Lyme disease, caused by Borrelia burgdorferi and transmitted by Ixodes ticks, is the most common vector-borne illness in the United States.1 While erythema migrans is its hallmark symptom, Lyme disease and coinfections can also present with systemic and neuropsychiatric symptoms, including depression, anxiety, fatigue, and cognitive impairments affecting attention, memory, and sleep.2,3 In high-risk regions, these symptoms are often misdiagnosed as primary psychiatric conditions or attributed to other postviral syndromes.3 This case report underscores the need for timely screening and treatment of Lyme disease and other tick-borne coinfections in patients with neuropsychiatric symptoms in tick-endemic areas.
Case Report
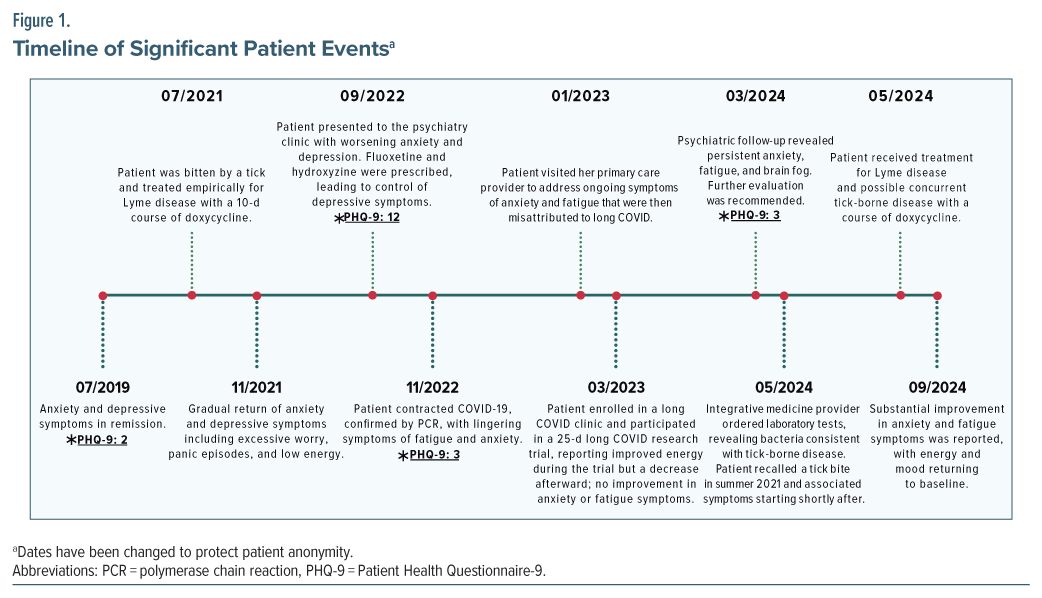
A 23-year-old woman with a history of major depressive disorder and generalized anxiety disorder presented to the psychiatry clinic in September 2022 with anxiety and depressive symptoms after 6 years of remission on escitalopram 30 mg daily. She reported excessive worry, panic episodes, nausea, shortness of breath, anhedonia, low energy, and disrupted sleep. Her Patient Health Questionnaire-9 (PHQ-9) score increased from 2 (2019) to 12 (September 2022).4 With no recent psychosocial stressors or substance use, her treatment was adjusted by cross-tapering escitalopram with fluoxetine 10 mg, which was titrated up to 20 mg daily by October 2022.
In January 2023, after a COVID-19 infection in November 2022, the patient reported further worsening of anxiety, low mood, fatigue, and “brain fog,” which were initially attributed to long COVID. While fluoxetine improved her depressive symptoms (PHQ-9 score dropped from 12 to 3), her anxiety and fatigue persisted. She participated in a blinded long COVID research trial (Paxlovid vs placebo) in March 2023 but noted minimal relief. By January 2024, despite remission of depressive symptoms, her anxiety and brain fog persisted. Following the trial, she noticed a decline in energy and was prescribed metoprolol by cardiology for palpitations, which was ineffective.
