Spinocerebellar ataxia type 3 (SCA3), otherwise known as Machado-Joseph disease (MJD), is an autosomal dominantly inherited neurodegenerative disease caused by an anticipatory expansion of the cytosine, adenine, and guanine (CAG) trinucleotide repeat in the ATXN3 gene, which codes for aberrantly long polyglutamine tracts in the transcriptome.1 The disease primarily affects the cerebellum, brain stem, and basal ganglia, leading to progressive neurological dysfunction, including but not limited to ataxia, spasticity, and pyramidal and extrapyramidal abnormalities, as well as a range of nonmotor symptoms such as ophthalmoplegia and peripheral neuropathy.2 Pathophysiologically, the accumulation of mutant ataxin-3 protein, characterized by an expanded polyglutamine tract, results in neuronal toxicity, dysfunction, and destruction of cerebral structures.2–4 Current evidence suggests that protein aggregation, mitochondrial dysfunction, and transcriptional dysregulation contribute to disease progression.4–7 Neuroimaging studies frequently demonstrate cerebellar and brain stem atrophy that correlate with clinical severity.8,9
Clinically, SCA exhibits significant heterogeneity, with 3 primary phenotypes categorized by age at onset and symptomatology.8 Type 1 presents early with severe spasticity and dystonia; type 2 encompasses classic cerebellar ataxia and peripheral neuropathy.7–10 MJD, or type 3, is marked by a later onset and milder symptoms and is the most common subtype of SCA among these 3 variants.11 Genetic testing confirming the CAG repeat expansion remains the leading diagnostic tool to distinguish among each specific type.12
Treatment of MJD is symptomatic and not curative, focusing on managing the motor and nonmotor manifestations.8 Currently, no disease-modifying therapies exist for this disease.8,13 Research has investigated molecular and gene-editing approaches, such as antisense oligonucleotides to target the underlying genetic abnormality.6,7 Physical and occupational therapy play critical roles in improving quality of life for patients with MJD.14
Psychiatric comorbidities in patients with MJD are frequently observed, significantly impacting quality of life. Studies assessing self-rated mental health in MJD patients highlight a high prevalence of mental health concerns, with depressive symptoms being the most prevalent.15 Further, investigations into the psychological burden of MJD have demonstrated that these neuropsychiatric manifestations can extend beyond patients to their relatives, emphasizing the hereditary and psychosocial dimensions of the disease.16 Additionally, mood disturbances and emotional dysregulation have been documented, suggesting a neurological basis for psychiatric symptoms in MJD.17 These findings underscore the necessity of comprehensive neuropsychiatric evaluation and integrated management strategies to improve patient outcomes in MJD.
This case report contributes to the limited literature on MJD, specifically highlighting the neuropsychiatric symptomology of the disease and how management may be approached in future older adult patients who might struggle with similar acute-onset psychiatric concerns.
Case Report
A 73-year-old divorced, white woman, residing in a long-term care facility, was referred to geriatric psychiatry services with chief concern for worsening behavioral symptoms, including verbal threats toward staff and mood instability. She also exhibited paranoid ideation, particularly directed at nursing staff, leading to challenges in providing her care. The patient frequently refused assistance with activities of daily living (ADLs) and attempted unsafe transfers from bed, raising significant safety concerns.
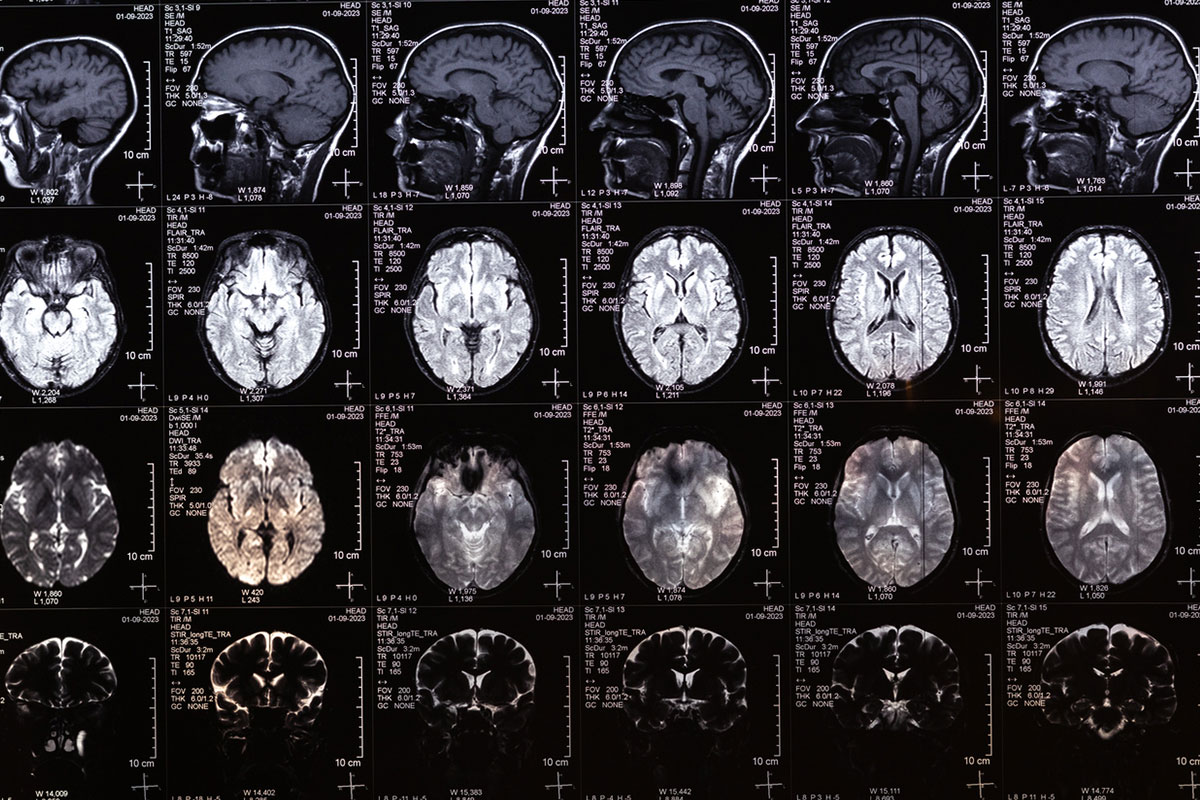
Her medical history was significant for hypertension, recurrent falls, muscle weakness, and MJD. She was diagnosed with MJD at age 58 years after presenting with progressive right-hand weakness, thenar atrophy, dysarthria, ataxia, generalized weakness, and orthostatic symptoms. Magnetic resonance imaging demonstrated pontocerebellar atrophy consistent with multisystem atrophy, and genetic testing confirmed a SCA3 mutation.
