Mucopolysaccharidoses (MPS) are a group of rare inborn errors of metabolism.1–3 Each type is due to a lysosomal enzyme deficiency leading to impaired catabolism of glycosaminoglycans that causes the accumulation of abnormal metabolic products.1–3 Morquio syndrome, also known as MPS IV,1–3 has 2 subtypes, A and B, which are due to deficiencies of galactose-6-sulfatase and β-galactosidase, respectively.1–3 Due to the vast number of mutations and allelic heterogeneity, disease presentation can range from mild to severe forms. Those with severe manifestations typically survive up to 20–30 years, whereas patients with milder presentations of MPS IV have been reported to live to their 70s.4,5 The incidence of MPS IVA is 0.22–1.3 per 100,000 live births compared to the less common MPS IVB with an incidence of 0.02–0.14 per 100,000.3,6,7 Because of the greater prevalence and severity of MPS IVA, the clinical features and treatment for Morquio syndrome are generalized predominately from research on type A.
Clinical manifestations of Morquio syndrome are progressive and often start to become apparent by 2–4 years of age.8 Signs of spinal deformity and reduced growth rate are observed as early as 18 months of age.9 Additional clinical manifestations of Morquio syndrome are multisystemic and often present with skeletal dysplasia, short stature, respiratory involvement, corneal clouding, decreased hearing, and dental anomalies.4,10–14 Other forms of MPS, such as subtypes II and III, commonly have coarse facial features and neurological involvement including hyperactivity, attention-deficit/hyperactivity disorder, and aggressive behavior; however, such neurological manifestations are rare in MPS IV, and intellectual ability is often spared.9
Given that few patients with MPS IV live beyond 3 decades of life, little is documented about the disease manifestations in the later stages of life and its relationship with other comorbid conditions typical to such age groups. Moreover, little is known about neurobehavioral manifestations in elderly patients with MPS IV living into the seventh decade of life. The current case is that of an older adult patient with Morquio syndrome requiring psychotropic management in the setting of mood instability and aggression. This case contributes to the growing knowledge of neurobehavioral manifestations in Morquio syndrome and can aid clinicians in the psychopharmacological management of patients with rare MPS.
Case Report
A 73-year-old married white man was referred to a geriatric psychiatry consultant for physical aggression toward nursing staff and other coresidents in his long-term care facility. He was noted for multiple chronic medical conditions including hypertension, glaucoma, hyperlipidemia, benign prostatic hyperplasia, dwarfism, and Morquio syndrome, unspecified type. He had no prior psychiatric conditions including any type of addictive disorder. However, it was noted that he had a history of memory decline.
Pharmacologically, he received atorvastatin, finasteride, latanoprost, bisacodyl, and diltiazem. Additionally, he had been on diazepam 5 mg 3 times a day for anxiety and muscle relaxation for an extended period. Prior to his admission to this facility, he was cared for by his wife and an in-home caregiver. He eventually became a significant burden to his elderly wife, which prompted his admission to the facility approximately 4 months prior. Since his admission, he also became a considerable challenge to the nursing team due to his anxiety, verbal aggression, and refusal of activities of daily living. He then became physically aggressive and nonresponsive to verbal redirections. At his psychiatric evaluation, he was found to be alert but indifferent with poor eye contact and was sitting in a wheelchair. His speech was loud but coherent, speaking only when spoken to. No delusions or hallucinations were noted primarily based on nursing observation. He was nonresponsive to questions as to his mood, while his affect was blunted. He did not respond to questions concerning his cognitive function. However, he was aware that he was not at home. Additionally, there was no fluctuation of his consciousness. His laboratory data including complete blood count, basic metabolic panel, urinalysis, vitamin B12 level, folic acid level, and thyroid-stimulating hormone level were largely unremarkable. Based on a mental status examination and basic laboratory investigations, underlying delirium was ruled out.
At the initial visit, his diazepam was tapered off while he was placed on aripiprazole 2 mg once a day for mood instability. Throughout the follow-up visits, aripiprazole was titrated up based on his response (2 mg once a day for 7 days, 5 mg once a day for 7 days, 7 mg once a day for 7 days, 10 mg once a day for 7 days, and 15 mg once a day eventually). His behavior symptoms became much more manageable at the daily dose of aripiprazole 15 mg. He was markedly calmer and cooperative with his nursing care. However, his affect remained blunted, and he displayed no noticeable side effects from the aripiprazole. Per nursing staff, he was very alert and could follow instructions. In addition, he became compliant with medication and attended recreational therapy sessions.
