Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(4):24f03899
Author affiliations are listed at the end of this article.
Have you been unsure about when and why stress reactions morph into posttraumatic stress disorder (PTSD) and when and how they should be treated? Have you been uncertain about what predisposes people to develop PTSD after a traumatic experience? Have you struggled to treat or refer your patients for specialty help? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Mr A, a 42-year-old married man, was admitted to the hospital after he was struck by a motor vehicle. He sustained a mild traumatic brain injury (mTBI), with loss of consciousness that lasted less than 30 minutes (as noted by witnesses and medics at the scene), a fractured right wrist, a dislocated right shoulder, as well as a right tibia and fibula fracture, for which he required stabilization in the intensive care unit (ICU). After his ICU stay, he was transferred to a unit with orthopedic and physical medicine and rehabilitation services, including physical therapy and occupational therapy. He had no prior psychiatric treatment or hospitalizations. He was seen for a psychiatric consultation 3 weeks into his hospitalization due to difficulties in progressing with his rehabilitation, as well as symptoms of anxiety, pain, and tearfulness.
On evaluation, Mr A reported difficulty with sleeping, frequent nightmares (related to death and dying in the hospital), and heightened anxiety about his condition. He was concerned about his ongoing pain, and he wondered whether his symptoms would interfere with his returning to work. He described having a partial memory for events leading up to his accident and his time in the ICU. He was anxious and visibly tearful, feeling overwhelmed by his recovery process.
DISCUSSION
What Are the Diagnostic Criteria for PTSD, and How Does It Differ From Acute Stress Disorder?
PTSD is one of the most highly prevalent psychiatric disorders, affecting approximately 5% of individuals in any given year and 6% of individuals during their lifetimes.1 PTSD is twice as common in women than in men. Trauma-exposed populations (eg, military veterans and first responders) experience higher rates than do matched controls. It also co-occurs frequently with other psychiatric conditions (eg, substance use disorder [SUD] and mood disorders).1 Acute stress disorder (ASD) can be distinguished from PTSD because the symptom pattern in ASD is limited to 3 days to 1 month after exposure to the traumatic event.2
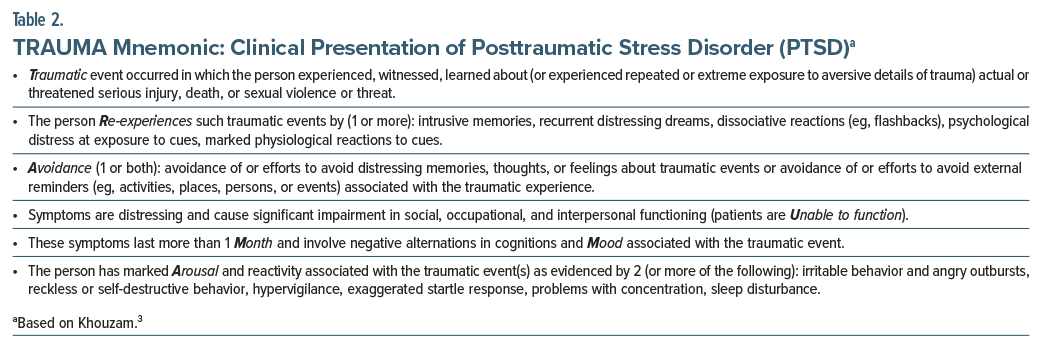
PTSD diagnostic criteria consist of 6 criteria (A–H). PTSD can develop after someone has been exposed to an actual or threatened death, serious injury, or sexual violence via direct exposure, witnessing the event in person, learning that it happened to a close family member or friend, or being repeatedly exposed to stressful reminders of the traumatic event(s) (Criterion A).2 This diagnosis is unique among Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR)2 disorders in that it requires that trauma exposure precedes onset or exacerbation of symptoms. Diagnosis of PTSD also includes 4 main symptom clusters: intrusions (Criterion B), avoidance (Criterion C), impaired cognition and mood (Criterion D), and alterations in arousal and reactivity (Criterion E) (see the DSM-5-TR, as well as Table 1 for the Posttraumatic Checklist-5 [PCL-5], which provides a structured diagnostic overview and is widely used in clinical and research settings). These symptom clusters can be recalled by the mnemonic “TRAUMA” (Table 2).2,3
ASD diagnostic criteria share the same Criterion A as PTSD and consist of 5 criteria (A–E). ASD has similar symptoms to PTSD but is distinguished by its shorter symptom duration. As stated previously, in ASD, the symptom pattern is limited to 3 days to 1 month after exposure to the traumatic event (see DSM-5-TR for full ASD diagnostic criteria), whereas PTSD requires symptoms to persist for more than 1 month.
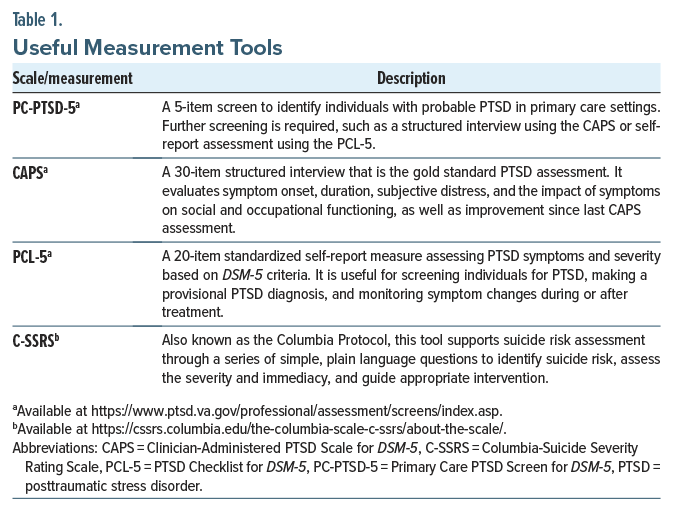
What Validated Assessments Can Be Used to Identify and Diagnose PTSD?
