Abstract
Objective: To investigate the impact of various exercise modalities on the mitigation of pain catastrophizing in patients with fibromyalgia.
Data Sources: A systematic review with comparative analysis was conducted on May 22, 2024, utilizing Embase, PubMed, Scopus, Cochrane Library, and Web of Science.
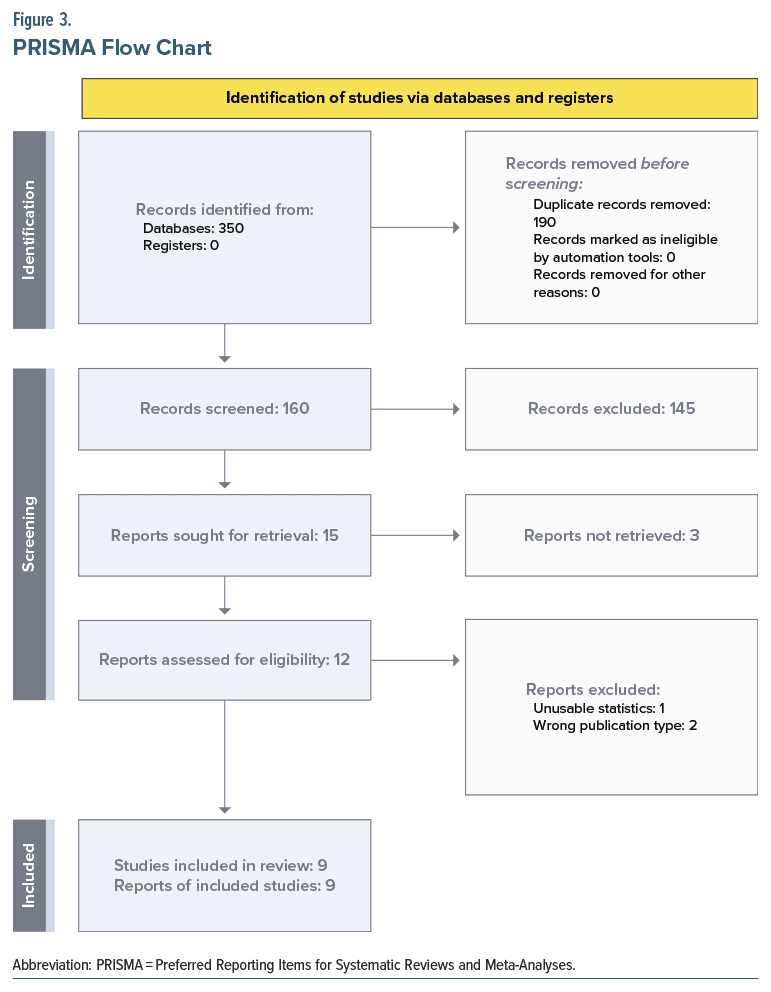
Study Selection: The search resulted in 350 articles, of which 190 were duplicates. After duplicate removal, title and abstract appraisal was conducted followed by full-text appraisal. A total of 9 articles fit the inclusion/exclusion criteria.
Data Extraction: Usable statistics and relevant data points were extracted. Outcomes of interest were pain catastrophizing scores. The duration of treatment protocol and the number of exercise sessions per week were also extracted.
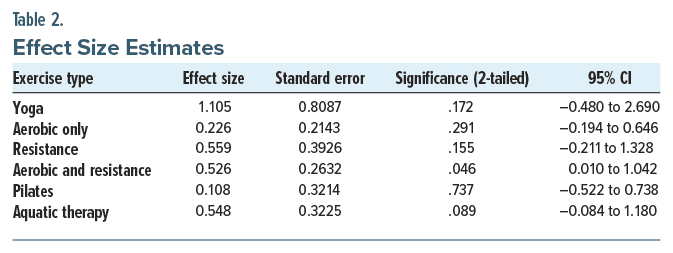
Results: Exercise intervention of any type showed a moderate impact on pain catastrophizing (d =0.58; 95% CI, 0.16–1.01; P < .01). Subgroup analysis showed varying effects. Yoga was not statistically significant but was the most clinically effective (d = 1.1; 95% CI, −0.48 to 2.69; P = .172). Pilates did not clinically or statistically reduce pain catastrophizing (d = 0.108; 95% CI, −0.522 to 0.738; P = .737). Resistance training, mixed aerobic-resistance exercise, aquatic therapy/exercise, and aerobic only all denoted a degree of clinically significant effectiveness (d = 0.559, 0.526, 0.548, and 0.226, respectively). Only mixed aerobic resistance training was significant (P = .046).
