Abstract
Objective: Polycystic ovary syndrome (PCOS) symptoms extend beyond reproductive issues, impacting mental health significantly, with noted correlations to anxiety, depression, and suicide attempts. The objective of this study was to quantify psychiatric comorbidities among adolescent females with PCOS.
Methods: Utilizing the National Inpatient Sample dataset from January 2016 to December 2018, this study examined a cohort of female adolescents aged 14–17 years diagnosed with PCOS, identified via International Classification of Diseases, Tenth Revision, Clinical Modification code E28.2, and matched 1:2 with non-PCOS individuals on demographic variables using propensity score matching. The primary outcomes included the prevalence of psychiatric disorders and were analyzed through categorical and continuous variable comparisons, employing t tests and Rao-Scott adjusted χ2 tests, with odds ratios calculated to assess associations.
Results: The study encompassed 11,985 patients, highlighting a significantly higher prevalence of mood disorders, major depressive disorder, and anxiety disorders in the PCOS cohort compared to controls (P < .001). Specifically, mood disorders were reported in 43.6% of the PCOS group. Attention-deficit/hyperactivity disorder/conduct disorders were also more prevalent in the PCOS population. However, rates of schizophrenia and suicidal ideation/attempts did not significantly differ between groups.
Conclusion: Adolescents with PCOS exhibit increased psychiatric comorbidities, highlighting the urgent need for integrated care strategies. Future research should aim to elucidate the mechanisms underlying these associations and develop effective interventions to improve outcomes in this vulnerable population.
Prim Care Companion CNS Disord 2024;26(6):24m03760
Author affiliations are listed at the end of this article.
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder within the female reproductive-age population, affecting an estimated 6%–13% of women and 6%–18% of adolescent girls.1–3 It is a complex, heterogeneous disorder characterized by clinical or biochemical signs of elevated androgens, irregular or absent menstrual periods due to chronic lack of ovulation, and the presence of polycystic ovaries, as observed in ultrasound imaging.4 Elevated androgen levels in individuals with PCOS disrupt the normal regulation of gonadotropins, such as luteinizing hormone and follicle-stimulating hormone, through impaired feedback mechanisms with progesterone and estrogen.5 Consequently, people with PCOS often exhibit an increased luteinizing hormone to follicle-stimulating hormone ratio, leading to ovarian dysfunction and the continuous excess production of androgens. This hormonal imbalance is associated with several symptoms, including infertility, acne, painful menstruation, excessive hair growth, and obesity.6
PCOS is a chronic condition with symptoms starting in adolescence and evolving into infertility and metabolic issues.7 It leads to psychological distress (poor quality of life, depression, and anxiety) and reproductive problems (infertility and pregnancy complications) and negatively affects self-image due to weight gain, acne, and excessive hair growth.8–10 These challenges severely impact mental health and quality of life. Research indicates that females with PCOS have increased odds of depression and anxiety and higher rates of suicide attempts.11–13 Mood disturbances and low self-esteem also hinder the adoption of lifestyle changes essential for managing the condition, pushing the patient into a downward spiral.6 In 2021, the total annual direct health care costs for the mental health disorders associated with PCOS surpassed $4 billion for the US population.14
There has been no large-scale study conducted specifically within the adolescent population to quantify psychiatric comorbidities among adolescent females with PCOS. The prevailing hypothesis suggests that the development of PCOS is primarily driven by insulin resistance and hyperinsulinemia, which in turn lead to hyperandrogenism. This hormonal imbalance not only contributes to reproductive and metabolic abnormalities but is also believed to increase the prevalence of psychiatric conditions in individuals with PCOS, particularly depression and anxiety. These psychological disturbances may arise from the hyperandrogenism and the physical manifestations of PCOS, such as obesity, acne, and hirsutism.15 Such symptoms can be incredibly stigmatizing for adolescent girls who are at a pivotal stage of developing their identity and body image awareness.16 The consensus recommendation suggests that adolescent girls diagnosed with PCOS should undergo screening for anxiety and depression. However, this advice is derived from data on adult women since the prevalence of psychiatric comorbidity among adolescent girls remains undetermined.17 The current study aims to address this gap in the literature.
