ABSTRACT
Objective: To assess the prevalence of psychiatric disorders among children and adolescents in child welfare custody admitted to the hospital.
Methods: Data were collected from the 2016–2017 National Inpatient Sample of the US population of general hospital admissions. Data for patients aged 12–17 years who were in child welfare custody were obtained using the ICD-10 diagnosis code Z6221: child in welfare custody. The control group comprised patients not in child welfare custody. Groups were compared for demographic, clinical, and hospital characteristics.
Results: The study group included 879 child welfare patients, of whom 38.9% were male, with a mean age of 14.7 years. The control group comprised 222,494 patients, of whom 41.2% were male, with a mean age of 14.9 years. In the study group, 69.4% of patients had mood disorders compared to 28.6% in the control group. Half of the patients in the study group had anxiety disorders and almost 44% had ADHD and other conduct disorders compared to 19.3% and 14.2%, respectively, in the control group. Prevalence of suicidal ideation/attempt was almost 3 times higher in the study group compared to controls (41.0% vs 14.8%), and 18.3% of study group patients had a substance use disorder compared to 8.3% of controls. Mood disorders were the most common reason for hospitalization (44.8% vs 19.2%), followed by ADHD/other conduct disorders (5.3% vs 1.1%) and anxiety disorders (4.9% vs 0.9%).
Conclusions: Children and adolescents in the child welfare system are associated with a higher risk of mental health problems. More studies are needed to identify the factors that contribute to psychiatric comorbidities in this population and to determine and address the factors that can prevent mental health issues.
Prim Care Companion CNS Disord 2023;25(6):22m03238
Author affiliations are listed at the end of this article.
Psychiatric disorders among children and adolescents are described as serious deviations from expected cognitive, social, and emotional development.1 In the United States, 13%–20% of children experience a psychiatric disorder in a given year, and an estimated $247 billion is spent each year on childhood mental disorders.1 At least 1 of every 5 youth aged 9–17 years has a diagnosable mental health disorder that causes some degree of impairment, and 1 of every 10 has a disorder that causes significant impairment.2 In 2016, 3.2% of US children and adolescents were diagnosed with depression, 7.1% with anxiety, and 7.4% with behavioral/conduct disorders.3 Psychiatric disorders are observed to have an early onset in childhood or adolescence, which increases the risk for poor physical health, social relationship issues, impaired psychological health, and financial problems.4,5
Several predictive factors were identified for the development of psychiatric disorders in children, which mainly include child and child caregiver factors.6,7 Child-related factors for developing psychiatric disorders are age, sex, ethnicity, physical health, cognitive and psychological function, prenatal and perinatal exposures to physical stress, illnesses, alcohol, drugs, nutrition, infections, and other environmental agents. Caregiver factors include parental psychiatric and medical history, education, age, socioeconomic status, and employment.6,7
Lifetime child maltreatment prevalence in the United States of youth aged < 18 years is about 12.5%.8 After controlling for sex, race/ethnicity, and age, youth in child welfare were significantly more likely to report multiple types of maltreatment than those in mental health or juvenile justice settngs.9 In 2018, almost 678,000 children were victims of maltreatment, increasing from nearly 674,000 in the year 2017. Additionally, more than 15% of the victims experienced ≥ 2 types of maltreatment.10 Child protective services agencies received and reported a national estimate of 4.4 million (4,378,000) total referrals in the year 2019.11 The child welfare system is responsible for ensuring the safety, permanency, and well-being of children and adolescents who have been maltreated. Types of maltreatment experienced by children in the child welfare system include physical abuse, sexual abuse, neglect, domestic violence, parental substance abuse, poverty, community violence, and numerous other insults.12
Children involved in the child welfare system are at higher risk for mental health problems and poorer mental health outcomes than children in the general population.13,14 Children with behavioral and/or developmental issues are more prone to remain in the child welfare system.14
In the United States, the yearly cost of care for a child in the child welfare system is about $35,000.14 High prevalence rates of psychiatric disorders such as depression,15,16 anxiety,15,16 attention-deficit/hyperactivity disorder (ADHD),17 conduct disorder,18 behavior problems,13 suicide,19–22 and substance abuse23–25 in these children are reported.