Conclusions: Exercise in general is a moderately effective treatment option to mitigate pain catastrophizing, although various treatment modalities may prove more practical than others due to their nature. High-effort, high intensity modalities may be less effective (Pilates) as lower-intensity modalities (aquatic therapy). Yoga, having the highest effect size, was the only modality which focuses on physical exercise as well as meditation and spirituality. More randomized trials are needed to further clarify the importance of mindfulness, spirituality, and meditation in combination with physical exercise for fibromyalgia patients who catastrophize.
Prim Care Companion CNS Disord 2025;27(2):24r03817
Author affiliations are listed at the end of this article.
Fibromyalgia is a debilitating pathology characterized by widespread musculoskeletal pain, which has no identifiable cause and is not due to inflammation.1 Making a diagnosis of fibromyalgia is challenging due to the lack of an identifiable source on imaging, histology, or physical exam. The American College of Rheumatology classifies fibromyalgia diagnosis by a patient having no other identifiable disorder to cause pain, pain symptoms for at least 3 months, and a Widespread Pain Index (WPI) ≥7 with a Symptom Severity (SS) score ≥5 or a WPI ranging from 3 to 6 and SS ≥9.2 Although there is no current identifiable cause, the discomfort experienced from fibromyalgia is often exacerbated by physical and psychological stressors.3 Due to the difficulties posed by this pathology, patients often utilize health care resources more than patients without fibromyalgia, leading to significant medical costs to both patients and health care systems.4 In addition to pain and pain dysregulation, patients suffering from fibromyalgia often experience muscle and joint stiffness, sleep disturbances, and cognitive and psychiatric ailments, leading to significant decreases in quality of life.5 Fibromyalgia has a higher propensity to affect females, with a potential genetic component leading to familial patterns of disease development.6
The treatment of fibromyalgia can prove to be clinically challenging due to the varying presentations of the disease. First-line management involves lifestyle modifications such as improving sleep, increasing exercise, and engaging in cognitive-behavioral therapy.7 Pharmacologic management is typically with selective serotonin reuptake inhibitors or serotonin-norepinephrine inhibitors such as duloxetine. Other options included in management are pregabalin for severe pain or tricyclic antidepressants such as amitriptyline for sleep disturbances.8
An interesting phenomenon exacerbated by fibromyalgia is pain catastrophizing. Pain catastrophizing has been defined as the tendency to hyperfixate on the pain, exaggerate the magnitude, and perceive the pain as uncontrollable.9 Increased pain catastrophizing has been associated with increased distress, decreased quality of life, and pain induced disability in patients suffering from fibromyalgia.10 Some aspects of this condition include excessive rumination over pain, inability to perform daily functions such as movement, and feelings of overwhelming helplessness.11 As a result of pain catastrophizing, there is increased avoidance of painful or noxious stimuli; patients afflicted with fibromyalgia often become more sedentary and avoid exercise, as it is believed to cause their pain to be worsened.12
Exercise is one of the first management options prescribed for patients suffering from fibromyalgia. Exercise also combats chronic depression and improves sleep, making it an excellent option for treating fibromyalgia-related conditions.13 Some of the proposed mechanisms by which exercise improves pain in fibromyalgia patients are increased endogenous opioid, growth hormone, and corticotropin production; reduced sympathetic nervous system activity; downregulation of proinflammatory cytokines; and improvement of muscle oxygenation.14 However, patients are often met with a dilemma when they are unable to exercise or become more active due to their heightened sense of pain catastrophizing.
