Turner syndrome (TS) is a genetic disorder affecting 1 in 2,500 live female births, marked by the partial or complete absence of one X chromosome.1 This anomaly leads to physical and neuropsychiatric challenges, including cardiovascular issues, short stature, infertility, and intellectual disabilities.2 Individuals with TS also commonly experience psychiatric conditions such as anxiety, depression, and psychosis.3 These conditions significantly impact daily life, requiring a combination of pharmacologic and therapeutic interventions.4
Auditory hallucinations, a common psychotic symptom, have been noted in TS patients.5 While antipsychotics are typically used to treat psychiatric symptoms, refractory cases may require alternative treatments.6 This report explores the use of electroconvulsive therapy (ECT) for refractory auditory hallucinations in a young TS patient, where conventional treatments were ineffective. This case underscores the potential role of ECT in managing psychosis and hallucinations in TS when pharmacologic options fail, marking the first known use of ECT for this purpose in TS.
Case Report
A 19-year-old female with TS, schizophrenia, and major depressive disorder presented for an ECT evaluation after multiple pharmacologic treatments failed to control her refractory auditory hallucinations, which had persisted for approximately 4 years. Her psychiatric history included recurrent emergency department visits for hallucinations and distressing behaviors, such as public undressing. Despite high-doses of risperidone (up to 14 mg) and later aripiprazole (20 mg), the patient continued to experience persistent hallucinations, particularly derogatory voices.
The patient fulfilled DSM-5 diagnostic criteria for schizophrenia, exhibiting persistent auditory hallucinations and disorganized behavior for over 6 months.7 Despite trials of multiple antipsychotic medications, including a therapeutic course of clozapine at an adequate dose (up to 300 mg daily) for 12 weeks, the patient continued to experience significant psychotic symptoms. These findings led to the classification of clozapine-resistant schizophrenia and justified the initiation of ECT as an adjunctive treatment.
The patient was evaluated for ECT on January 30, 2024 (all dates have been de-identified to protect patient anonymity), and after a thorough discussion of risks and benefits, including the absence of known evidence supporting ECT in TS, the decision was made to proceed. ECT was administered using a Thymatron System IV device. Initial treatments employed bilateral electrode placement with stimulus dosing titrated to induce adequate seizures, which typically lasted between 70 and 90 seconds as monitored by electroencephalogram (EEG). Treatments were delivered 2 times weekly during the first 8 weeks, once weekly for approximately 8 months, and then tapered to twice monthly maintenance sessions based on clinical response. Adjustments to stimulus intensity and frequency were made individually to optimize efficacy while minimizing cognitive side effects.
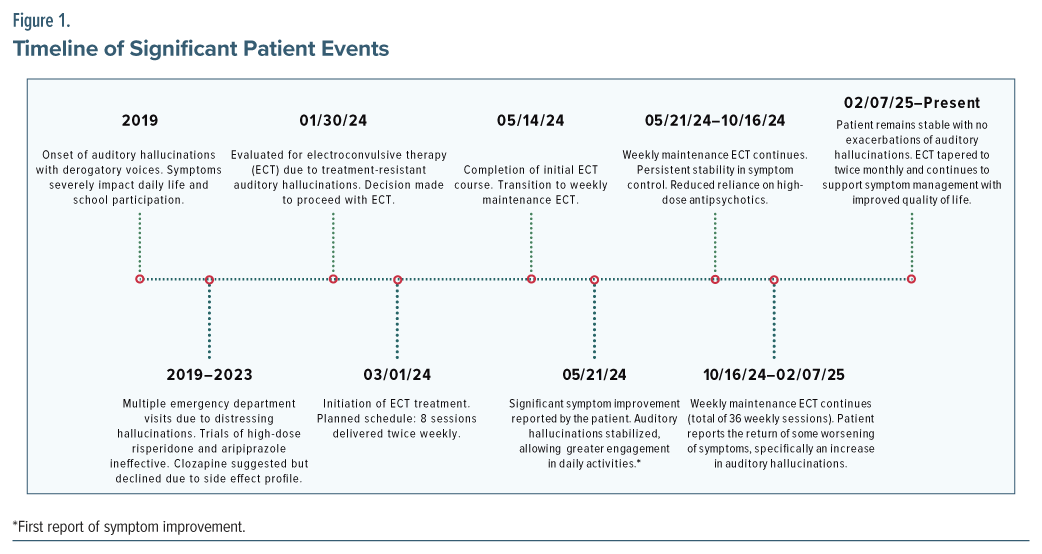
ECT treatment began on March 1, 2024, with 8 sessions planned twice weekly. Treatment continued through May 14, 2024, and was then tapered to weekly maintenance. By May 21, 2024, the patient reported significant improvement in her symptoms and improved daily functioning. According to the patient, ECT contributed to a reduction in symptom severity, with intermittent periods of complete remission or only minimal hallucinations. However, between October 16, 2024, and January 3, 2025, the patient reported some worsening symptoms, specifically an increase in auditory hallucinations, before stabilizing again. The patient continued weekly ECT treatments through this time, and by February 7, 2025, she was still experiencing stable symptom control.
As of the most recent follow-up in February 2025, the patient has begun receiving twice-monthly ECT treatments and has maintained symptom stability with no further exacerbations of auditory hallucinations. The ECT treatment has resulted in reduced reliance on highdose antipsychotic medications, which was a primary goal of the therapy. Of note, the patient’s clozapine was tapered from 300 mg to 50 mg progressively over the initial 36 ECT sessions, and her aripiprazole was tapered from 20 mg to 10 mg after 24 ECT sessions. These medication adjustments aimed to decrease potential side effects and reliance on high-dose antipsychotics while preserving clinical stability alongside ongoing ECT therapy.
