk SE, Housden S, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health. 2014;104(10):e31–e42. CrossRef
- Dalle Grave R. Nutrition and Fitness: Mental Health. MDPI; 2020:1804. CrossRef
- Marx W, Moseley G, Berk M, et al. Nutritional psychiatry: the present state of the evidence. Proc Nutr Soc. 2017;76(4):427–436. PubMed CrossRef
- Mikkelsen K, Stojanovska L, Polenakovic M, et al. Exercise and mental health. Maturitas. 2017;106:48–56. PubMed CrossRef
- Cai C, Busch S, Wang R, et al. Physical activity before and during pregnancy and maternal mental health: a systematic review and meta-analysis of observational studies. J Affect Disord. 2022;309:393–403. PubMed CrossRef
- He L, Soh KL, Huang F, et al. The impact of physical activity intervention on perinatal depression: a systematic review and meta-analysis. J Affect Disord. 2023;321:304–319. PubMed CrossRef
- Yelverton CA, Rafferty AA, Moore RL, et al. Diet and mental health in pregnancy: nutrients of importance based on large observational cohort data. Nutrition. 2022;96:111582. PubMed CrossRef
- Zheng M, Campbell KJ, Scanlan E, et al. Development and evaluation of a food frequency questionnaire for use among young children. PloS one. 2020;15(3):e0230669. PubMed CrossRef
- Bailey RL. Overview of dietary assessment methods for measuring intakes of foods, beverages, and dietary supplements in research studies. Curr Opin Biotechnol. 2021;70:91–96. PubMed CrossRef
This PDF is free for all visitors!