As such, it is imperative to discern a means of helping patients cope with and decrease the level of catastrophizing so that patients may exercise. This systematic review and comparative analysis investigates various types of exercise therapies and their potential impact on fibromyalgia patients with elevations in their pain catastrophizing.
METHODS
An exhaustive systematic review, using Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) 2020 guidelines, of 5 medical databases was conducted to investigate the potential effects of various exercise types on pain catastrophizing in fibromyalgia patients.15 The systematic review was registered and published online ahead of manuscript completion through PROSPERO (registration reference: CRD42024545889).
Inclusion Criteria
For an article to be considered for inclusion, it had to (1) be a randomized controlled trial (RCT), single-arm study, case series, or any form of retrospective study; (2) contain primary clinical data (those with secondary clinical data were excluded); (3) contain patients who are officially diagnosed with fibromyalgia; (4) contain an exercise intervention arm; and (5) have usable pre- and postintervention statistics (if statistical reporting is not compatible with meta-analytics or pooling is excluded). “Grey” literature could be included so long as it met the above criteria. Outcomes of interest were the degree of pain catastrophizing before and after exercise intervention, the type of exercise intervention, and the patient demographics.
Exclusion Criteria
Studies were excluded if they were case reports, posters, or abstracts on single patients (due to their lack of standard deviation, causing difficulty for statistical analysis) or if the statistics were not compatible with meta-analysis or pooling. If improper reporting of baseline or postintervention statistics were found within an article of interest, the corresponding author was contacted, and a month was given for response before the article was excluded. Articles were not excluded based on language of origin, date of origin, or country of origin. If an article did not have full text available after exhaustive searching, interlibrary loaning, or contacting the corresponding author, it was then excluded. Studies were excluded if they did not include a measure or metric on pain catastrophizing. Articles were also excluded if they did not have an exercise-only intervention arm. Due to the nature of fibromyalgia treatments, studies with patients on concomitant medications for their illness were not excluded.
Information Sources and Search Strategy
Initial querying of the 5 databases was conducted on May 22, 2024. The databases employed were Embase, PubMed, Scopus, Cochrane Library, and Web of Science. The search string used in these databases was first developed utilizing Medical Subject Headings (MeSH) terms and then by adding Boolean operators and terms and variables of interest often associated with the topic of interest but not located in MeSH. The string was as follows: (“fibromyalgia” OR “fibromyalgias” OR “fibrositis” OR “fibrositides” OR “muscular rheumatism”) AND (“exercise” OR “physical activity” OR “physical exercise” OR “exercise training” OR “exercise trainings” OR “physical fitness”) AND (“pain catastrophizing” OR “pain-related cognitive rumination” OR “pain catastrophizings”). To ensure all relevant articles were retrieved for analysis, a manual appraisal of article references and cited-by sections was conducted.
Duplicates were detected with Rayyan.ai and subsequently deleted. Manual duplicate checking by 2 independent reviewers was then conducted to ensure no articles were missed by the program.
Study Selection
After article retrieval and subsequent screening for duplicates, articles were then screened for inclusion criteria based on their titles and abstracts by 2 independent reviewers (B.G. and N.E.) with a third (M.G.) being brought in to break ties. Following title and abstract appraisal, articles then had their full text reviewed for relevance and inclusion/ exclusion criteria. Following this extensive review process, for articles deemed to fit all inclusion criteria and contain relevant statistics, data extraction was conducted.
Data Collection
Articles that contained usable statistics and relevant data points had the information extracted and placed into an external data sheet. Outcomes of interest were pain catastrophizing scores, typically reported as the Pain Catastrophizing Scale16 or Pain Related Catastrophizing Thoughts Scale.17 The duration of treatment protocol and the number of exercise sessions per week were also extracted. These data would then be subsequently imputed into SPSS version 21 (IBM Corp, Armonk, NY) where it was stored and later analyzed.