METHODS
Data Source
The study utilized data from the National Inpatient Sample (NIS) dataset 2016–2018, a component of the Healthcare Cost and Utilization Project (HCUP).18 The NIS dataset comprises discharge records representing approximately a 20% stratified sample of all discharges from US community hospitals, excluding rehabilitation and long-term acute care hospitals. Additional information about the dataset is available on the official HCUP website: https://www.hcup-us.ahrq.gov/.
Study Population
The research cohort consisted of female adolescents aged 14–17. Patients with PCOS were identified using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code E28.2. A propensity score matching methodology was applied to construct a comparative control cohort, adhering to a 1: 2 case-to-control ratio. This strategy involved aligning subjects diagnosed with PCOS with non-PCOS individuals, ensuring matching based on demographic variables such as age and race to mitigate confounding factors and enhance the validity of comparative analyses.
Propensity Score Matching
To address potential confounding effects and achieve equivalence in baseline characteristics between the PCOS cohort and the control group, we implemented propensity score matching employing the MatchIt package within the R statistical computing environment (version 3.6.3).19 A matching ratio of 1:2 was chosen to ensure an adequate representation of controls relative to the PCOS cases. Matching was conducted in a random sequence utilizing the nearest neighbor matching algorithm, applying a caliper width of 0.0001, thereby minimizing bias.
Outcomes
The primary outcomes examined were the prevalence rates of psychiatric disorders among adolescents with PCOS compared to the control group. We also investigated mental health conditions, including mood disorders, major depressive disorder, adjustment disorders, bipolar disorder, anxiety disorders, attention deficit/hyperactivity disorder (ADHD)/conduct disorders, schizophrenia, and suicidal ideation/attempts.
Statistical Analysis
