Though antibiotics have become foundational in modern medicine, their administration is not without adverse effects. Neuropsychiatric side effects are rare but insufficiently studied and encompass anxiety, insomnia, delirium, and psychosis.1 Amoxicillin, a commonly used penicillin-based antibiotic, is generally well-tolerated and effective, particularly in pediatric patients.2 The propensity for psychotic disorders to initially manifest in mid-adolescence through early adulthood makes the potential for antibiotic-induced psychosis especially relevant in this demographic.3 This case report presents the first known instance, to our knowledge, of first-episode psychosis in an adolescent following amoxicillin administration.
Case Report
A 17-year-old male with a history of mild major depressive disorder presented to the emergency department (ED) with acute homicidal ideation, disorganized behavior, heightened religious preoccupation, disorientation, and auditory and visual hallucinations. The patient also reportedly experienced symptoms of anxiety and had been prescribed fluoxetine about 1 year prior to presentation but reported a trial of only about 2 weeks before discontinuing due to no perceived benefits. There was no known psychiatric follow-up or reported side effects during this period, and no other psychiatric medications were identified from chart review. His only current medication was amoxicillin (500 mg 3 times/d) for presumed sinusitis taken for 5 days. There was no family history of psychiatric disorders.
The patient was admitted to the psychiatry unit for first-episode psychosis evaluation. Comprehensive laboratory tests, including a urine drug screen and synthetic cannabinoid panel, were negative. The patient acknowledged cannabis use 2 months prior, though chart review showed no positive toxicology screens. Given literature reports of antibiotic-induced psychosis, amoxicillin was discontinued. Symptoms resolved over 6 days with risperidone (1 mg twice/d, tapered to 1 mg every night at bedtime).
He was readmitted 2 days later due to auditory hallucinations after missing a dose of risperidone. A computed tomography head scan without contrast showed no abnormalities, and repeat drug screens were negative. During this 2-week readmission, the patient was treated with olanzapine (5 mg every night at bedtime, increased to 7.5 mg every night at bedtime) and then transitioned to paliperidone (6 mg by mouth every night at bedtime, followed by long acting injectable 234 mg and 156 mg) and discharged, supplemented by propranolol for akathisia and hydroxyzine for anxiety.
Within 2 weeks, he returned to the ED twice for escalating akathisia, which was resolved with the addition of clonazepam and increased propranolol. Psychotic symptoms remained well managed with paliperidone. Presently, the working diagnosis is substance-induced psychosis vs unspecified schizophrenia spectrum disorder.
Discussion
Although antibiotics are generally safe, neuropsychiatric side effects are important to consider in the appropriate clinical context. Psychosis has been linked as a major neurotoxic side effect of macrolides, fluoroquinolones, sulfonamides, and isoniazid.1 While amoxicillin has a lower risk, psychotic symptoms can still occur.1 Several hypotheses for the mechanism behind CNS involvement have been suggested, ranging from effects on neurotransmitter function to impact on the gut microbiome that may also increase blood-brain barrier permeability.1,4 Certain cases also suggest a dose-dependent relationship, as shown in patients with toxic antibiotic concentrations or impaired renal function.5,6
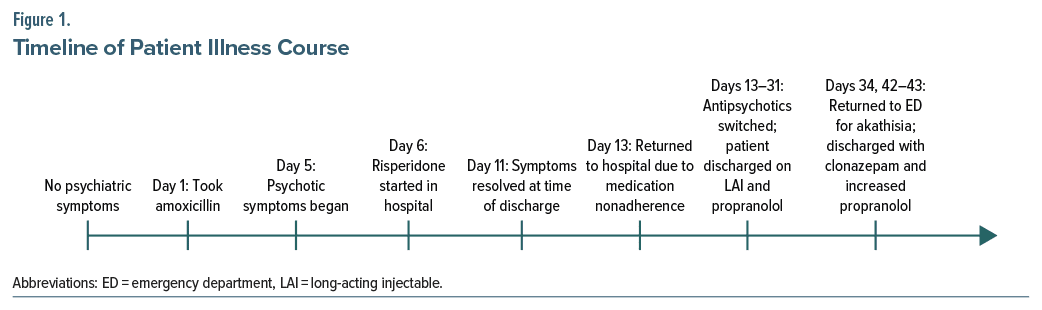
This case of first-episode psychosis associated with amoxicillin in an adolescent underscores the need for awareness of potential neuropsychiatric side effects of antibiotics. While certain symptoms could be attributed to adverse effects of fluoxetine, the patient had an insufficient trial from roughly 1 year prior to presentation, thus singling out amoxicillin given its temporal relationship to illness onset and the results from the literature review. Additionally, use of the Naranjo Adverse Drug Reaction Probability Scale indicates a possible reaction due to amoxicillin given previous reports and timing of symptom onset.7 Figure 1 illustrates the timeline of this patient’s presentation.