Certainty of Evidence and Risk of Bias Assessment
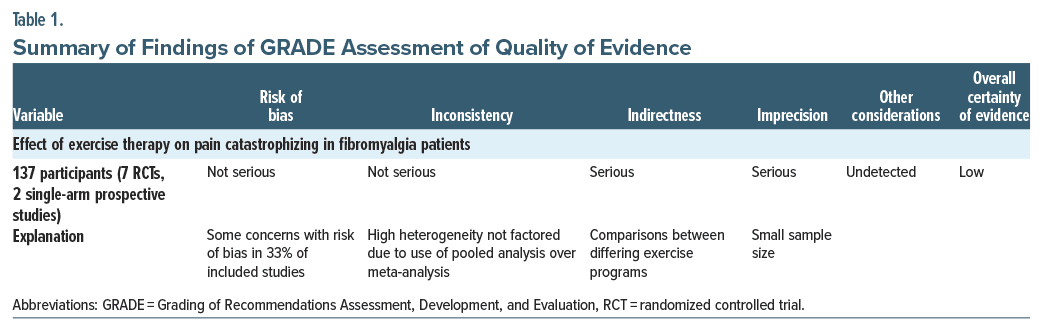
Articles included in the analysis were then scored for certainty of evidence utilizing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria.18 The GRADE criteria and explanation for any decisions to downgrade the quality of evidence are detailed in the summary of findings chart, which was adopted from GRADEpro Guideline Development Tool (Table 1).19
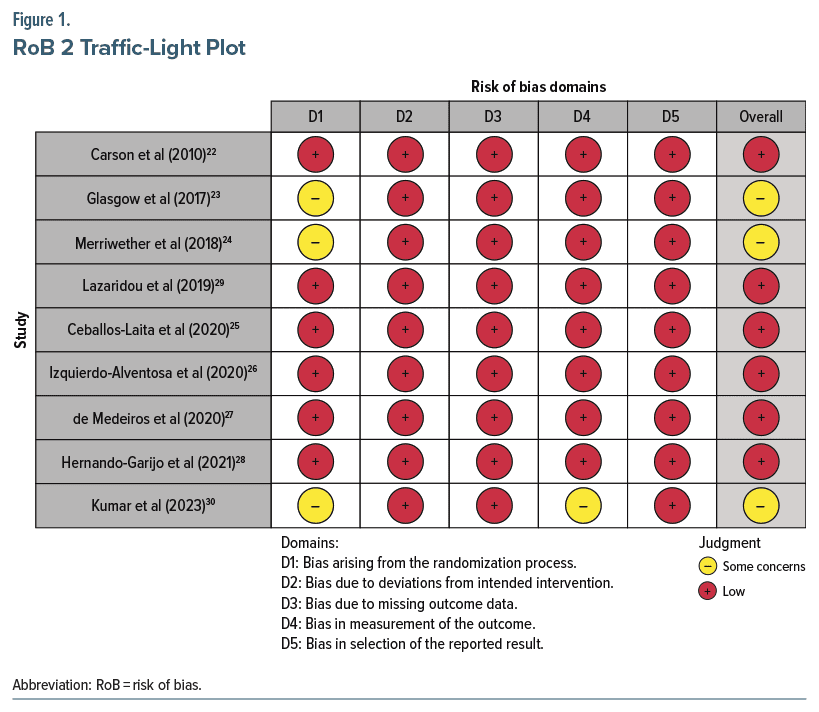
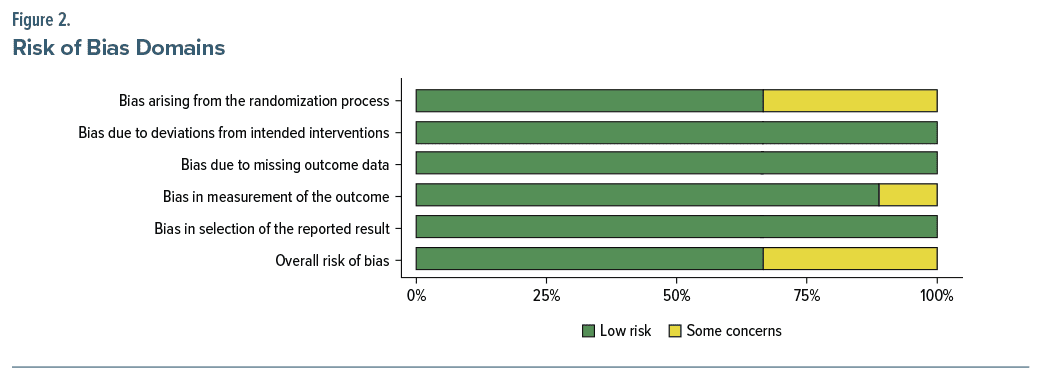
Bias in included articles was assessed using metrics designed for their specific study type. To encompass the included study types, Risk of Bias, version 2 (RoB 2) was employed.20 A description of the domains and the respective determinations for each study are included in Figure 1 and Figure 2, respectively, which were generated using robvis.21
RESULTS
The initial database inquiry resulted in 350 articles. Of the 350 articles, 190 were duplicates leaving 160 articles for title and abstract screening. Of the 160 articles, 15 articles underwent full-text appraisal, after which 9 articles remained. Three articles were studies comparing patients’ current activity level to pain catastrophizing: 1 was a clinical trial protocol article, 1 was an abstract without usable data, and 1 did not have a catastrophizing outcome. Of the articles that met all inclusion criteria, 7 were RCTs,22–28 and 2 were single arm prospective studies.29,30 As of June 2024, 354 fibromyalgia patients underwent some type of exercise therapy for pain catastrophizing. Figure 3 includes the PRISMA flowchart.15
Effect of Intervention
Initial heterogeneity testing denoted an I 2=84%, surpassing Cochrane’s recommendations of a 50% threshold to use random-effects models. Due to the high degree of heterogeneity, meta-analysis was not done. A pooled analysis with subsequent subgroup analyses was conducted instead.
The average exercise intervention lasted roughly 9.1 weeks. The overall effect size of any exercise intervention on pain catastrophizing was d=0.58 (95% CI, 0.16–1.01; P<.01). However, it is important to note that subsequent subgroup analyses denoted differing benefits based on their respective modality. For instance, yoga served as the most clinically effective modality for reducing pain catastrophizing, albeit not statistically significant (d=1.1; 95% CI, −0.48 to 2.69; P=.172). Conversely, treatments such as Pilates, while offering decreases in pain score, did not clinically or statistically reduce pain catastrophizing (d=0.108; 95% CI, −0.522 to 0.738; P=.737). Resistance training, mixed aerobic-resistance exercise, aquatic therapy/exercise, and aerobic exercise all denoted a degree of clinically significant effectiveness (d=0.559, 0.526, 0.548, and 0.226, respectively). It is worth noting that of the other 4 modalities investigated, only mixed aerobic resistance training also achieved statistical significance (P =.046) (Table 2).
Certainty of Evidence and RoB Assessment
GRADE analysis revealed an overall low quality of evidence. Indirect comparisons and a small sample size lowered the certainty of evidence. Other factors that are taken into account for upgrading the quality of evidence (ie, large effect size, dose-response gradient, and plausible confounders that would have reduced effect size) were not applicable (see Table 1).
The RoB assessment revealed some concerns with the RoB in 3 of 9 of the included studies (see Figure 1). Two of the studies were found to have some concerns with the RoB arising from the randomization process. One of the studies was found to have some concerns with the RoB arising from the randomization process and in the measurement of the outcome; however, the RoB across these 2 domains was not enough to substantially lower confidence in the results of the study.
DISCUSSION
This systematic review with pooled analysis sought to determine the effect of various exercise modalities such as yoga, aerobics, mixed aerobics, resistance training, Pilates, and aquatic therapy on pain catastrophizing in fibromyalgia patients. Our initial database inquiry yielded 350 results, of which 9 articles were included in the statistical analysis.
Clinical Efficacy of Exercise Therapies
All exercise types included in the analysis except Pilates denoted some degree of significance in effect size. Yoga had the highest effect size of any exercise therapy (d = 1.105). Three other types of exercise—resistance training, mixed aerobic and resistance, and aquatic therapy (resistance or aerobic)—depict a medium effect size (d = 0.559, 0.526, and 0.548, respectively). Aerobic exercise showed a small effect size for the reduction of pain catastrophizing (d = 0.226).