PTSD is a clinical diagnosis rather than a condition that can be established by imaging, laboratory, or physiological metrics (see Table 1 for a list of useful measures, descriptions, and where to obtain them). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) is a 5-item questionnaire that is widely used in primary care settings to identify probable PTSD with excellent diagnostic accuracy.4–6 The PC-PTSD-5 assesses Criterion A traumatic stressors and other PTSD symptoms (eg, re-experiencing, avoidance, hypervigilance, emotional numbness, and guilt/self-reproach). Research in a large sample of VA primary care patients found that use of a cut point of 4 is optimal for men but not for women, as this cut point resulted in high numbers of false negatives. Therefore, a lower cut point for women may be indicated.6 However, positive PC-PTSD-5 screens require further assessment, ideally with the use of validated structured clinician-administered interviews (eg, the Clinician-Administered PTSD Scale for DSM-5 [CAPS-5]) to diagnose PTSD.7,8 To detect changes in PTSD symptom severity over time, evidence supports use of validated instruments (eg, the PTSD Checklist for DSM-5 [PCL-5]) or a structured clinician-administered interview (eg, CAPS-5).9–11
According to the US Preventive Services Task Force (USPSTF), there is insufficient evidence to recommend routine PTSD screening in the general population. However, the USPSTF does recommend screening for anxiety disorders in adults aged <65 years, which may help identify individuals with PTSD symptoms due to symptom overlap between the conditions.12 In high-risk populations, such as those seen in urban community health centers, targeted screening for PTSD may be especially important to ensure timely identification and intervention.
What Conditions Commonly Co-Occur With PTSD, and How Can They Be Differentiated?
Individuals with PTSD are 80% more likely than those without PTSD to have symptoms that meet diagnostic criteria for at least 1 other psychiatric condition (eg, SUDs).2 Some of the most prevalent conditions associated with PTSD are major depressive disorder (MDD), alcohol use disorder (AUD), and other anxiety disorders.13 Following trauma, individuals often develop both PTSD and MDD, rather than 1 or the other, and both should be diagnosed and treated when present. Self-medication of PTSD often involves use of alcohol and illicit substances.14 Similarly, generalized anxiety disorder (GAD) occurs in 40% of individuals with PTSD, which leads to more intense symptoms and greater impairment than in individuals with GAD alone.15 Certain phobias, specifically social phobia, are also highly comorbid with PTSD.16
PTSD is among the most frequently diagnosed psychiatric disorders associated with mTBI. Studies of veterans, service members, and civilians indicate that the risk of PTSD is elevated 2- to 3-fold following mTBI.17–19 Co-occurrence of PTSD and mTBI occurred in nearly half of US military personnel and deployed combat veterans (in the Iraq/Afghanistan wars). Mild TBIs in soldiers deployed to Iraq have been strongly associated with PTSD and physical health problems several months after soldiers return home.20 Certain physical health problems (including bone and joint disease, metabolic diseases, neurological conditions, respiratory conditions, and cardiovascular conditions) have also been independently associated with PTSD.14
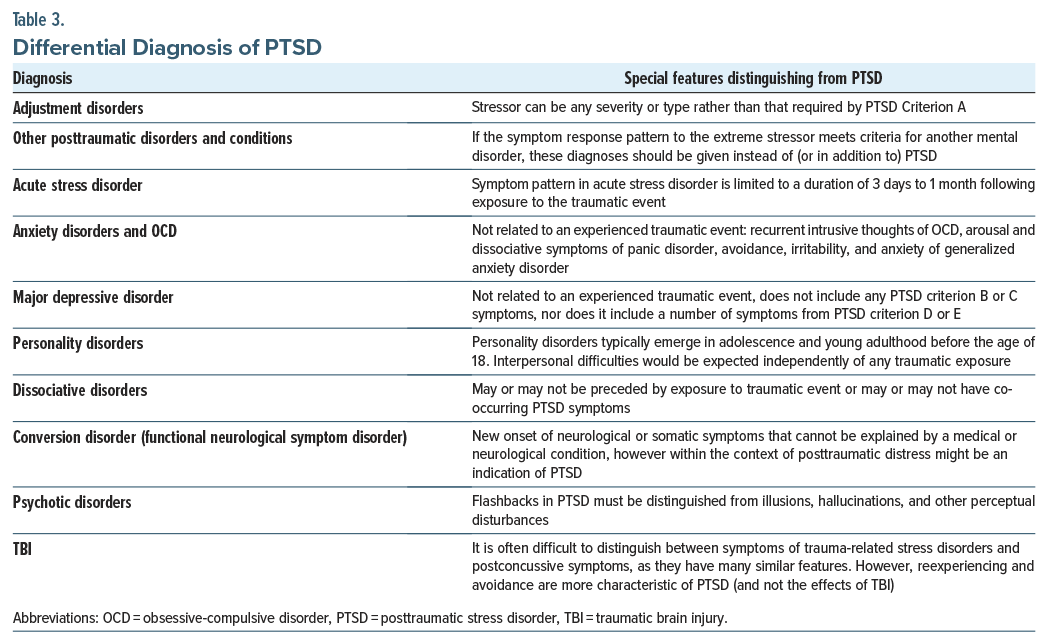
Many of these conditions, such as GAD, MDD, and panic disorder, can present with similar symptomatology to PTSD, complicating its diagnosis. For example, individuals with GAD have a history of anxiety across a wide range of circumstances, whereas those with PTSD often experience anxiety in response to a major trauma.21 Individuals with depression, whether comorbid or trauma-related, may feel hopelessness, intense shame, or guilt. When patients with PTSD experience these symptoms, they may be primarily focused on the trauma-related event(s) that occurred. Those with panic disorder experience intense anxiety, which can be related to a specific object or situation. In these cases, one might avoid a specific situation to prevent a panic attack. Similarly, individuals with PTSD may also avoid certain situations (see Table 3 for the differential diagnosis of PTSD).2 Table 3 provides a structured comparison of conditions that not only share overlapping symptoms with PTSD but also have distinct diagnostic criteria. Accurate differentiation is essential, as disorders such as GAD, panic disorder, and obsessive-compulsive disorder can present with anxiety and avoidance behaviors without the history of trauma exposure. Similarly, while TBI can lead to cognitive and emotional disturbances, PTSD is more specifically characterized by reexperiencing and avoidance symptoms. The table also clarifies distinctions between PTSD and conditions like MDD, dissociative disorders, and psychotic disorders, helping to guide accurate diagnosis and treatment planning.
Beyond psychiatric comorbidities, PTSD is also associated with sleep disturbances, including insomnia, nightmares, and obstructive sleep apnea. In addition, individuals with PTSD also have an increased risk of cardiovascular disease and metabolic disorders, which may be influenced by chronic stress and autonomic dysregulation. Recognizing these comorbidities is important for comprehensive care, as managing both PTSD and associated medical conditions can improve overall health outcomes.