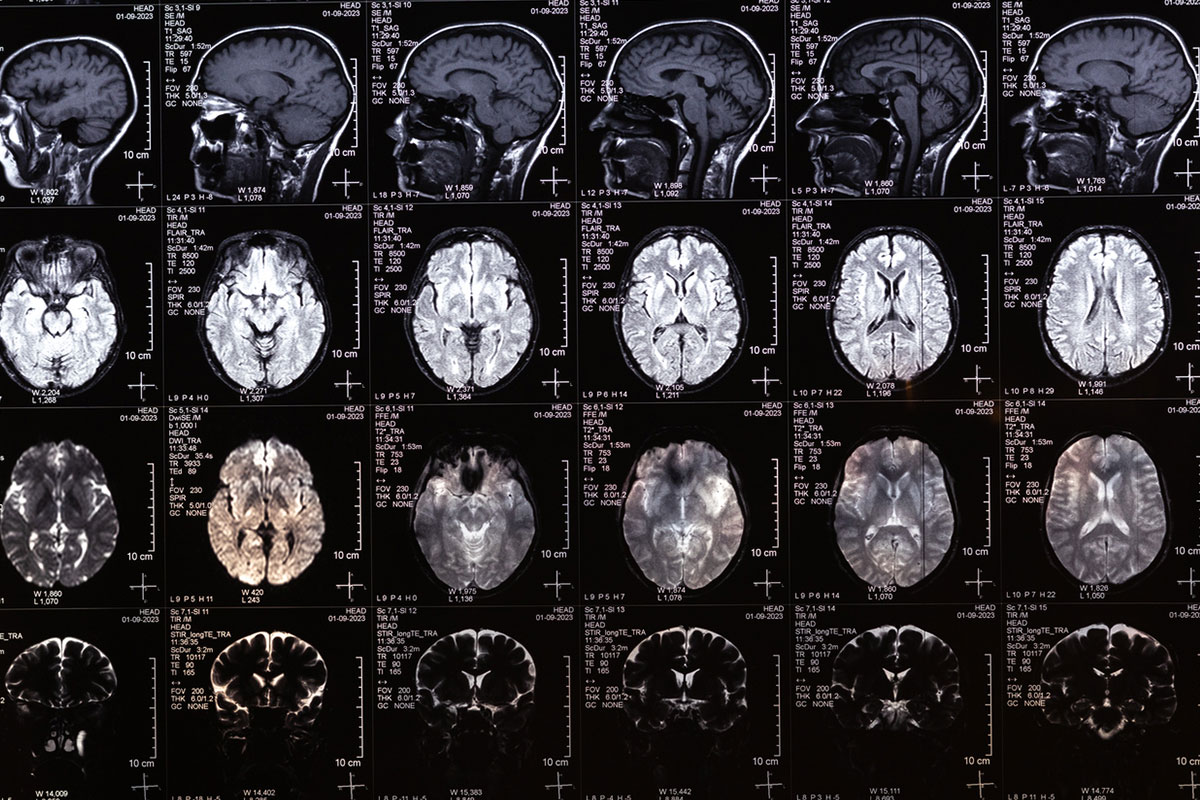
Subsequent to his behavioral stabilization, the patient unfortunately experienced a cerebrovascular accident (CVA) evidenced by brain magnetic resonance imaging without contrast. It demonstrated multiple moderately large infarcts in the posterior circulation involving bilateral occipital lobes and cerebellar hemispheres. Additionally, the right temporal lobe was affected. He was treated in a local medical center and then returned to the same long-term care facility. After the CVA, the patient physically declined in all aspects including significant ataxia but remained behaviorally manageable with the same treatment. His family decided to bring him home on hospice care, where he passed away.
Discussion
There are few studies that include older adults over 65 years of age with Morquio syndrome and even fewer that focus on psychiatric outcomes. In the literature, Morquio syndrome is predominately described as without neurocognitive involvement or psychopathological symptoms.2,3,15,16 However, there is a growing body of evidence that suggests the contrary. There are reports of mild cognitive changes, specifically in areas of attention and hypersocial behavior, and other psychological symptoms, such as anxiety and depression.11,16–20 However, it is important to note that these studies were conducted in primarily pediatric populations or with small sample sizes.