Unlike every other exercise modality included in this study, yoga focuses on physical exercise in combination with mindfulness and meditation practices. Yoga has a well-documented history of focusing on bodily awareness, such as breathing rate and depth, and has been proposed as an effective mechanism for mitigating pain in previous literature.31 As of now, yoga stands as a strong potential candidate for more research on its impact on pain catastrophizing in fibromyalgia patients.
One possible explanation for the low effect size of Pilates for fibromyalgia patients is the intensity of the exercise. Patients with fibromyalgia often experience widespread pain, fatigue, and sensitivity to physical activity. Pilates, with its unique and often moderate to high-intensity approach, stands in contrast to other low-impact workouts like yoga, especially when incorporating resistance bands, reformers, or weights. Pilates targets core strength and stability through small, repetitive movements. This approach demands increased muscular effort and cardiovascular engagement, enhancing endurance with prolonged position holds.32 However, this intensity may worsen fibromyalgia symptoms, potentially explaining the minimal improvements in pain catastrophizing.
Resistance training demonstrated a clinically significant impact, likely due to its ability to increase muscle mass, endurance, and strength, enhancing overall physical functioning.33 The increased muscle mass can counteract the weakness and fatigue experienced by fibromyalgia patients, reducing pain catastrophizing. Mixed aerobic resistance exercise was the only modality showing both clinical and statistical significance. This exercise combines the benefits of aerobic and resistance training, improving cardiovascular and respiratory health while building muscular strength and endurance.34 This multifaceted approach likely contributes to its effectiveness in alleviating fibromyalgia symptoms. Aquatic therapy/exercise also showed clinical significance, using water to reduce joint and muscle impact while promoting relaxation and reducing pain perception.35 Despite the low-impact nature, water resistance can help to improve muscle strength, making this exercise an ideal choice for fibromyalgia patients who may fear high-impact activities. Finally, although aerobic exercise had a smaller effect size compared to other modalities, it still demonstrated clinical significance by improving cardiovascular fitness, reducing fatigue, and promoting endorphin release, contributing to a reduction in pain catastrophizing.35
Limitations
The study had several limitations. First, the small sample sizes in the included studies reduced the statistical power and limited the generalizability of the findings. Second, the inconsistency in exercise regimens and the varying intensity of each modality across the studies made it difficult to determine the most effective exercise for reducing pain catastrophizing in fibromyalgia patients. Additionally, the high heterogeneity in study designs complicated the comparisons between different exercise modalities further.
Future Directions
Beyond our systematic review, there is a notable lack of large-scale, high-quality randomized controlled trials specifically evaluating the impact of different exercise modalities on pain catastrophizing in fibromyalgia patients. This absence of extensive studies emphasizes the need for more research to create stronger evidence. Future research should focus on combination exercise interventions, such as aerobic-resistance training, and their impact on pain catastrophizing and overall symptom management for fibromyalgia patients. Given yoga’s effectiveness in reducing pain catastrophizing, studies should also identify which aspects of yoga, such as meditation or movement, make it so effective in optimizing exercise prescriptions for fibromyalgia patients. Additionally, the duration and frequency of yoga should be explored to optimize the reduction of pain catastrophizing in fibromyalgia patients.
CONCLUSION
Exercise therapy holds significant potential to decrease pain catastrophizing in fibromyalgia patients. Among the various types of exercise therapies, yoga depicted the largest clinical effect size compared to other modalities, while Pilates did not show any relevant effect sizes. Due to an overall lack of RCTs and standardization in the duration and intensity of exercise therapies, further research is needed to determine the exact benefit of exercise therapy in the reduction of pain catastrophizing.
Article Information
Published Online: March 27, 2025. https://doi.org/10.4088/PCC.24r03817
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 16, 2024; accepted October 14, 2024.