Categorical variables are presented as percentages, while continuous variables are summarized using means and standard errors. The independent samples t test and the Rao-Scott adjusted χ2 test were applied for group comparisons. A descriptive analysis characterized the patient population, displaying results in tabular format. The Rao-Scott adjusted χ2 test was employed to compare the prevalence rates of mental health disorders between the PCOS and control groups. Odds ratios (ORs) were calculated to evaluate the strength of the association between PCOS and psychiatric disorders, with a predetermined significance threshold of P < .05.
Given the large sample size, patients with missing data were excluded to enhance the accuracy of the analysis. The statistical methodology incorporated complex survey data analysis techniques, taking into account variables such as the NIS stratum, hospital identification codes, and discharge weights from the NIS dataset. These analyses were performed using the widely used and trusted SPSS version 26.0.
RESULTS
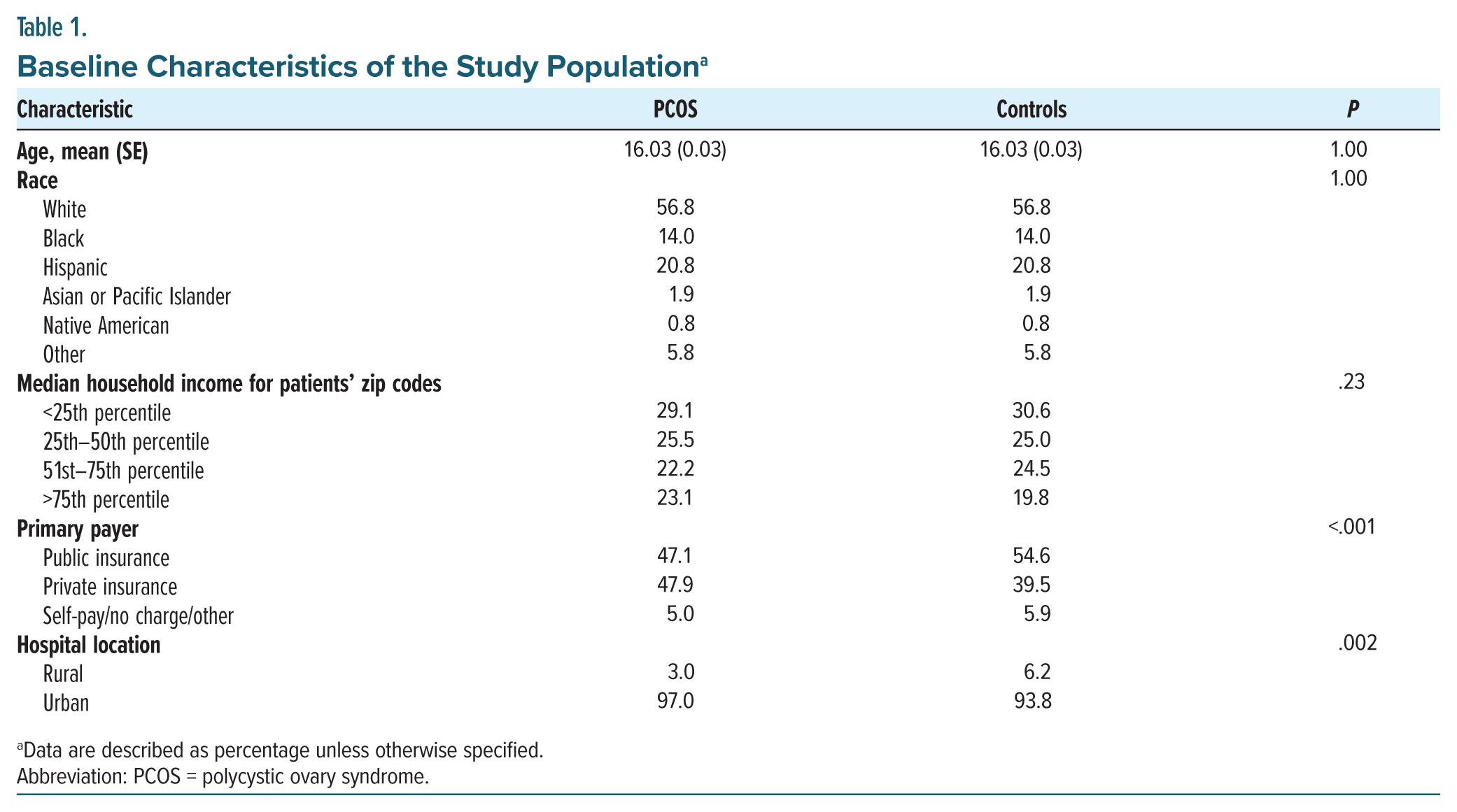
The analysis encompassed 11,985 patients, divided into 3,995 patients in the PCOS cohort and 7,990 patients in the non-PCOS cohort. The average age was 16.03, with the age distribution as follows: 9.1% were 14 years old, 17.5% were 15 years old, 34.9% were 16 years old, and 38.4% were 17 years old. Racially, 56.8% were white, 14% were black, and 20.8% were Hispanic (Table 1).
Significant disparities were observed in socioeconomic status indicators, such as hospital location and primary payer source, between the PCOS and control groups, showing P values <.001. The PCOS group demonstrated a higher prevalence of private insurance coverage (47.9% compared to 39.5% in the control group). The control group had a larger share of public insurance beneficiaries (54.6% vs 47.1% in the PCOS group). Additionally, a greater proportion of patients with PCOS were admitted to urban hospitals than those in the control group (97.0% vs 93.8%, P = .002).
Figure 1 presents the prevalence of psychiatric disorders, highlighting that adolescents diagnosed with PCOS exhibited significantly higher rates of mood disorders than those in the non-PCOS group (43.6% vs 33.1%, OR = 1.56, P < .001). Specifically, within the PCOS cohort, the prevalence of major depressive disorder was 36.5%, and bipolar disorder was observed in 5.5% of patients. Anxiety disorders were significantly more prevalent in adolescents with PCOS compared to the non-PCOS group (37.5% vs 25.1%, OR = 1.80, P < .001).