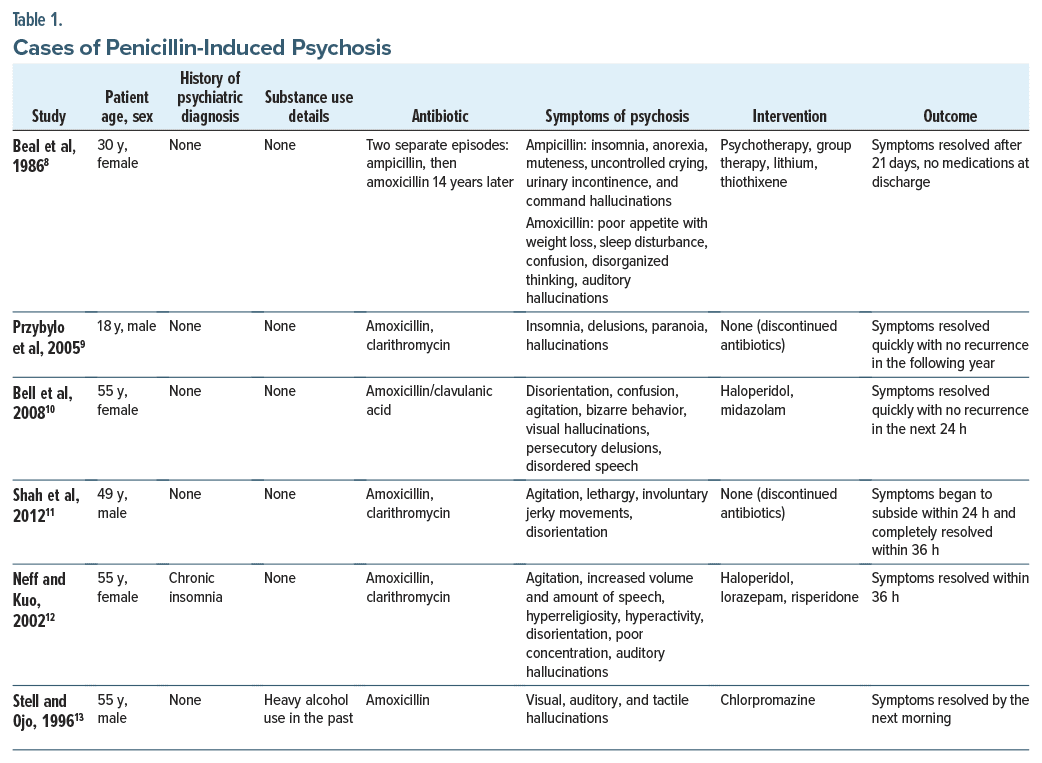
Several similar cases of penicillin induced psychosis compiled from PubMed using the search terms “amoxicillin and psychosis,” summarized in Table 1, showed swift resolution of symptoms upon antibiotic discontinuation in patients with an average age of 44 years. However, this patient experienced a protracted course of psychosis despite discontinuation, suggesting the possibility of a gene-environment interaction contributing to the development of a schizophrenia spectrum disorder. This hypothesis is supported by research in other areas, such as the role of cannabinoids in precipitating schizophrenia in genetically susceptible individuals. At this time, the patient’s only risk factors for a psychotic disorder were either related to substance use (both his reported recreational use and this amoxicillin-related incident) or his general demographics.