The patient’s family history was notable for bipolar disorder in her sister, diabetes in her mother, and alcohol abuse in her brother. She had a history of heavy smoking, having quit at age 40 years, and frequent alcohol consumption, averaging 10–15 glasses of wine weekly before entering the facility. She had no prior psychiatric history but was recently diagnosed with major depressive disorder, unspecified, and started on sertraline by her primary care provider, titrated to 100 mg daily. For chronic insomnia, she was prescribed trazodone 75 mg and melatonin 3 mg at bedtime. Comprehensive laboratory workup, including erythrocyte sedimentation rate, thyroid function tests, vitamin B12, folic acid, rheumatoid factor, and serum protein electrophoresis, was unremarkable.
Mental status examination revealed an apprehensive but engaged patient. She reported her mood as “sad,” with congruent affect marked by depression and anxiety. She expressed nonspecific accusatory remarks about the nursing staff, such as “they don’t like me,” while displaying intact cognitive function. She was aware of her depressive and anxious state and complained of sleep difficulties, including trouble initiating sleep and early awakening.
Given her persistent insomnia, trazodone and melatonin were replaced with mirtazapine, titrated to 15 mg at bedtime. This intervention improved her sleep to 6 consistent hours nightly. However, irritability, verbal agitation, and depressive symptoms persisted. Sertraline was subsequently discontinued and replaced with escitalopram, titrated to 20 mg daily, which reduced her depressive and anxious symptoms. Despite these improvements, verbal agitation and resistance to care persisted, necessitating the initiation of aripiprazole 2 mg daily for mood instability.
Within 9 days of starting aripiprazole, the patient demonstrated improved cooperation and redirection during ADL care. At a 3-month follow-up, she remained on the same regimen, with no reported side effects and stable behavioral improvements.
Discussion
This case highlights the complexity of managing acute-onset neuropsychiatric symptoms in patients with a history of MJD and underscores the importance of integrating cognitive and behavioral considerations into their care. While MJD is primarily recognized as a neurodegenerative condition with motor and cerebellar symptoms, its treatment recommendations for managing the neuropsychiatric manifestations do not have cohesive guidelines due to the individualized case-by-case basis for symptom severity or prevalence.
While it is known that neuropsychiatric manifestations such as depression or cognitive impairments are not uncommon in MJD, there is a paucity of reported literature on the behavioral aspect seen in this case. The patient’s presentation of mood instability, irritability, and verbal agitation—alongside her paranoid ideation—raises the question of whether these symptoms are a direct extension of the neurodegenerative process or secondary to environmental stressors and medical comorbidities. While current literature recognizes some psychiatric complications of MJD, such as major depression and mood disorders, this case adds to the growing body of evidence suggesting a broader spectrum of neuropsychiatric symptoms, including depression, anxiety, and behavioral dysregulation, in this inherited disease state.
The management of such cases requires an interdisciplinary approach. This patient’s improvement with targeted psychopharmacological interventions, including the use of mirtazapine for sleep disturbances and escitalopram combined with aripiprazole for mood and behavioral symptoms, highlights the potential role of a structured and individualized treatment plan. Importantly, the rapid response to aripiprazole emphasizes its clinical efficacy in addressing acute behavioral disturbances in patients with neurodegenerative conditions, providing a possible avenue for future research and establishing evidence- based guidelines specific to these concerns.