According to the patient, the most notable improvement has been the absence of responses to internal stimuli, marking a significant breakthrough. Additionally, when ECT had an EEG duration above 70 seconds, the patient’s auditory hallucinations ceased completely. When the EEG duration was below 70 seconds, hallucinations remained stabilized, with a significant reduction in both frequency and severity, decreasing from multiple daily occurrences to only a few times per week (Figure 1).
Discussion
ECT induces therapeutic seizures, with the electroencephalographic characteristics of these seizures varying between patients. Although the patient in this case benefited from seizure durations exceeding 70 seconds, there is no current evidence that suggests that longer EEG seizure durations, particularly those exceeding 70 seconds, have been associated with more significant reductions in auditory hallucinations when compared to shorter durations.8
The use of ECT in TS patients with psychosis and auditory hallucinations is undocumented to date. TS is associated with unique medical considerations, including cardiovascular issues (eg, aortic coarctation), hormonal imbalances, and intellectual disabilities, which must be carefully evaluated when considering psychiatric interventions such as ECT.[2]
Antipsychotic medications are the standard treatment for psychosis in TS patients. However, as demonstrated in this case, they may be ineffective, particularly in instances of treatmentresistant hallucinations.6 Additionally, certain medications like risperidone can cause extrapyramidal symptoms, which can significantly complicate treatment options.9 While ECT is well-established as an effective treatment for severe mood disorders, especially depression, its use in treating psychosis in TS patients remains rare.10
While routine pre-ECT evaluations include a clinical history and physical examination, additional testing is guided by patient-specific factors. One critical consideration when administering ECT to TS patients is their underlying medical conditions, especially potential cardiovascular abnormalities.11 In this case, an echocardiogram was performed because the patient has TS, a condition associated with potential cardiac abnormalities such as bicuspid aortic valve and coarctation of the aorta.11 This evaluation was necessary to assess cardiac risk prior to initiating ECT, despite echocardiograms not being a standard part of pre-ECT workup. In this case, the patient’s normal electrocardiogram and echocardiogram indicated no immediate safety concerns regarding the procedure.
Conclusion
To our knowledge, this is the first case that demonstrates the potential of ECT for treating refractory auditory hallucinations in TS. When psychotic symptoms fail to respond to medication, ECT may be a viable alternative. Further research is needed to establish its long-term safety and efficacy in this unique population. Clinicians should consider ECT alongside other treatment options for managing refractory psychiatric symptoms in TS.
Article Information
Published Online: September 23, 2025. https://doi.org/10.4088/PCC.25cr03986
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(5):25cr03986
Submitted: April 18, 2025; accepted June 12, 2025.
To Cite: McDuffee NS, Forster AA, Shah K. Electroconvulsive therapy for refractory auditory hallucinations in Turner syndrome. Prim Care Companion CNS Disord 2025;27(5):25cr03986.
Author Affiliations: Wake Forest School of Medicine, Winston-Salem, North Carolina (McDuffee, Forster); Atrium Health Wake Forest Baptist, Winston-Salem, North Carolina (Shah).
Corresponding Author: Nicholas S. McDuffee, MA, BS, Atrium Health Wake Forest Baptist, Department of Psychiatry, Wake Forest School of Medicine, 1 Medical Center Blvd, Winston-Salem, North Carolina 27157 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information, including dates, has been de-identified to protect anonymity.
References (11)

- Nielsen J, Wohlert M. Chromosome abnormalities found among 34,910 newborn children: results from a 13-year incidence study in Arhus, Denmark. Hum Genet. 1991;87(1):81–83. PubMed CrossRef
- Gupta M, Zubiar F, Gupta N. Turner syndrome and the risks of clinical depression in adolescence. Cureus. 2021;13(11):e19204. PubMed CrossRef
- Ygland Rödström M, Johansson BA, Bäckström B, et al. Acute mania and matatonia in a teenager successfully treated with electroconvulsive therapy and diagnosed with Turner syndrome and bipolar disorder. Case Rep Psychiatry. 2021;2021:3371591. PubMed
- Björlin Avdic H, Butwicka A, Nordenström A, et al. Neurodevelopmental and psychiatric disorders in females with Turner syndrome: a population-based study. J Neurodev Disord. 2021;13(1):51. PubMed CrossRef
- Catinari S, Vass A, Heresco-Levy U. Psychiatric manifestations in Turner syndrome: a brief survey. Isr J Psychiatry Relat Sci. 2006;43(4):293–295. PubMed
- Xia Y, Sun Y, Zhi Q, et al. A case report of a patient with Turner syndrome who develops catatonia secondary to psychotic symptoms. Med Baltim. 2024;103(14):e37730. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Sinclair DJ, Zhao S, Qi F, et al. Electroconvulsive therapy for treatment-resistant schizophrenia. Cochrane Database Syst Rev. 2019;3(3):CD011847. PubMed CrossRef
- Ostinelli EG, Hussein M, Ahmed U, et al. Risperidone for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2018;4(4):CD009412. PubMed CrossRef
- Rojas M, Ariza D, Ortega Á, et al. Electroconvulsive therapy in psychiatric disorders: a narrative review exploring neuroendocrine-immune therapeutic mechanisms and clinical implications. Int J Mol Sci. 2022;23(13):6918. PubMed CrossRef
- Silberbach M, Roos-Hesselink JW, Andersen NH, et al. Cardiovascular health in Turner syndrome: a scientific statement from the American Heart Association. Circ Genom Precis Med. 2018;11(10):e000048. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!