The objective of this study was to assess the prevalence of psychiatric disorders among children and adolescents in child welfare custody admitted to the hospital. The study reports the prevalence of psychiatric disorders and substance use disorders among children (aged 12–17 years) in child welfare custody from a large, representative nationwide inpatient sample dataset from 2016 to 2017. In addition, this study examines how youth who differ by sex, race, type of out-of-home placement, and region of residence vary in the rates meeting diagnostic criteria.
METHODS
Dataset
Data were collected from the 2016–2017 national representative sampling of the US population of general hospital admissions. The National Inpatient Sample (NIS) is sponsored by the Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality.26 A detailed description of the dataset is provided at https://www.hcup-us.ahrq.gov/.
Study Groups
Data for patients aged 12–17 years who were in child welfare custody (study group) were obtained using the ICD-10 diagnosis code Z6221: child in welfare custody. The control group comprised patients not in child welfare custody. Groups were compared for demographic, clinical, and hospital characteristics. Data on psychiatric comorbidities were collected using the ICD-10 code provided in the Clinical Classifications Software of the dataset.27 Data were collected on age, sex, race, and income categories for the patient’s zip code for the demographic characteristics. Hospitalization characteristics were hospital location, region, bed size, length of stay, and cost of hospitalization. We included the following psychiatric comorbidities: mood disorders, anxiety disorders, psychotic disorders, personality disorders, suicidal ideation/attempt, and ADHD/other conduct disorders.
Statistical Analysis
Mean (standard error) was used to describe continuous data, and percentage was used for the categorical data type. Group comparison was performed using the survey analysis technique, and independent-sample t test and Rao-adjusted χ2 test were used to compare groups. A P value < .05 was considered statistically significant. Cost to charge ratio files were used to convert hospitalization charges into the cost. Length of stay and hospitalization cost were compared (adjusted for age, sex, hospital characteristics) between the 2 groups for patients admitted to the hospital for psychiatric reasons.28 All the analyses were performed using SPSS software, version 26.0 (IBM Corp, 2020).
RESULTS
The study group included 879 patients, of whom 38.9% were male, with a mean age of 14.7 years. The control group included 222,494 patients, of whom 41.2% were male, with a mean age of 14.9 years. Table 1 provides the demographic and hospital characteristics. There was minimal difference in average age between the groups. Sex distribution was similar between the groups. The study group had more Black patients and less Hispanic patients compared to the control group. The groups did not differ in hospital characteristics such as location (rural or urban) and type by bed size (small/medium/large). More patients in the study group were from the area with a median household income ≤ 50th percentile. More patients in the study group were from the Midwest (46.1%) compared to the Northeast (7.3%).
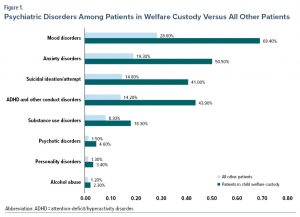
Figure 1 shows the comparison of psychiatric comorbidities between the groups. A higher number of child welfare patients had psychiatric comorbidities compared to controls. In the study group, 69.4% of patients had mood disorders and 50.5% had anxiety disorders compared to 28.6% and 19.3%, respectively, in the control group. Almost 44% of patients had ADHD and other conduct disorders in the study group versus 14.2% in the control group. Prevalence of suicidal ideation/attempt was almost 3 times higher in the study group compared to the control group (41.0% vs 14.8%), and 18.30% of patients had a substance use disorder in the study group compared to 8.3% in the control group.
Hospitalization related to mental health conditions was also common among the study group, with 57.0% of patients admitted for psychiatric disorders compared to 22.1% in the control group. Hospitalization due to mood disorders was most common (44.8% vs 19.2%), followed by ADHD/other conduct disorders (5.3% vs 1.1%) and anxiety disorders (4.9% vs 0.9%). After adjusting for age, sex, and hospital characteristics (bed size, ownership, region, location), the average length of hospitalization for patients with psychiatric disorders was significantly higher among the study group (14.0 days vs 6.6 days, P < .001). Cost of hospitalization was also high in the study group ($9,493 vs $5,745, P < .001). However, no difference in hospitalization cost was observed when adjusted for length of stay (P = .61).