Why Might PTSD Develop?
PTSD is associated with changes in neurophysiology and the brain’s anatomy, including a reduced hippocampal size and an overactive amygdala, which have been observed in individuals with chronic PTSD and are thought to result from prolonged stress exposure rather than preexisting risk factors.22 The medial prefrontal cortex, which provides inhibitory control over the emotional reactivity of the amygdala, appears to be smaller and less responsive in those with PTSD, ie, the stress-response system reacts inappropriately to the stressors/trauma. This leads to difficulties adapting to, and recovering from, the traumatic event, which results in an impaired extinction of the fear response.22 In addition, alterations in brain-derived neurotrophic factor levels have been implicated in PTSD, suggesting a role in stress-related neuroadaptations.23
Those who suffer from PTSD may also experience an increased startle response and disrupted sleep related to increased sympathetic nervous system (SNS) reactivity.24 With the balance of SNS and parasympathetic nervous system activity disrupted, an autonomic imbalance can result in an increase of basal activity and an intermittent exaggerated demand on the cardiovascular system.25 The hypothalamic-pituitary-adrenal axis is the body’s major response system for stress.22 The hypothalamus secretes corticotropin-releasing hormone, which binds to receptors on pituitary cells and subsequently produces/releases adrenocorticotropin hormone (ACTH). ACTH is then transported to the adrenal gland where adrenal hormones (eg, cortisol) are produced/released. The release of cortisol activates SNS pathways and generates negative feedback to both the hypothalamus and the anterior pituitary. This negative feedback system appears dysfunctional in those with PTSD.22
Who Is Prone to Developing PTSD After a Traumatic Event?
Several meta-analyses have identified empirically validated risk factors for the development of PTSD, often categorized as pretraumatic factors, peri-traumatic factors, and posttraumatic factors.14 Pretraumatic factors exist before the trauma and may influence risk or resilience. Peri-traumatic factors refer to experiences occurring during or immediately after the traumatic event, including emotional, cognitive, and physiological responses, while posttraumatic describes responses or adaptations that emerge afterward. Pretraumatic risk factors include those that occurred before the trauma, relating to temperament (ie, early childhood emotional problems and prior mental disorders), the environment (ie, lower socioeconomic status, lower education, prior trauma exposure or adversity, lower intelligence, minoritized racial/ethnic status, and family psychiatric history), and genetic and physiological factors (eg, female gender and younger age at time of trauma exposure [for adults]).2 Peri-traumatic risk factors also include environmental risk factors (eg, the severity/dose of trauma, the perception of life threat, interpersonal violence, personal injury) and have been associated with an increased likelihood of developing PTSD. For military personnel, risk factors also involve being a perpetrator, witnessing atrocities, or killing the enemy. Posttraumatic risk factors (eg, negative appraisals and limited coping skills, repeated upsetting reminders, and subsequent adverse life events) are factors that occur after the traumatic event.2 As detailed above, the risk of PTSD is 2–3 times more likely after mTBI in studies of veterans, service members, and civilians.
Certain groups are also especially vulnerable to trauma sequelae and to PTSD. Among these are members of racial and sexual minorities, individuals who have suffered sexual trauma, and those who have experienced adverse childhood experiences (ACEs).26,27 The original ACEs study was developed based on data from middle class, predominantly white families in 1950s Kaiser Permanente cohorts. Since then, trauma frameworks have evolved to better reflect the diverse experiences of low-income, minority, and urban populations, recognizing a broader spectrum of adversity and structural inequities that contribute to long-term health outcomes. In the United States, the lifetime PTSD prevalence has been highest among blacks, intermediate among Hispanic and white individuals, and lowest among Asians. Furthermore, racial discrimination and peri-traumatic dissociation increase the risk of developing PTSD.28 Peri-traumatic dissociation is the complex process of disorientation, depersonalization, and derealization that arises during a traumatic event. Frequent racial discrimination may increase the propensity for peri-traumatic dissociation in the context of new traumatic experiences and contribute to the development of PTSD symptoms.28 Compared to white individuals, minorities have been less likely to seek treatment for PTSD symptoms, with fewer than half seeking treatment.29
Individuals with a history of ACEs are also associated with a higher likelihood of developing PTSD.30–32 The ACE Questionnaire is a widely used scale that assesses physical, emotional, and sexual abuse and household dysfunction (eg, alcohol or drug misuse, having a parent who engaged in violent or criminal behavior in the household, and mental illness in the family).33
Certain types of trauma are correlated with a greater severity of posttraumatic stress symptoms, specifically combat-related trauma and sexual trauma. In military populations, 20% of PTSD cases result from sexual trauma, which affects both men and women and can occur regardless of deployment history. Furthermore, traumas can co-occur (eg, neglect with sexual trauma).34
What Are the Complications of PTSD?
Complications of PTSD extend into multiple facets of life (eg, impacting physical health, psychological wellness, social relationships) and can lead to suicide. Beyond suicide risk, PTSD is associated with significant impairments in relationships, occupational functioning, and overall quality of life, which can contribute to the chronicity of symptoms and increase vulnerability to suicidality. In addition, studies reveal a connection among greater posttraumatic stress symptomatology and more chronic medical conditions, including cardiovascular disease, metabolic dysregulation, and certain autoimmune diseases.35
From a psychological perspective, trauma survivors are at increased risk of depression, anxiety, sensitivity to abandonment/rejection, and difficulties establishing trust. This can interfere with psychosocial functioning and lead to further isolation or unstable relationships. Early childhood traumas are exceptionally harmful, as these can result in impaired early attachments, especially if the caregiver is also the abuser. Subsequent experiences lead children to experience altered self-perceptions, perceptions of the world, and impaired trust in others.36
Individuals with PTSD are also prone to suicidal ideation, suicide attempts, and death by suicide.37 Thus, early identification and treatment of PTSD is a priority for suicide prevention efforts.38 Gradus and colleagues39 studied 163 women with a history of rape and other lifetime traumatic events who received cognitive processing therapy (CPT) or prolonged exposure (PE) for PTSD. Treatment of PTSD was associated with significant reductions in suicidal ideation, with declines that were maintained over 5–10 years.39
Among suicide screening tools, the Columbia-Suicide Severity Rating Scale (C-SSRS) has been used in psychiatric emergency departments around the globe. The C-SSRS has demonstrated predictive value in identifying individuals at heightened suicide risk within 1 week, 1 month, and 1 year following screening.40 Individuals who scored above the cutoff (>3; suicidal thoughts with a method) had roughly 4 times the odds of dying by suicide within 1 week and 1 month and twice the odds of dying within a year of screening.40
How Long Does PTSD Typically Last?