To Cite: Goodwin B, Khan D, Mehta A, et al. Exercise therapies for fibromyalgia catastrophizing: a systematic review and comparative analysis. Prim Care Companion CNS Disord 2025;27(2):24r03817.
Author Affiliations: Futures Forward Research Institute, Toms River, New Jersey (Goodwin, Mehta, Brancaccio, Rubin, Eltman, Davuluri, Lo); Department of Graduate Medical Education, Ocean University Medical Center, Brick Township, New Jersey (Goodwin, Davuluri); Department of Medicine, Rowan-Virtua School of Osteopathic Medicine, Stratford, New Jersey (Khan, Mehta, Brancaccio, Goud, Rubin, Eltman, Lo, King).
Corresponding Author: Brandon Goodwin, DO, Department of Graduate Medical Education, Ocean University Medical Center, Brick Township, NJ 08724 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
ORCID: Brandon Goodwin: https://orcid.org/0000-0002-3965-4664; Danyaal Khan: https://orcid.org/0009-0005-9714-415; Aarti Mehta: https://orcid.org/0009-0009-1891-2124; Hanna Brancaccio: https://orcid.org/0009-0005-8005-9276; Maithri Goud: https://orcid.org/0009-0002-3887-2077; David Rubin: https://orcid.org/0009-0006-2594-8043; Nicholas Eltman: https://orcid.org/0009-0008-4323-6052; Sanjana Davuluri: https://orcid.org/0009-0003-4955-3255; David Lo: https://orcid.org/0000-0003-2408-9735; Alexander King: https://orcid.org/0009-0001-8454-3058
Clinical Points
- Exercise therapy is the cornerstone of conservative fibromyalgia treatment.
- Adjunctive exercise therapies can be potentially beneficial in improving quality of life through reduction in pain catastrophizing.
- Yoga depicted the highest overall effect size for decreasing pain catastrophizing scores.
References (35)

- Maffei ME. Fibromyalgia: recent advances in diagnosis, classification, pharmacotherapy and alternative remedies. Int J Mol Sci. 2020;21(21):7877.
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010;62(5):600–610. PubMed CrossRef
- Bhargava J, Hurley JA. Fibromyalgia. In: StatPearls. StatPearls Publishing; 2023.
- Vincent A, Lahr BD, Wolfe F, et al. Prevalence of fibromyalgia: a population-based study in Olmsted County, Minnesota, utilizing the Rochester Epidemiology Project. Arthritis Care Res (Hoboken). 2013;65(5):786–792. PubMed CrossRef
- Offenbaecher M, Kohls N, Ewert T, et al. Pain is not the major determinant of quality of life in fibromyalgia: results from a retrospective “real world” data analysis of fibromyalgia patients. Rheumatol Int. 2021;41(11):1995–2006.
- Ablin JN, Buskila D. Update on the genetics of the fibromyalgia syndrome. Best Pract Res Clin Rheumatol. 2015;29(1):20–28.
- Gota CE. Fibromyalgia: recognition and management in the primary care office. Med Clin North Am. 2021;105(2):285–296.
- Millea PJ, Holloway RL. Treating fibromyalgia. Am Fam Physician. 2000;62(7):1575–1587.
- Catalá P, Gutiérrez L, Écija C, et al. How to generate self-efficacy despite pain: the role of catastrophizing and avoidance in women with fibromyalgia. Biomedicines. 2023;12(1):47.
- Droppert KM, Knowles SR. The role of pain acceptance, pain catastrophizing, and coping strategies: a validation of the common sense model in females living with fibromyalgia. J Clin Psychol Med Settings. 2023;30(2):445–452.
- Varallo G, Scarpina F, Giusti EM, et al. The role of pain catastrophizing and pain acceptance in performance-based and self-reported physical functioning in individuals with fibromyalgia and obesity. J Pers Med. 2021;11(8):810.
- López-Gómez I, Velasco L, Gutiérrez L, et al. Symptoms in women with fibromyalgia after performing physical activity: the role of pain catastrophizing and disease impact. Clin Rheumatol. 2023;42(1):225–232.