DISCUSSION
This study uniquely compared children in child welfare custody with matched controls. We found that about two-thirds of patients in the child welfare group had mood disorders. Patients in the child welfare group also had increased rates of anxiety disorders and ADHD compared to the control group. The estimated suicide attempt/ideation prevalence among the child welfare patients was found to be as high as 3 times that of the control group. Concurrently, patients in the child welfare group were diagnosed with substance use disorder at rates 2 times that of the control group. Patients in the control group had a lower hospitalization rate in terms of mental health conditions compared to the child welfare patients. Mood disorder was the common cause of hospitalization in both groups, but the prevalence in child welfare patients was twice as high as that of controls. Child welfare patients also had higher rates of psychiatric hospitalization due to ADHD and anxiety disorders compared to controls.
Heneghan et al29 assessed data from the National Survey on Child and Adolescent Well-being examining depression, anxiety, substance use/abuse, suicidality, and ADHD in teens (aged 12–17.5 years) referred to child welfare agencies. The study29 showed that overall placement location and prior child welfare history were not associated with the psychiatric issues mentioned previously. However, the study reported an overall increase (8.9%, 23.0%, and 13.9%) over the past decade for depression, substance use/abuse, and suicidality, respectively, for teens aged 12–17 years in child welfare custody.29 In comparison, our study reported a remarkably higher number of psychiatric problems and mood disorders in child welfare patients compared to controls. Our study did not focus on psychiatric problem trends longitudinally.
A study by Sullivan and Van Zyl30 evaluated children’s medical and emotional needs in foster care. Another prospective study31 with similar objectives assessed the mental health needs of children from different counties in Tennessee after referral to child welfare and juvenile justice, in-home, and case management services. Few studies provide evidence of the benefits of specialty mental health care in decreasing the need for out-of-home placements among children in child foster care. However, these studies30,31 focus on the needs of child welfare patient populations in certain US states. Thus, they lack generalizability. In comparison, our study provides a census from the NIS from across the US comparing child welfare patients and matched controls.
Policy Implications
We found that children who enter the welfare custody system are at increased risk of mental health comorbidities. Our findings have significant implications for improving preventive mental health services and the cost of care containment for children in welfare custody.
Our findings have important public health implications. First, a thorough and complete mental health screening and assessment program of children removed from their homes is required. Second, mechanisms need to be identified to integrate current guidelines into practice, as such an approach will assist in the prevention and long-term consequences of mental health problems. Third, a comprehensive and effective public policy should include the estimated child welfare costs and economic burdens at large for feasible and practical implications.
Research indicates that mental health reasons can compel a child to stay in welfare custody longer, thus increasing the cost of child maintenance.32 However, existing literature does not highlight the additional cost of maintaining a child with psychiatric comorbidities compared to children with no psychiatric conditions. Moreover, there is a lack of research in longitudinal economic costs and practical screening programs to identify and track these parameters. Such research questions will be critical to decrease the cost of care and mental health burden.
Our study has limitations. Despite selecting the child welfare custody group samples from the NIS randomly, we did not assess the previous history of mental health problems or associated risk factors (eg, history of abuse, family conflicts, domestic violence, and family history of mental health disorders). This omission can limit conclusions as to whether the higher frequency of mental health problems and hospitalization among children in child welfare custody are solely due to predisposing factors or that these children are more prone to mental health problems. Also, the majority of the samples were from the urban population (94.9%). A more generalizable sample size from both urban and rural areas could robustly increase the external validity of the study design. The cost of mental health services in children who remain in welfare custody compared to control groups could also have been included in the creation of the study. A cost-effective analysis can provide a strong justification for policymakers and legislators to tailor the existing guidelines accordingly and provide better health care services for children who remain in welfare custody. Finally, the dataset is a discharge-level record instead of individual patients. Despite these limitations, this study is the first, to our knowledge, to compare and contrast mental well-being in children in welfare custody to matched controls not in welfare custody.
Clinical Significance
Information is scarce regarding the prevalence of mental disorders among children and adolescents in the child welfare system.33 A possible reason for this scarcity could be that child welfare and mental health agencies function in different jurisdictions, and diagnostic information is not typically shared between systems. However, an increased interagency collaboration between child welfare and mental health agencies might help bridge this information gap.34 Children in child welfare custody have higher rates of psychiatric conditions and need more specialized care. The implications of failing to address adolescent mental health conditions continue into adulthood, affecting both physical and mental health and constraining opportunities to live fulfilling lives as adults. Early diagnosis and intervention can help reduce the mental health burden and cost.