Additionally, this case underscores the need for increased vigilance when new psychiatric symptoms emerge in patients with neurodegenerative diseases and late-onset genetically inherited disease states. It is essential to differentiate between primary psychiatric conditions, medication side effects, or behavioral changes related to neurodegenerative progression. Comprehensive workup, including imaging, genetic studies, and laboratory testing, remains crucial to rule out contributing organic or systemic factors, particularly in the aging population with MJD.
Conclusion
This case is significant because it contributes to the current understanding of neuropsychiatric co-occurrences in MJD. It also serves as a reminder of the importance of tailoring psychiatric management in neurodegenerative conditions, with careful consideration of safety and quality-of-life implications in long-term care settings. Further research into the neuropsychiatric aspects of MJD and related disorders could help inform future therapeutic guidelines and improve patient neuropsychiatric and cognitive outcomes.
Article Information
Published Online: September 2, 2025. https://doi.org/10.4088/PCC.25cr03955
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(5):25cr03955
Submitted: March 1, 2025; accepted May 8, 2025.
To Cite: Tanchanco C, Wong J, Kim K. Management of neurobehavioral symptoms associated with Machado-Joseph disease. Prim Care Companion CNS Disord. 2025; 27(5):25cr03955.
Author Affiliations: Virginia Tech Carilion School of Medicine, Roanoke, Virginia (Tanchanco, Wong, Kim); Department of Psychiatry, Carilion Clinic, Roanoke, Virginia (Kim).
Corresponding Author: Kye Kim, MD, Carilion Clinic Center for Healthy Aging, 4434 Electric Rd, Roanoke, VA 24018 ([email protected];[email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Additional Information: Information has been de-identified to protect patient anonymity.
ORCID: Kye Kim: http://orcid.org/0000-0003-2543-5230
References (17)

- Bettencourt C, Lima M. Machado-Joseph Disease: from first descriptions to new perspectives. Orphanet J Rare Dis. 2011;6(1):35. PubMed CrossRef
- Matos CA, de Almeida LP, Nóbrega C. Machado-Joseph disease/spinocerebellar ataxia type 3: lessons from disease pathogenesis and clues into therapy. J Neurochem. 2019;148(1):8–28. PubMed CrossRef
- Onofre I, Mendonça N, Lopes S, et al. Fibroblasts of Machado Joseph disease patients reveal autophagy impairment. Sci Rep. 2016;6(1):28220. PubMed CrossRef
- Almeida F, Ferreira IL, Naia L, et al. Mitochondrial dysfunction and decreased cytochrome c in cell and animal models of Machado-Joseph disease. Cells. 2023;12(19):2397. PubMed CrossRef
- Nóbrega C, Simões AT, Duarte-Neves J, et al. Molecular mechanisms and cellular pathways implicated in Machado-Joseph disease pathogenesis. Adv Exp Med Biol. 2018;1049:349–367. PubMed CrossRef
- Raposo M, Bettencourt C, Vieira Melo AR, et al. Novel Machado-Joseph disease-modifying genes and pathways identified by whole-exome sequencing. Neurobiol Dis. 2022;162:105578. PubMed CrossRef
- Sullivan R, Yau WY, O’Connor E, et al. Spinocerebellar ataxia: an update. J Neurol. 2019;266(2):533–544. PubMed CrossRef
- Mendonça N, França MC Jr, Gonçalves AF, et al. Clinical features of Machado-Joseph disease. Adv Exp Med Biol. 2018:1049:255–273. PubMed
- Murata Y, Yamaguchi S, Kawakami H, et al. Characteristic magnetic resonance imaging findings in Machado-Joseph disease. Archives Neurology. 1998;55(1):33–37. PubMed CrossRef
- Schmitz-Hübsch T, Coudert M, Bauer P, et al, Spinocerebellar ataxia types 1, 2, 3, and 6: disease severity and nonataxia symptoms. Neurology. 2008;71(13):982–989. PubMed CrossRef
- Schöls L, Bauer P, Schmidt T, et al. Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurology. 2004;3(5):291–304. PubMed CrossRef
- Tsai H-F, Liu C-S, Leu T-M, et al. Analysis of trinucleotide repeats in different SCA loci in spinocerebellar ataxia patients and in normal population of Taiwan. Acta Neurol Scand. 2004;109(5):355–360. PubMed CrossRef
- Ogawa M. Pharmacological treatments of cerebellar ataxia. Cerebellum. 2004;3(2):107–111. PubMed CrossRef
- D’Abreu A, França MC Jr, Paulson HL, et al. Caring for Machado-Joseph disease: current understanding and how to help patients. Parkinsonism Relat Disord. 2010;16(1):2–7. PubMed
- Kawai Y, Takeda A, Abe Y, et al. Cognitive impairments in Machado-Joseph disease. Archives neurology. 2004;61(11):1757–1760. PubMed CrossRef
- Schmitz-Hübsch T, Coudert M, Giunti P, et al. Self-rated health status in spinocerebellar ataxia-results from a European multicenter study. Movement Disord. 2010;25(5):587–595. PubMed
- Cecchin CR, Pires AP, Rieder CR, et al. Depressive symptoms in Machado-Joseph disease (SCA3) patients and their relatives. Community Genet. 2007;10(1):19–26. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!