- Lima LV, Abner TS, Sluka KA. Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J Physiol. 2017;595(13):4141–4150. PubMed CrossRef
- Neelapala YV, Mercuri D, Macedo L, et al. Mechanisms hypothesized for pain relieving effects of exercise in fibromyalgia: a scoping review. Ther Adv Musculoskelet Dis. 2023;15:1759720X231182894.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- Sullivan M, Bishop S, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assessment. 1995;7(4):524–532. In press.
- Sarda J, Nicholas MK, Pereira IA, et al. Validation of the Pain-Related Catastrophizing Thoughts Scale. Acta Fisiatr. 2008;15(1):31–36. In press.
- Schünemann H, Brożek J, Guyatt G, et al, eds. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. The GRADE Working Group; 2013. https://guidelinedevelopment.org/handbook
- GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime; 2024. https://gradepro.org
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. PubMed CrossRef
- McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Syn Meth. 2021;12:55–61.
- Carson JW, Carson KM, Jones KD, et al. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010;151(2):530–539. PubMed CrossRef
- Glasgow A, Stone TM, Kingsley JD. Resistance exercise training on disease impact, pain catastrophizing and autonomic modulation in women with fibromyalgia. Int J Exerc Sci. 2017;10(8):1184–1195.
- Merriwether EN, Frey-Law LA, Rakel BA, et al. Physical activity is related to function and fatigue but not pain in women with fibromyalgia: baseline analyses from the Fibromyalgia Activity Study with TENS (FAST). Arthritis Res Ther. 2018;20(1):199. PubMed CrossRef
- Ceballos-Laita L, Mingo-Gómez MT, Navas-Cámara F, et al. Therapeutic exercise and pain neurophysiology education in female patients with fibromyalgia syndrome: a feasibility study. J Clin Med. 2020;9(11):3564.
- Izquierdo-Alventosa R, Inglés M, Cortés-Amador S, et al. Low-intensity physical exercise improves pain catastrophizing and other psychological and physical aspects in women with fibromyalgia: a randomized controlled trial. Int J Environ Res Public Health. 2020;17(10):3634.
- de Medeiros SA, de Almeida Silva HJ, do Nascimento RM, et al. Mat Pilates is as effective as aquatic aerobic exercise in treating women with fibromyalgia: a clinical, randomized and blind trial. Adv Rheumatol. 2020;60(1):21. PubMed CrossRef
- Hernando-Garijo I, Ceballos-Laita L, Mingo-Gómez MT, et al. Immediate effects of a telerehabilitation program based on aerobic exercise in women with fibromyalgia. Int J Environ Res Public Health. 2021;18(4):2075.
- Lazaridou A, Koulouris A, Devine JK, et al. Impact of daily yoga-based exercise on pain, catastrophizing, and sleep amongst individuals with fibromyalgia. J Pain Res. 2019;12:2915–2923. PubMed CrossRef
- Kumar A, Yadav RK, Venkataraman S, et al. Exploring pain status and flexibility in fibromyalgia patients: effect of 20 sessions of yoga therapy. Indian J Physiol Pharmacol. 2023;67:262–269.
- Chopra D, Stern E, Bushell WC, et al. Yoga and pain: a mind-body complex system. Front Pain Res. 2023;4:1075866.
- Kloubec J. Pilates: how does it work and who needs it? Muscles Ligaments Tendons J. 2011;1(2):61–66. PubMed
- Rodríguez-Domínguez ÁJ, Rebollo-Salas M, Chillón-Martínez R, et al. Clinical relevance of resistance training in women with fibromyalgia: a systematic review and meta-analysis. Eur J Pain. 2024;28(1):21–36.
- Bidonde J, Busch AJ, Schachter CL, et al. Mixed exercise training for adults with fibromyalgia. Cochrane Database Syst Rev. 2019;5(5):CD013340. PubMed CrossRef
- Zamunér AR, Andrade CP, Arca EA, et al. Impact of water therapy on pain management in patients with fibromyalgia: current perspectives. J Pain Res. 2019;12:1971–2007.
Enjoy this premium PDF as part of your membership benefits!