CONCLUSIONS
Our study results indicate that children in the child welfare system are associated with a higher risk of mental health problems. However, more longitudinal studies are needed to identify the factors contributing to psychiatric comorbidities in this population and to determine and address the factors that can prevent mental health issues.
Article Information
Published Online: November 21, 2023. https://doi.org/10.4088/PCC.22m03238
© 2023 Physicians Postgraduate Press, Inc.
Submitted: January 5, 2022; accepted March 3, 2023.
To Cite: Mainali P, Vadukapuram R, Trivedi C, et al. Prevalence of psychiatric disorders among children and adolescents from child welfare custody admitted to the hospital: a nationwide inpatient sample analysis. Prim Care Companion CNS Disord. 2023;25(6):22m03238.
Author Affiliations: Department of Psychiatry, Case Western University/Metro Health Medical Center, Cleveland, Ohio (Mainali); Department of Psychiatry, The University of Texas Rio Grande Valley, Harlingen (Vadukapuram); Texas Tech University Health Sciences Center at Permian Basin, Midland (Trivedi, Jain); Texas Tech University Health Sciences Center at Lubbock (Yousufzai); Boston Children’s Hospital/Harvard Medical School, Massachusetts (Mansuri).
Author Contributions: Drs Mainali and Vadukapuram share equal credits for first authorship. Drs Mansuri and Jain share equal credits for senior authorship.
Corresponding Author: Pranita Mainali, MD, Case Western University/Metro Health Medical Center, 2500 Metro Health Dr, Cleveland, OH 44109 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- A high prevalence of psychiatric disorders was identified in hospitalized children and adolescents in child welfare custody.
- Suicidal ideation and attempt were 3 times higher in child welfare patients compared to controls.
- Factors that can prevent psychiatric comorbidities in the child welfare population should be identified and addressed.
References (34)

- Perou R, Bitsko RH, Blumberg SJ, et al; Centers for Disease Control and Prevention (CDC). Mental health surveillance among children–United States, 2005–2011. MMWR suppl. 2013;62(2):1–35. PubMed
- Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. PubMed CrossRef
- Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. 2019;206:256–267.e3. PubMed CrossRef
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. PubMed CrossRef
- Jones PB. Adult mental health disorders and their age at onset. Br J Psychiatry suppl. 2013;202(s54):s5–s10. PubMed CrossRef
- Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7–20. PubMed CrossRef
- Reinherz HZ, Paradis AD, Giaconia RM, et al. Childhood and adolescent predictors of major depression in the transition to adulthood. Am J Psychiatry. 2003;160(12):2141–2147. PubMed CrossRef
- Sabol W, Coulton C, Polousky E. Measuring child maltreatment risk in communities: a life table approach. Child Abuse Negl. 2004;28(9):967–983. PubMed CrossRef
- Stewart SL, Thornley E, Lapshina N, et al. Sex differences in youth with mental health problems in inpatient, outpatient and youth justice settings. BMC Psychiatry. 2020;20(1):11. PubMed CrossRef
- Child abuse, neglect data released. January 15, 2020. The Administration for Children and Families. Accessed October 20, 2023. https://www.acf.hhs.gov/media/press/2020/2020/child-abuse-neglect-data-released#:%7E:text=In%20total%2C%2060.8%20percent%20of,7.0%20percent%20were%20sexually%20abused.&text=A%20national%20estimate%20of%201%2C770,died%20in%20fiscal%20year%202017
- Children’s Bureau. January 15, 2020. The Administration for Children and Families. Accessed October 20, 2023. https://www.acf.hhs.gov/cb/data-research/child-maltreatment
- Levitt JM. Identification of mental health service need among youth in child welfare. Child Welfare. 2009;88(1):27–48. PubMed
- Aarons GA, James S, Monn AR, et al. Behavior problems and placement change in a national child welfare sample: a prospective study. J Am Acad Child Adolesc Psychiatry. 2010;49(1):70–80. PubMed CrossRef