In conclusion, this case highlights the importance of early recognition of antibiotic-associated psychosis in adolescents. When psychiatric symptoms align with antibiotic initiation, thorough history taking is essential to identify potential iatrogenic causes. Future research is necessary to elucidate the mechanisms behind antibiotic-induced psychosis, explore potential dose-dependent relationships, and develop management guidelines. Such research will enhance clinicians’ ability to prevent, recognize, and treat antibiotic-associated neuropsychiatric complications.
Article Information
Published Online: May 27, 2025. https://doi.org/10.4088/PCC.24cr03854
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(3):24cr03854
Submitted: September 17, 2024; accepted January 22, 2025.
To Cite: Li KD, Irani K, Shah K, et al. Exploring antibiotic-related psychotic episodes in adolescents. Prim Care Companion CNS Disord 2025;27(3): 24cr03854.
Author Affiliations: Department of Psychiatry and Behavioral Medicine, Atrium Health Wake Forest Baptist, Winston-Salem, North Carolina (all authors).
Corresponding Author: Kaushal Shah, MD, MPH, MBA, Department of Psychiatry and Behavioral Medicine, Atrium Health Wake Forest Baptist, 1 Medical Center Blvd, Winston-Salem, NC 27157 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (13)

- Bangert MK, Hasbun R. Neurological and psychiatric adverse effects of antimicrobials. CNS Drugs. 2019;33(8):727–753. PubMed CrossRef
- Akhavan BJ, Khanna NR, Vijhani P. Amoxicillin. In: StatPearls [Internet]. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK482250/
- Albin K, Albin C, Jeffries CD, et al. Clinician recognition of first episode psychosis. J Adolesc Health. 2021;69(3):457–464. PubMed CrossRef
- Wu Q, Zhang Y, Zhang Y, et al. Potential effects of antibiotic-induced gut microbiome alteration on blood brain barrier permeability compromise in rhesus monkeys. Ann N Y Acad Sci. 2020;1470(1):14–24. PubMed CrossRef
- Guo Y, Shao X, Zhang L, et al. A case of suspected antibiotic-associated encephalopathy in a patient undergoing long-term peritoneal dialysis. J Int Med Res. 2020;48(5):300060520924507. PubMed CrossRef
- Nanjundappa A, Munankami S, Al Talib K, et al. Ceftriaxone-induced encephalopathy in a patient with end-stage renal disease on hemodialysis. Cureus. 2023;15(9):e46226. PubMed CrossRef
- Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–245. PubMed CrossRef
- Beal DM, Hudson B, Zaiac M. Amoxacillin-induced psychosis? Am J Psychiatry. 1986;143(2):255–256. PubMed CrossRef
- Przybylo HJ, Przybylo JH, Todd Davis A, et al. Acute psychosis after anesthesia: the case for antibiomania. Paediatr Anaesth. 2005;15(8):703–705. PubMed CrossRef
- Bell CL, Watson B, Waring WS. Acute psychosis caused by co-amoxiclav. BMJ. 2008;337:a2117. PubMed CrossRef
- Shah M, Subhani M, Rizvon K, et al. Transient psychotic episode induced by Helicobacter pylori triple therapy treatment. Case Rep Gastroenterol. 2012;6(2):381–386. PubMed CrossRef
- Neff NE, Kuo G. Acute manic psychosis induced by triple therapy for H. pylori. J Am Board Fam Pract. 2002;15(1):66–68. PubMed
- Stell IM, Ojo OA. Amoxycillin-induced hallucinations-a variant of Hoigne’s syndrome? Br J Clin Pract. 1996;50(5):279. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!