Herein, we report a rare case of an elderly patient with Morquio syndrome exhibiting neurobehavioral symptoms including aggression toward staff and coresidents at his long-term care facility. Due to the lack of official guidelines on managing these symptoms in adult patients with Morquio syndrome, drug selection was primarily based on side effect profiles of available antipsychotic medications. Aripiprazole was the preferred drug because of its overall safety profile in the elderly who are more prone to gait disturbance as well as sedative side effects of antipsychotic medications. The patient’s prior diazepam was tapered off, and the aripiprazole was slowly titrated up on subsequent visits after ensuring the dose was appropriately tolerated and the patient’s clinical response was carefully measured. A daily dose of aripiprazole 15 mg was adequate to resolve his previous aggression; however, his affect remained blunted. Given the patient’s prior history of ataxia, antipsychotics such as risperidone and quetiapine were less favored for symptomatic control to avoid precipitating extrapyramidal and sedative side effects. With aripiprazole treatment, the patient did not display any noticeable adverse effects, such as sedation, tremors, restlessness, and insomnia.
It is important to note that atypical antipsychotic medications should also be used with caution in elderly individuals with known diagnoses of dementia due to a black box warning regarding CVA. While our patient did not have an official diagnosis of dementia, cognitive decline of unknown severity was documented prior to admission to the long-term care facility. Obtaining a full cognitive assessment to investigate underlying dementia is important when considering starting antipsychotic medications in patients with cognitive decline. However, performing a cognitive assessment was difficult in this case given the patient’s ongoing mood instability and agitation in the clinic. Ultimately, the patient experienced a CVA while receiving treatment with aripiprazole, yet it is hard to distinguish whether this was a side effect from antipsychotic therapy or attributable to the patient’s other comorbid medical conditions. When considering initiating aripiprazole in similar patient populations, it is important to fully assess their risk of stroke, including but not limited to history of hypertension, hyperlipidemia, cardiac pathologies, and prior stroke. It is also essential to consider secondary prevention measures, such as statins, antiplatelets, or other medications known to reduce CVA risk. After experiencing the CVA, the patient was transitioned from the long-term care facility to home hospice care due to continued physical decline. If the patient had continued to stay within the long-term care facility, treatment with an antidepressant could have been attempted to address his blunted affect.
This case illustrates the risks and benefits of using aripiprazole for the management of neurobehavioral symptoms in a patient with Morquio syndrome. However, our findings are limited by the treatment of only 1 patient, and more investigation is needed regarding neuropsychiatric outcomes in Morquio syndrome. With advancements in technology and medical treatments, patients with rare diseases, including Morquio syndrome, are living longer and may also need to utilize long-term care facilities. Because management of psychiatric conditions with mood instability and aggression presents significant challenges in long-term care settings,21–23 it is important to identify psychiatric manifestations in patients with rare diseases so that adequate treatment guidelines can be developed to manage their symptoms.
Conclusion
Psychopathologies are under-recognized in Morquio syndrome, especially within geriatric subpopulations. This case is the first, to our knowledge, in the literature to highlight the variable behavioral and mood manifestations as well as well as their managment in an elderly patient in his 70s with Morquio syndrome. Discussed are the risks and benefits of aripiprazole therapy along with the up-titration protocol that successfully reduced the patient’s symptoms of agitation and physical aggression. However, there needs to be further investigation into the safety profile of antipsychotics for the optimal management of comorbidities in older patients with Morquio syndrome.
Article Information
Published Online: September 25, 2025. https://doi.org/10.4088/PCC.25cr03988
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(5):25cr03988
Submitted: April 22, 2025; accepted June 16, 2025.
To Cite: Casado GL, Haymete MA, Jan D, et al. Management of neuropsychiatric symptoms associated with Morquio syndrome. Prim Care Companion CNS Disord 2025;27(5):25cr03988.
Author Affiliations: Virginia Tech Carilion School of Medicine, Roanoke, Virginia (Casado, Haymete, Jan, Kim); Carilion Clinic Center for Healthy Aging, Roanoke, Virginia (Jan, Kim). Casado and Haymete are co-first authors.
Corresponding Author: Kye Y. Kim, MD, Carilion Clinic Center for Healthy Aging, 4434 Electric Rd, Roanoke, VA 24018 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Additional Information: Information has been de-identified to protect patient anonymity.