In March 2024, given her persistent symptoms, her psychiatrist recommended further evaluation with integrative medicine. In May 2024, polymerase chain reaction urine testing revealed positive results for Borrelia miyamotoi, Borrelia recurrentis-IND, and Ehrlichia chaffeensis-IND. Living in a tick-endemic region of North Carolina, she recalled a tick bite in summer 2021, after which she had fatigue, fever, headache, and joint pain but no erythema migrans rash. She received a 10-day course of doxycycline at an urgent care clinic but later realized that her anxiety, depression, and fatigue began after this tick bite, not after COVID-19 infection. Following treatment with doxycycline, her fatigue and mood improved significantly, and by September 2024, she reported restored energy and a return to baseline.
Discussion
This case highlights the diagnostic challenges of Lyme disease and other tick-borne infections, particularly when symptoms overlap with psychiatric conditions like depression, anxiety, and long COVID. The patient’s symptoms were initially misattributed to long COVID, delaying diagnosis for over a year, which underscores the need for clinicians to consider tick-borne diseases in patients with unexplained neuropsychiatric symptoms, especially in endemic regions.5
Lyme disease and other tick-borne infections are common in North America, particularly in the Northeast, Mid-Atlantic, and Upper Midwest, with increasing cases in the Southeast.1,6 Their neuropsychiatric symptoms, such as depression, anxiety, cognitive impairment, and sleep disturbances, often mimic primary psychiatric disorders, making thorough history taking and diagnostic testing essential.2
Borrelia miyamotoi, spread by Ixodes scapularis and Ixodes pacificus, causes hard tick relapsing fever (HTRF), which typically presents within 2 weeks postbite with fever, chills, fatigue, nausea, headache, and myalgia.7 While most cases resolve on their own, severe infections require antibiotics.7 Though less common than Lyme disease, HTRF follows a similar geographic pattern and peaks in August.7 Borrelia recurrentis, transmitted by Pediculus humanus humanus (human body lice), causes louse-borne relapsing fever (LBRF), primarily in overcrowded African regions.8 Symptoms resemble other relapsing fevers but occur less frequently, with pregnant women at higher risk for complications.8 LBRF is rare in the United States unless linked to travel.8 Ehrlichia chaffeensis, spread by the lone star tick (Amblyomma americanum), causes human ehrlichiosis, mostly in the southeastern and eastern United States.9 Symptoms include fever, chills, muscle aches, fatigue, and headache, with severe cases leading to organ failure, especially in immunocompromised individuals.8 Preventing tick bites with repellents and avoiding tick habitats remain key.9
In this case, the patient received a 10-day empiric course of doxycycline without confirmatory testing.2 Notably, doxycycline is often used first line in the treatment of Borrelia miyamotoi, Borrelia recurrentis, Ehrlichia chaffeensis, and Borrelia burgdorferi infections.10,11 While early treatment is common, it may have contributed to a missed diagnosis of concurrent infections. Persistent fatigue, worsening depression, and anxiety were initially attributed to postviral syndrome, delaying proper treatment. Serologic testing in 2024 confirmed additional infections, and targeted antimicrobial therapy led to significant improvement, suggesting an undiagnosed tick-borne disease.12
Diagnosing Lyme disease with neuropsychiatric symptoms requires clinical evaluation and serologic testing, including enzyme-linked immunosorbent assay and Western blot for Borrelia burgdorferi antibodies.5 In suspected neuroborreliosis, cerebrospinal fluid analysis may be helpful.13 Early antibiotic therapy, such as doxycycline or ceftriaxone, is crucial for managing both infection and psychiatric effects, with adjunctive psychiatric treatments as needed.5
Untreated tick-borne infections can worsen psychiatric symptoms, leading to chronic depression or anxiety.2,3 If the disease progresses, neuroborreliosis may develop, presenting with cognitive impairment, psychiatric symptoms, meningitis, or cranial nerve palsies.12 Thorough history taking and diagnostic testing are essential to avoid misdiagnosis, particularly in patients with persistent fatigue and depression who may have had tick exposure.12
A multidisciplinary approach was key in this case. Comprehensive blood testing in May 2024, as shown in Figure 1, identified an overlooked infectious cause, reinforcing the value of integrative medicine and collaboration across specialties in complex cases, especially when standard treatments failed.