Due to the heterogeneous nature of trauma and its myriad clinical presentations, the duration of PTSD is highly varied. Most individuals who experience a traumatic event do not develop PTSD. Although 70% of people experience a traumatic event in their lifetime, the global lifetime prevalence of PTSD is only 3.9%, while the US lifetime prevalence is estimated at 6.1%.41,42
Approximately half of those who meet criteria for PTSD recover within 3 months.2 PTSD symptoms last for a shorter period (3 years) when treatment (cognitive therapy, exposure therapy, and psychopharmacology) is employed than for those who do not receive care (5 years).43 The American Psychological Association has reported that half of patients recover after 15–20 therapy sessions of trauma-focused psychotherapy. For those with comorbid conditions, the American Psychological Association recommends a longer course of therapy.44 The pace, intensity, and type of trauma-focused psychotherapy (eg, CPT, PE, or eye movement desensitization and reprocessing [EMDR] therapy) are often quite variable and determined by the patient’s symptomatology, preferences, and life stability.44
Sexual assault has been associated with the highest rate of PTSD. Following sexual assault, 75% of survivors meet criteria for PTSD 1 month after the incident. At 3 and 12 months, 54% and 41% meet criteria, respectively.45 These findings point to a potentially critical recovery period during the first 3 months after a trauma, when recovery rates are the highest. Following this period, there is a continued reduction in symptoms, but at a lower rate. However, symptoms can persist throughout an individual’s life.2
Unfortunately, a universal consensus is lacking on the definition of recovery and recurrence of symptoms following recovery. Although tracking symptom severity using standardized scales (eg, the PCL-5) is common, there is little consensus on the duration or level of symptom reduction that is required to label a person as being in recovery or in remission, as research studies have used varied terminology to describe the return of PTSD symptoms after a prior reduction (eg, for relapse, reactivation, and recurrence).46
How Can PTSD Be Treated?
The VA/DoD Clinical Practice Guideline for Management of Posttraumatic Stress Disorder and Acute Stress Disorder (2023) was developed following a systematic review of large clinical and epidemiological databases and includes nonpharmacologic and pharmacologic treatment recommendations for PTSD.47 Individual psychotherapies are strongly recommended over pharmacologic interventions for PTSD.47 For many patients, a combination of psychotherapy and pharmacotherapy is appropriate, as both treatments can be beneficial when used together. While there was previous concern that pharmacotherapy might significantly impair a patient’s ability to engage in and benefit from psychotherapy, current evidence supports the efficacy of combined treatment approaches for PTSD. Individual, manualized trauma-focused psychotherapies for treatment of PTSD include CPT, EMDR, or PE. The VA/DoD clinical practice guideline suggests that the presence of a co-occurring SUD and/or other disorder(s) do not preclude these treatments.
Pharmacologic treatment is not recommended by the National Institutes of Health to prevent PTSD following trauma due to the lack of consistent evidence regarding drug treatments to prevent PTSD.48 Medication or therapy treatment following exposure to trauma is neither recommended for nor against by the VA/DoD guideline for the prevention of PTSD.47 For prevention of PTSD in those diagnosed with ASD, referral to trauma-focused cognitive-behavioral psychotherapy is recommended.47
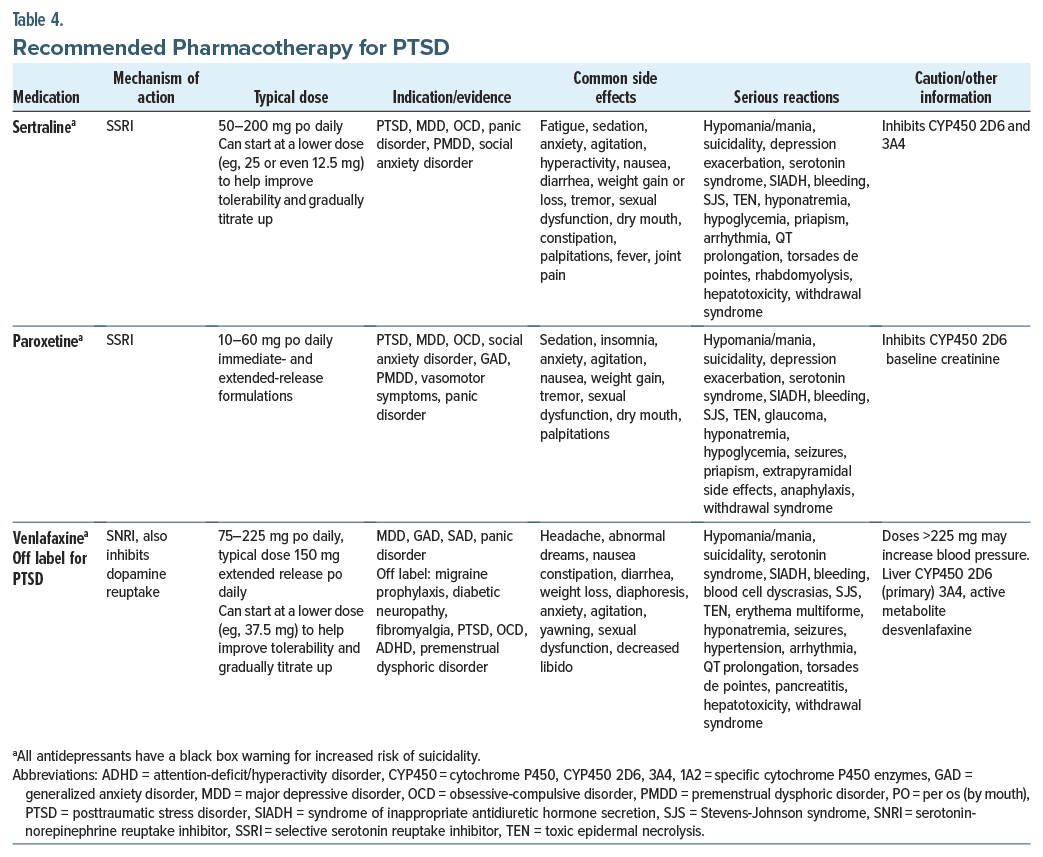
When needed, pharmacologic management of PTSD focuses on the use of serotonergic agents (eg, selective serotonin reuptake inhibitors [SSRIs] such as sertraline and paroxetine and the serotonin-norepinephrine reuptake inhibitor [SNRI] venlafaxine).47 Details regarding these medications (eg, dosing, side effects, relative contraindications) are provided in Table 4. However, additional research into other agents is needed, as there is insufficient evidence for or against the use of alternative SSRIs or SNRIs. However, numerous guidelines recommend the SSRI fluoxetine for the treatment of PTSD.49 When selecting an agent, clinicians should account for the patient’s presentation, their medication history, the drug’s side effect profile, and drug interactions. SSRIs are often the first-line agent given their abundance of safety, tolerability, and