References (23)

- Cimaz R, La Torre F. Mucopolysaccharidoses. Curr Rheumatol Rep. 2014;16(1):389. PubMed CrossRef
- Hopwood J, Morris CP. The mucopolysaccharidoses. Diagnosis, molecular genetics and treatment. Mol Biol Med. 1990;7(5):381–404. PubMed
- Muenzer J. Overview of the mucopolysaccharidoses. Rheumatology. 2011;50(suppl 5):v4–v12. PubMed CrossRef
- Tomatsu S, Montaño A, Oikawa H, et al. Mucopolysaccharidosis type IVA (Morquio A disease): clinical review and current treatment. Curr Pharm Biotechnol. 2011;12(6):931–945. PubMed CrossRef
- Lavery C, Hendriksz C. Mortality in patients with Morquio syndrome A. In: Zschocke J, Gibson KM, Brown G, et al, eds. JIMD Reports. 15. Springer;2015:59–66.
- Poorthuis BJHM, Wevers RA, Kleijer WJ, et al. The frequency of lysosomal storage diseases in The Netherlands. Hum Genet. 1999;105(1–2):151–156. PubMed CrossRef
- Çelik B, Tomatsu SC, Tomatsu S, et al. Epidemiology of mucopolysaccharidoses update. Diagnostics. 2021;11(2):273. PubMed CrossRef
- Donida B, Marchetti DP, Biancini GB, et al. Oxidative stress and inflammation in mucopolysaccharidosis type IVA patients treated with enzyme replacement therapy. Biochim Biophys Acta. 2015;1852(5):1012–1019. PubMed CrossRef
- Galimberti C, Madeo A, Di Rocco M, et al. Mucopolysaccharidoses: early diagnostic signs in infants and children. Ital J Pediatr. 2018;44(suppl 2):133. PubMed CrossRef
- Bleier M, Yuskiv N, Priest T, et al. Morquio B patient/ caregiver survey: first insight into the natural course of a rare GLB1 related condition. Mol Genet Metab Rep. 2018;16:57–63. PubMed CrossRef
- Gholamian T, Chhina H, Stockler S, et al. Morquio B disease: a case report. Front Pediatr. 2024;12:1285414. PubMed CrossRef
- Harmatz P, Mengel KE, Giugliani R, et al. The Morquio A Clinical Assessment Program: baseline results illustrating progressive, multisystemic clinical impairments in Morquio A subjects. Mol Genet Metab. 2013;109(1):54–61. PubMed CrossRef
- Hendriksz CJ, Harmatz P, Beck M, et al. Review of clinical presentation and diagnosis of mucopolysaccharidosis IVA. Mol Genet Metab. 2013;110(1-2):54–64. PubMed CrossRef
- Montaño AM, Tomatsu S, Gottesman GS, et al. International Morquio A registry: clinical manifestation and natural course of Morquio A disease. J Inherit Metab Dis. 2007;30(2):165–174. PubMed
- Northover H, Cowie RA, Wraith JE. Mucopolysaccharidosis type IVA (Morquio syndrome): a clinical review. J Inherit Metab Dis. 1996;19(3):357–365. PubMed CrossRef
- Shapiro EG, Eisengart JB. The natural history of neurocognition in MPS disorders: a review. Mol Genet Metab. 2021;133(1):8–34. PubMed CrossRef
- Davison JE, Kearney S, Horton J, et al. Intellectual and neurological functioning in Morquio syndrome (MPS IVa). J Inherit Metab Dis. 2013;36(2):323–328. PubMed CrossRef
- Blundell J, Frisson S, Chakrapani A, et al. Markers of cognitive function in individuals with metabolic disease: Morquio syndrome and tyrosinemia type III. Cogn Neuropsychol. 2018;35(3-4):120–147. PubMed CrossRef
- Abumansour IS, Yuskiv N, Paschke E, et al. Morquio-B disease: clinical and genetic characteristics of a distinct GLB1-related dysostosis multiplex. JIMD Rep. 2020;51(1):30–44. PubMed CrossRef
- Ali N, Cagle S. Psychological health in adults with Morquio syndrome. JIMD Rep. 2015;20:87–93. PubMed CrossRef
- Angevaare MJ, van Hout HPJ, Smalbrugge M, et al. The association between possible stressors and mood outcomes in older residents of long-term care facilities. Front Psychiatry. 2022;13:811252. d. PubMed CrossRef
- Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int Psychogeriatr. 2010;22(7):1025–1039. PubMed CrossRef
- Lachs MS, Rosen T, Teresi JA, et al. Verbal and physical aggression directed at nursing home staff by residents. J Gen Intern Med. 2013;28(5):660–667. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!