- Leslie LK, Gordon JN, Lambros K, et al. Addressing the developmental and mental health needs of young children in foster care. J Dev Behav Pediatr. 2005;26(2):140–151. PubMed CrossRef
- Naylor MW, Wakefield SM, Morgan W, et al. Depression in children and adolescents involved in the child welfare system. Child Adolesc Psychiatr Clin N Am. 2019;28(3):303–314. PubMed CrossRef
- Lehmann S, Havik OE, Havik T, et al. Mental disorders in foster children: a study of prevalence, comorbidity and risk factors. Child Adolesc Psychiatry Ment Health. 2013;7(1):39. PubMed CrossRef
- Klein B, Damiani-Taraba G, Koster A, et al. Diagnosing attention-deficit hyperactivity disorder (ADHD) in children involved with child protection services: are current diagnostic guidelines acceptable for vulnerable populations? Child Care Health Dev. 2015;41(2):178–185. PubMed CrossRef
- Bronsard G, Alessandrini M, Fond G, et al. The prevalence of mental disorders among children and adolescents in the child welfare system: a systematic review and meta-analysis. Medicine (Baltimore). 2016;95(7):e2622. PubMed CrossRef
- Farand L, Chagnon F, Renaud J, et al. Completed suicides among Quebec adolescents involved with juvenile justice and child welfare services. Suicide Life Threat Behav. 2004;34(1):24–35. PubMed CrossRef
- Fulginiti A, He AS, Negriff S. Suicidal because I don’t feel connected or vice versa? a longitudinal study of suicidal ideation and connectedness among child welfare youth. Child Abuse Negl. 2018;86:278–289. PubMed CrossRef
- Ruch DA, Steelesmith DL, Warner LA, et al. Health services use by children in the welfare system who died by suicide. Pediatrics. 2021;147(4):e2020011585; Advance online publication. PubMed CrossRef
- Katz LY, Au W, Singal D, et al. Suicide and suicide attempts in children and adolescents in the child welfare system. CMAJ. 2011;183(17):1977–1981. PubMed CrossRef
- Goldstein AL, Faulkner B, Wekerle C. The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child Abuse Negl. 2013;37(1):22–32. PubMed CrossRef
- Yarnell LM, Traube DE, Schrager SM. Brief report: Growth in polysubstance use among youth in the child welfare system. J Adolesc. 2016;48(1):82–86. PubMed CrossRef
- Seay KD. Detection of problematic substance use in the child welfare system: a comparison of self-report and caseworker report. Child Maltreat. 2019;24(2):152–160. PubMed CrossRef
- HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2012. Agency for Healthcare Research and Quality, Rockville, MD. Accessed October 20, 2023. www.hcup-us.ahrq.gov/nisoverview.jsp
- Clinical Classifications Software Refined (CCSR). Healthcare Cost and Utilization Project (HCUP). March 2021. Agency for Healthcare Research and Quality, Rockville, MD. Accessed October 20, 2023. www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp.
- Cost-to-Charge Ratio for Inpatient Files. Healthcare Cost and Utilization Project (HCUP). December 2020. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/db/ccr/ip-ccr/ip-ccr.jsp.
- Heneghan A, Stein RE, Hurlburt MS, et al. Mental health problems in teens investigated by US child welfare agencies. J Adolesc Health. 2013;52(5):634–640. PubMed CrossRef
- Sullivan DJ, Van Zyl MA. The well-being of children in foster care: Exploring physical and mental health needs. Child Youth Serv Rev. 2008;30(7):774–786. CrossRef
- Glisson C, Green P. The role of specialty mental health care in predicting child welfare and juvenile justice out-of-home placements. Res Soc Work Pract. 2006;16(5):480–490. CrossRef
- Fang X, Brown DS, Florence CS, et al. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse Negl. 2012;36(2):156–165. PubMed CrossRef
- McMillen JC, Zima BT, Scott LD Jr, et al. Prevalence of psychiatric disorders among older youths in the foster care system. J Am Acad Child Adolesc Psychiatry. 2005;44(1):88–95. PubMed CrossRef
- Hurlburt MS, Leslie LK, Landsverk J, et al. Contextual predictors of mental health service use among children open to child welfare. Arch Gen Psychiatry. 2004;61(12):1217–1224. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!