efficacy data. If regular adherence to the medication regimen is in question, fluoxetine, given its extended half-life, should be considered. When used in individuals aged 65 years or older, or those with an elevated body mass index, the highly anticholinergic and weight gain–inducing agent paroxetine should be avoided. Venlafaxine, although associated with increases in blood pressure, may be beneficial in those who exhibit predominantly neurovegetative symptoms, given its effects on norepinephrine. Mirtazapine, a tetracyclic antidepressant, can be used for PTSD-related sleep disturbances and comorbid depression symptoms. Prazosin, an antihypertensive medication, can be used to treat PTSD-associated nightmares. While the VA/DoD guideline suggests against prazosin for the treatment of PTSD and states that there is insufficient evidence to recommend for or against mirtazapine, it does suggest prazosin for the treatment of nightmares associated with PTSD.47,50 Although the efficacy of prazosin for nightmares has been questioned, it has demonstrated benefit in service members and veterans.50–52 Service members and veterans with higher sympathetic activation may be more likely to benefit from prazosin.50,52 The antiadrenergic activity of prazosin blunts the persistent nocturnal elevation in noradrenergic activity, which is implicated in trauma-related nightmares and the hyperarousal state of PTSD. The lack of benefit observed in some studies may be due to the lower levels of sympathetic activation in the study population.50 Further supporting this theory, prazosin has been shown to be effective in trauma-associated sleep disorder, a condition characterized by hyperarousal.53
A systematic review and meta-analysis of benzodiazepines for PTSD demonstrated that benzodiazepines are ineffective for PTSD treatment and prevention and that risks associated with their use tend to outweigh short-term benefits.54 Moreover, benzodiazepines are associated with worse PTSD severity, an increased risk of developing PTSD with use after recent trauma, worse psychotherapy outcomes, aggression, depression, and substance use.54
Beta-blockers, particularly propranolol, have been explored as a potential intervention to prevent the progression of acute stress to chronic PTSD by modulating the fear response and memory reconsolidation.55,56 However, their clinical utility remains uncertain, as factors such as lipid solubility, blood-brain barrier penetration, and autonomic regulation complicate their effectiveness. While not a standard treatment, β-blockers may have a role in specific cases with particular symptom clusters, such as hyperarousal or autonomic dysregulation, though further research is needed to determine their long-term benefits.
When Should a Referral for PTSD Treatment Be Obtained and From Whom, Where, and to Whom?
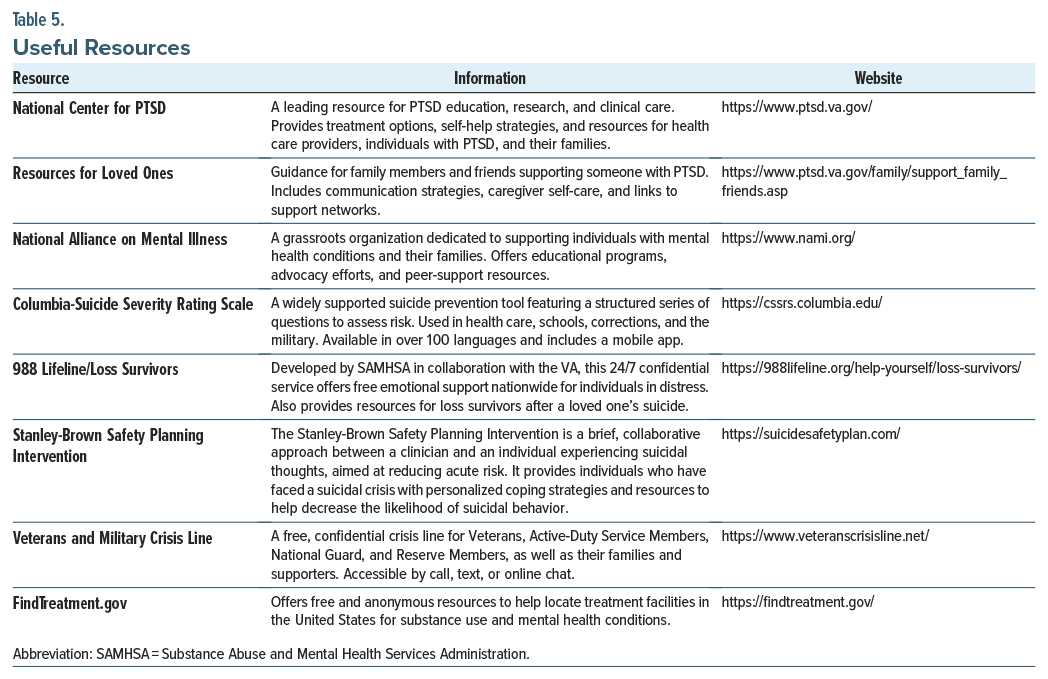
Primary care providers are often the first health care professionals to identify trauma and to diagnose PTSD, making it essential that they know when and to whom referrals should be made (see Table 5: Useful Resources). Clinical practice guidelines recommend referring patients to specialty care, including therapists trained in trauma-informed care who provide manualized, evidence-based treatments (eg, CPT, PE, and EMDR as detailed above), if a first-line therapy service is not available within the primary care setting.47,48,57 For adult patients who have experienced a trauma within the last month but have subdiagnostic symptoms for ASD or PTSD, monitoring is recommended to evaluate if intervention needs develop. For children or patients <18 years old in the same situation, referral for trauma-focused therapy or active monitoring is recommended.48
Since individuals with PTSD are at an elevated risk of suicide, safety evaluations such as suicide risk assessments and determinations of imminent danger are recommended in high-risk cases (as determined by C-SSRS). Primary care providers should refer patients for immediate evaluation in an emergency department if there is concern for acute high suicide risk, inability to maintain safety, or the need for crisis stabilization. If a safety hold or involuntary commitment is necessary, referral to psychiatric crisis services or local emergency psychiatric units should be considered. For those not requiring immediate hospitalization, the Stanley-Brown Safety Planning Intervention can be used as a brief, collaborative approach between a clinician and an at-risk individual to develop personalized coping strategies and crisis resources.