Conclusion
In summary, this case highlights the need to consider Lyme disease and other tick-borne infections in patients with persistent neuropsychiatric symptoms, especially in endemic regions. Symptom overlap with conditions like long COVID can delay diagnosis, emphasizing the importance of thorough evaluation and serologic testing, including consideration for retesting tick-borne infection to confirm complete resolution in patients with prior documented disease. Early diagnosis and antimicrobial treatment are crucial for resolving both the infection and its neuropsychiatric effects.
Article Information
Published Online: August 14, 2025. https://doi.org/10.4088/PCC.25cr03948
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(4):25cr03948
Submitted: February 2, 2025; accepted May 23, 2025.
To Cite: McDuffee NS, Steinour M, Shah K. Neuropsychiatric manifestation of Tick-borne disease and the importance of screening in endemic regions. Prim Care Companion CNS Disord 2025;27(4):25cr03948.
Author Affiliations: Atrium Wake Forest Baptist Health, Department of Psychiatry, Wake Forest School of Medicine, Winston-Salem, North Carolina (McDuffee); Mental Health and Behavioral Sciences, W.G. “Bill” Hefner VA Medical Center, Salisbury, North Carolina (Steinour); Kernersville Health Care Center, Kernersville, North Carolina (Steinour); Department of Psychiatry, Wake Forest Atrium Baptist Health, Winston-Salem, North Carolina (Shah).
Corresponding Author: Nicholas S. McDuffee, MA, BS, Atrium Wake Forest Baptist Health, Department of Psychiatry, Wake Forest School of Medicine, 1 Medical Center Blvd, Winston-Salem, North Carolina 27157 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information, including dates, has been de-identified to protect patient anonymity.
References (13)

- Eisen RJ, Eisen L. The blacklegged tick, Ixodes scapularis: an increasing public Health concern. Trends Parasitol. 2018;34(4):295–309. PubMed CrossRef
- Hündersen F, Forst S, Kasten E. Neuropsychiatric and Psychological symptoms in patients with Lyme disease: a study of 252 patients. Healthcare (Basel). 2021;9(6):733. PubMed CrossRef
- Maxwell SP, Brooks C, McNeely CL, et al. Neurological pain, Psychological symptoms, and diagnostic struggles among patients with tick-borne diseases. Healthcare. 2022;10(7):1178. PubMed CrossRef
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. PubMed CrossRef
- Rachman M, Garfield DA. Lyme disease and secondary depression: universal lessons from an uncommon case. Psychosomatics. 1998;39(3):301–302. PubMed CrossRef
- Centers for Disease Control and Prevention. About Lyme Disease. Yellow Book; 2024. Accessed February 3, 2025. https://www.cdc.gov/lyme/about/index.html
- Centers for Disease Control and Prevention. Hard Tick Relapsing Fever (HTRF). Yellow Book; 2022. Accessed February 13, 2025. https://www.cdc.gov/relapsing-fever/about/about-htrf.html
- Centers for Disease Control and Prevention. About Louse-borne Relapsing Fever. Yellow Book; 2022. Accessed February 13, 2025. https://www.cdc.gov/relapsing-fever/about/about-lbrf.html
- Centers for Disease Control and Prevention. About Ehrlichiosis. Yellow Book; 2022. Accessed February 13, 2025. https://www.cdc.gov/ehrlichiosis/index.html
- Ho BM, Davis HE, Forrester JD, et al. Wilderness medical society clinical practice guidelines for the prevention and management of tick-borne illness in the United States. Wilderness Environ Med. 2021;32(4):474–494. PubMed CrossRef
- Wormser GP, Warshafsky S, Visintainer P. Aggregation of data from 4 clinical studies demonstrating efficacy of single-dose doxycycline postexposure for prevention of the spirochetal infections: Lyme disease, syphilis, and tick-borne relapsing fever. Diagn Microbiol Infect Dis. 2021;99(4):115293. PubMed CrossRef
- Fallon BA, Nields JA. Lyme disease: a neuropsychiatric illness. Am J Psychiatry. 1994;151(11):1571–1583. PubMed CrossRef
- Kobayashi T, Higgins Y, Melia MT, et al. Mistaken identity: many diagnoses are frequently misattributed to Lyme disease. Am J Med. 2022;135(4):503–511.e5. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!