How Prevalent Is PTSD in Health Care Providers?
Rates of PTSD among health care workers vary according to their specialty and work setting. Stressors identified in a study of health care worker–related PTSD included treating trauma patients, working in conflict zones, experiencing residency training stress, and practicing medicine in rural areas.58 Events reported by nurses who were diagnosed with PTSD included caring for those with massive bleeding, trauma-related injuries, as well as witnessing a patient’s death and delivering futile care to terminally or critically ill patients.59
A 2024 systematic review and meta-analysis on PTSD in physicians during the COVID-19 pandemic reported that specialties with the highest prevalence of PTSD symptoms were family medicine and emergency medicine.60 They estimated that the pooled prevalence of PTSD across all specialties was 18.3%, with different rates for different disciplines: critical care (14.8%), trauma surgery (15%), anesthesiology (16.1%), internal medicine (21.9%), otolaryngology (23.0%), emergency medicine (23.4%), and family medicine (31.4%).60 The rates of PTSD for nurses in a survey study was 18%.59
The prevalence of PTSD was higher in trainees than in attending physicians (31% vs 24.7%).60 Rates of PTSD were also found to increase in ICU health care professions during the COVID-19 pandemic when compared to those prepandemic (prevalence of 3%–24% increased to 16%–73%).61 Female physicians experienced higher rates of PTSD, similar to that found in the general population, where females have around twice the lifetime prevalence compared to men.60 Military health care workers have similar rates of PTSD when compared to combat-exposed military personnel, with estimates of up to 20%.62
What Happened to Mr A?
Mr A’s presentation included symptoms of ASD following his traumatic incident, which was less than 1 month prior. His anxiety, nightmares, insomnia, and difficulty processing the trauma suggested that he was struggling to adapt to the psychological impacts of the accident. He was reassured by learning that some of his distress was a normal response to trauma. With further evaluation and interventions to address his anxiety and provide him with psychological support, he gradually improved. He was started on sertraline for anxiety that was titrated up to 100 mg daily and referred to individual psychotherapy with a therapist trained in CPT. However, he showed greater improvement with supportive therapy and weekly sessions with his therapist. To address nightmares and insomnia, prazosin was initiated and titrated to 5 mg at bedtime leading to symptom relief. His comorbid pain symptoms were treated with gabapentin 600 mg 3 times daily, resulting in a positive response. The team utilized a combination of pharmacologic pain management and therapeutic approaches to support his physical recovery and emotional and psychological adjustment following the trauma.
CONCLUSIONS
Since symptoms overlap between several anxiety disorders and PTSD, diagnostic precision and subsequent treatment may be compromised. Individuals with GAD have anxiety in a wide range of circumstances, whereas those with PTSD often experience anxiety in response to a major trauma. Individuals with depression may feel hopelessness, intense shame, or guilt, while those with panic disorder experience intense anxiety, which can be related to a specific object or situation.
Individuals with PTSD are much more likely than those without PTSD to have at least 1 other psychiatric condition (eg, MDD, AUD, and other anxiety disorders), and they are also prone to develop physical health problems (including bone and joint disease, metabolic diseases, neurological conditions, respiratory conditions, and cardiovascular conditions).
Pretraumatic risk factors for PTSD include early childhood emotional problems and prior mental disorders, while environmental factors (eg, lower socioeconomic status, lower education, prior trauma exposure or adversity, lower intelligence, minoritized racial/ethnic status, and family psychiatric history), genetic and physiological factors (eg, female gender and younger age at time of trauma exposure), and peri-traumatic environmental risk factors (eg, the severity/ dose of trauma, the perception of life threat, interpersonal violence, and personal injury) have also been linked with developing PTSD, while posttraumatic risk factors (eg, negative appraisals and limited coping skills and repeated upsetting reminders and subsequent adverse life events) complicate its treatment.
Unfortunately, health care workers also suffer from PTSD. In fact, military health care workers have similar rates of PTSD to combat-exposed military personnel, with estimates as high as 20%. Since individuals with PTSD are at an elevated risk of suicide, safety evaluations and timely treatment are recommended.
Article Information
Published Online: August 5, 2025. https://doi.org/10.4088/PCC.24f03899
© 2025 Physicians Postgraduate Press, Inc.
Submitted: December 5, 2024; accepted April 1, 2025.
To Cite: Matta SE, Rustad JK, Fisher DR, et al. Assessment and management of posttraumatic stress disorder in primary care practices. Prim Care Companion CNS Disord 2025;27(4):24f03899.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts (Matta, Stern); Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire (Rustad); Larner College of Medicine at University of Vermont, Burlington, Vermont (Rustad); Burlington Lakeside VA Community Based Outpatient Clinic, Burlington, Vermont (Rustad); White River Junction VA Medical Center, White River Junction, Vermont (Rustad); Department of Psychiatry, Wright State University Boonshoft School of Medicine and Wright-Patterson Medical Center in Dayton, Ohio (Fisher); Department of Psychiatry, Lewis Gale Medical Center, Salem, Virginia (Braford).
Corresponding Author: Sofia E. Matta, MD, Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School, 55 Fruit St, Boston, MA 02114 ([email protected]).
Relevant Financial Relationships: Dr Matta has no disclosures or conflicts of interest. Dr Rustad is employed by the US Department of Veterans Affairs, but the opinions expressed in this presentation do not reflect those of the Department of Veterans Affairs. Dr Fisher is employed by the US Department of Defense and is an officer in the US Air Force; this presentation does not reflect those of the Department of Defense or the US Air Force. Dr Braford has no disclosures or conflicts of interest, but the opinions expressed in this presentation do not reflect those of Lewis Gale Medical Center. Dr Stern has received royalties from Elsevier for editing textbooks on psychiatry.
Funding/Support: None.
Clinical Points
- Posttraumatic stress disorder (PTSD) can be diagnosed by its 4 symptom clusters: intrusions, avoidance, impaired cognition and mood, and alterations in arousal and reactivity, facilitated by use of a validated structured clinician-administered interview.
- PTSD diagnosis can be confounded by comorbid conditions such as generalized anxiety disorder, major depressive disorder, alcohol use disorder, and other psychiatric or medical conditions, including insomnia, obstructive sleep apnea, cardiovascular disease, and metabolic disorders.
- PTSD and mild traumatic brain injury are both common and commonly co-occur; they have occurred in nearly half of US military personnel and deployed combat veterans (in the Iraq/Afghanistan wars).
- Screening and timely treatment are lifesaving for individuals with PTSD, who are at increased risk for suicidal ideation, suicide attempts, and death by suicide.
- The VA/DoD Clinical Practice Guidelines strongly recommend individual psychotherapies over pharmacologic interventions (eg, cognitive processing therapy, prolonged exposure, or eye movement desensitization and reprocessing).
References (62)

- Goldstein RB, Smith SM, Chou SP, et al. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National Epidemiologic Survey on alcohol and related conditions-III. Soc Psychiatry Psychiatr Epidemiol. 2016;51(8):1137–1148. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Text Revision. American Psychiatric Association; 2022:271–286. https://doi.org/10.1176/appi.books.9780890425787
- Khouzam HR. A simple mnemonic for the diagnostic criteria for post-traumatic stress disorder. West J Med. 2001;174(6):424. PubMed CrossRef
- Prins A, Bovin MJ, Kimerling R, et al. Primary care PTSD screen for DSM-5 (PC-PTSD-5) [Measurement instrument]. 2015. Accessed 23 11, 2024. https://www.ptsd.va.gov/professional/assessment/screens/pc-ptsd.asp
- Bovin MJ, Kimerling R, Weathers FW, et al. Diagnostic accuracy and acceptability of the primary care posttraumatic stress disorder screen for the diagnostic and Statistical manual of mental disorders (Fifth edition) among US veterans. JAMA Netw Open. 2021;4(2):e2036733. PubMed CrossRef
- Prins A, Bovin MJ, Smolenski DJ, et al. The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. 2016;31(10):1206–1211. Epub 20160511. PubMed CrossRef
- Weathers FW, Litz BT, Keane TM, et al. The PTSD Checklist for DSM-5 (PCL-5). 2013. Accessed 23 11, 2024. www.ptsd.va.gov
- Jackson CE, Currao A, Fonda JR, et al. Research utility of a CAPS-IV and CAPS-5 hybrid interview: posttraumatic stress symptom and diagnostic concordance in recent-era U.S. veterans. J Trauma Stress. 2022;35(2):570–580. PubMed CrossRef
- Weathers FW, Blake DD, Schnurr PP, et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). 2013. Accessed 23 11, 2024. https://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp#obtain
- Lee DJ, Weathers FW, Thompson-Hollands J, et al. Concordance in PTSD symptom change between DSM-5 versions of the Clinician-Administered PTSD Scale (CAPS-5) and PTSD Checklist (PCL-5). Psychol Assess. 2022;34(6):604–609. PubMed CrossRef
- Marx BP, Lee DJ, Norman SB, et al. Reliable and clinically significant change in the clinician-administered PTSD Scale for DSM-5 and PTSD Checklist for DSM-5 among male veterans. Psychol Assess. 2022;34(2):197–203. PubMed CrossRef
- Anxiety Disorders in Adults. Screening in Final Recommendation Statement. U.S. Preventive Services Task Force; 2023. Accessed August 03, 2025. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/anxiety-adults-screening
- Rytwinski NK, Scur MD, Feeny NC, et al. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress. 2013;26(3):299–309. PubMed CrossRef
- Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatry. 2014;59(9):460–467. PubMed CrossRef
- Milanak ME, Gros DF, Magruder KM, et al. Prevalence and features of generalized anxiety disorder in Department of Veteran Affairs primary care settings. Psychiatry Res. 2013;209(2):173–179. PubMed CrossRef
- Brady KT, Killeen TK, Brewerton T, et al. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psych. 2000;61(suppl 7):22–32. PubMed
- Brassil HE, Salvatore AP. The frequency of posttraumatic stress disorder symptoms in athletes with and without sports related concussion. Clin Transl Med. 2018;7(1):25. PubMed CrossRef
- Miller SC, Whitehead CR, Otte CN, et al. Risk for broad-spectrum neuropsychiatric disorders after mild traumatic brain injury in a cohort of US Air Force personnel. Occup Environ Med. 2015;72(8):560–566. PubMed CrossRef
- Stein MB, Kessler RC, Heeringa SG, et al. Prospective longitudinal evaluation of the effect of deployment-acquired traumatic brain injury on posttraumatic stress and related disorders: results from the Army Study to Assess Risk and Resilience in Service members (Army STARRS). Am J Psychiatry. 2015;172(11):1101–1111. PubMed CrossRef
- Hoge CW, McGurk D, Thomas JL, et al. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. NEJM. 2008;358(5):453–463. PubMed CrossRef
- “Do I Have PTSD or Something Else?”. 2024. https://psychcentral.com/ptsd/differential-diagnosis-of-ptsd-symptoms
- Sherin JE, Nemeroff CB. Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues Clin Neurosci. 2011;13(3):263–278. PubMed CrossRef
- Ressler KJ, Berretta S, Bolshakov VY, et al. Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nat Rev Neurol. 2022;18(5):273–288. PubMed CrossRef
- Friedman MJ, McEwen BS. Posttraumatic stress disorder, allostatic load, and medical illness. In: Schnurr PP, Green BL, eds. Trauma and Health: Physical Health Consequences of Exposure to Extreme Stress. American Psychological Association; 2004:157–188. CrossRef
- Edmondson D, von Känel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4:320–329. PubMed CrossRef
- Marchi M, Travascio A, Uberti D, et al. Post-traumatic stress disorder among LGBTQ PEOPLE: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. 2023;32:e44. PubMed CrossRef
- Spoont M, McClendon J. Racial and ethnic disparities in PTSD. PTSD Res Q. 2020;31(4).
- Harb F, Bird CM, Webb EK, et al. Experiencing racial discrimination increases vulnerability to PTSD after trauma via peritraumatic dissociation. Eur J Psychotraumatol. 2023;14(2):2211486. PubMed CrossRef
- Roberts AL, Gilman SE, Breslau J, et al. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41(1):71–83. PubMed CrossRef
- Tabb LP, Rich JA, Waite D, et al. Examining associations between adverse childhood experiences and posttraumatic stress disorder symptoms among young survivors of urban violence. J Urban Health. 2022;99(4):669–679. PubMed CrossRef
- McCabe SE, Hughes TL, West BT, et al. Sexual orientation, adverse childhood experiences, and comorbid DSM-5 substance use and mental health disorders. J Clin Psychiatry. 2020;81(6):20m13291. PubMed CrossRef
- Zhang X, Monnat SM. Racial/ethnic differences in clusters of adverse childhood experiences and associations with adolescent mental health. SSM Popul Health. 2022;17:100997. PubMed CrossRef
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults – the adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258. PubMed CrossRef
- Guina J, Nahhas RW, Sutton P, et al. The influence of trauma type and timing on PTSD symptoms. J Nerv Ment Dis. 2018;206(1):72–76. PubMed CrossRef
- Ryder AL, Azcarate PM, Cohen BE. PTSD and physical health. Curr Psychiatry Rep. 2018;20(12):116. PubMed CrossRef
- Dye H.. The impact and long-term effects of childhood trauma. J Hum Behav Soc Envir. 2018;28(3):381–392. CrossRef
- Stanley IH. Advancements in the understanding of PTSD and suicide risk: Introduction to a special section. Psychol Trauma. 2021;13(7):723–724. PubMed CrossRef
- Akbar R, Arya V, Conroy E, et al. Posttraumatic stress disorder and risk of suicidal behavior: a systematic review and meta-analysis. Suicide Life Threat Behav. 2023;53(1):163–184. PubMed CrossRef
- Gradus JL, Suvak MK, Wisco BE, et al. Treatment of posttraumatic stress disorder reduces suicidal ideation. Depress Anxiety. 2013;30(10):1046–1053. PubMed CrossRef
- Bjureberg J, Dahlin M, Carlborg A, et al. Columbia-Suicide Severity Rating Scale screen version: Initial screening for suicide risk in a psychiatric emergency department. Psychol Med. 2022;52(16):3904–3912. CrossRef
- Koenen KC, Ratanatharathorn A, Ng L, et al. Posttraumatic stress disorder in the world mental health Surveys. Psychol Med. 2017;47(13):2260–2274. PubMed CrossRef
- Goldstein RB, Smith SM, Chou SP, et al. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National epidemiologic Survey on alcohol and related conditions-III. Soc Psychiatry Psychiatr Epidemiol. 2016;51(8):1137–1148. PubMed CrossRef
- Grinage BD. Diagnosis and management of post-traumatic stress disorder. Am Fam Physician. 2003;68(12):2401–2408. PubMed
- American Psychological Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. American Psychological Association; 2017. Accessed November 20, 2024. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Dworkin ER, Jaffe AE, Bedard-Gilligan M, et al. PTSD in the year following sexual assault: a meta-analysis of prospective studies. Trauma Violence Abuse. 2023;24(2):497–514. PubMed CrossRef
- Brooks SK, Greenberg N. Recurrence of post-traumatic stress disorder: systematic review of definitions, prevalence and predictors. BMC Psychiatry. 2024;24(1):37. PubMed CrossRef
- VA/DoD Clinical Practice Guideline for Management of Posttraumatic Stress Disorder and Acute Stress Disorder. US Gov Pr Office; 2023. Accessed November 23, 2024. https://www.healthquality.va.gov/guidelines/MH/ptsd/VA-DoD-CPGPTSD-Full-CPG-Edited-11162024.pdf
- National Institute for Health and Care Excellence (NICE). Post-Traumatic Stress Disorder: Management. NICE Guideline [NG116]; 2018. Accessed November 22, 2024. https://www.nice.org.uk/guidance/ng116
- Martin A, Naunton M, Kosari S, et al. Treatment guidelines for PTSD: a systematic review. J Clin Med. 2021;10(18):4175. PubMed CrossRef
- Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507–517. PubMed CrossRef
- Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160(2):371–373. PubMed CrossRef
- Raskind MA, Millard SP, Petrie EC, et al. Higher pretreatment blood pressure is associated with greater posttraumatic stress disorder symptom reduction in soldiers treated with prazosin. Biol Psychiatry. 2016;80(10):736–742. PubMed CrossRef
- Brock MS, Powell TA, Creamer JL, et al. Trauma associated sleep disorder: clinical developments 5 years after discovery. Curr Psychiatry Rep. 2019;21(9):80. PubMed CrossRef
- Guina J, Rossetter SR, DeRhodes BJ, et al. Benzodiazepines for PTSD: a systematic review and meta-analysis. J Psychiatr Pract. 2015;21(4):281–303. PubMed CrossRef
- Roque AP. Pharmacotherapy as prophylactic treatment of post-traumatic stress disorder: a review of the literature. Issues Ment Health Nurs. 2015;36(9):740–751. PubMed CrossRef
- Mallet C, Chick CF, Maatoug R, et al. Memory reconsolidation impairment using the β-adrenergic receptor blocker propranolol reduces nightmare severity in patients with posttraumatic stress disorder: a preliminary study. J Clin Sleep Med. 2022;18(7):1847–1855. PubMed CrossRef
- Ursano RJ, Bell C, Eth S, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry. 2004;161(11 suppl):3–31. PubMed
- Sendler J, Rutkowska A, Makara-Studzinska M. How the exposure to trauma has hindered physicians’ capacity to heal: prevalence of PTSD among healthcare workers. Eur J Psychiatry. 2016;30:321–334.
- Mealer M, Burnham EL, Goode CJ, et al. The prevalence and impact of posttraumatic stress disorder and burnout syndrome in nurses. Depress Anxiety. 2009;26(12):1118–1126. PubMed CrossRef
- Kamra M, Dhaliwal S, Li W, et al. Physician posttraumatic stress disorder during COVID-19: a systematic review and meta-analysis. JAMA Netw Open. 2024;7(7):e2423316. PubMed CrossRef
- Deltour V, Poujol AL, Laurent A. Post-traumatic stress disorder among ICU healthcare professionals before and after the COVID-19 health crisis: a narrative review. Ann Intensive Care. 2023;13(1):66. PubMed CrossRef
- Nash WP, Silva C, Litz BT. The historic origins of military and veteran mental health stigma and the stress injury model as a means to reduce it. Psychiatr Ann. 2009;39(8):789–794. CrossRef
This PDF is free for all visitors!