Additionally, ADHD/conduct disorders were more prevalent among adolescents with PCOS compared to those without (11.8% vs 8.0%, P = .002). In contrast, the prevalence rates of schizophrenia (1.9% vs 1.3%, P = .24) and suicidal ideation (19.6% vs 18.3%, P = .74) did not significantly differ between the PCOS and non-PCOS groups. Furthermore, no significant association was found between PCOS and adjustment disorders.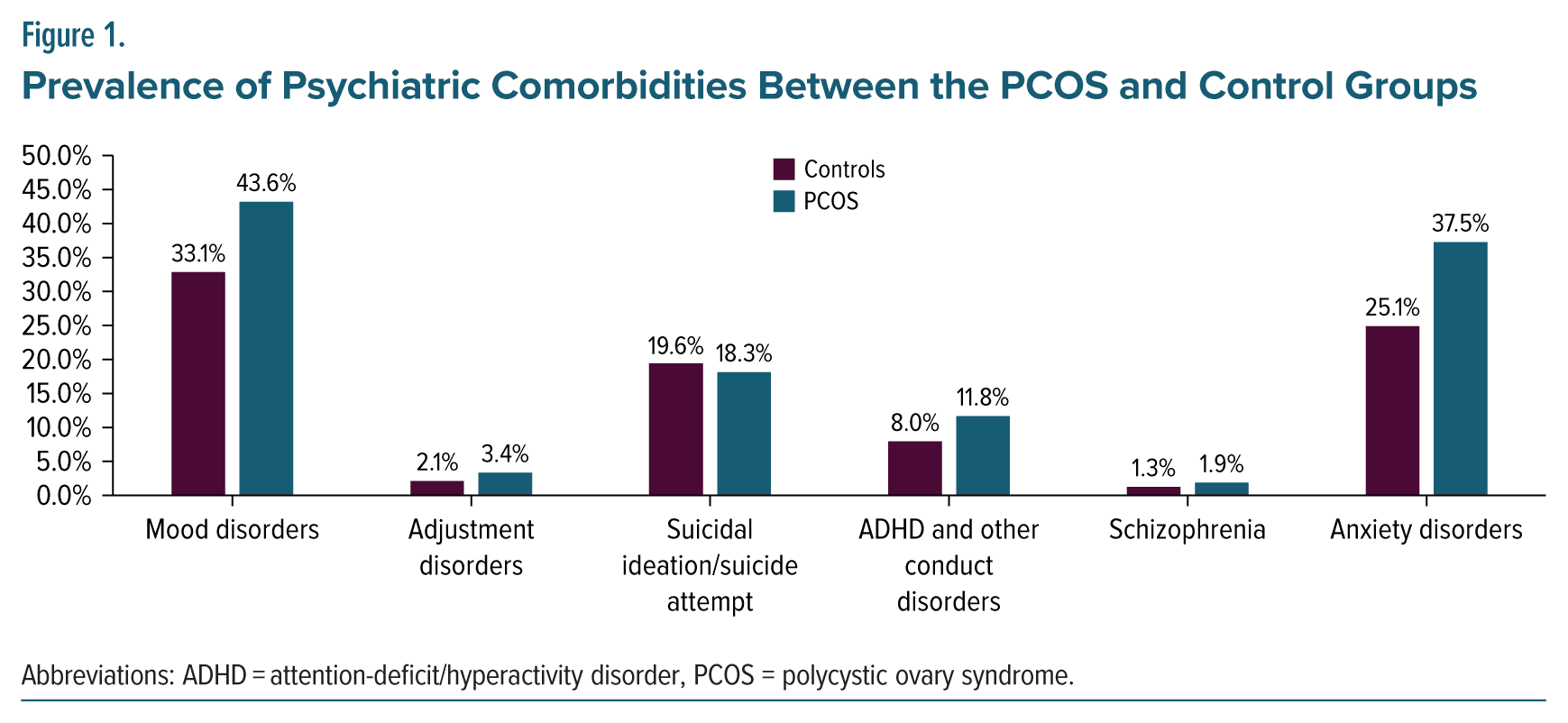
DISCUSSION
Our study revealed a significantly higher prevalence of mood disorders, major depressive disorder, and anxiety among hospitalized adolescents with PCOS compared to their non-PCOS counterparts. Specifically, mood disorders were present in 43.6% of the PCOS group vs 33.1% of the control group, indicating a substantial impact of PCOS on mental health in adolescents. Additionally, the incidence of ADHD/conduct disorders was notably higher in the PCOS population. In contrast, schizophrenia and suicidal ideation rates did not significantly differ between groups, suggesting a complex and selective relationship between PCOS and psychiatric conditions.
The increased prevalence of mood dysfunctions and psychiatric disorders in adolescent girls with PCOS aligns with literature that has mainly focused on adults.13 Studies highlight diminished quality of life,20 with high anxiety and depression rates in women with PCOS.11,21 The distress from PCOS symptoms significantly impacts mood, with obesity and insulin resistance affecting both reproductive and psychological aspects of PCOS.22–24 A link between depressive symptoms and high androgen levels has been noted.25,26 Although the association between psychiatric comorbidities and PCOS is established, the causal mechanisms, including obesity, insulin resistance, elevated androgens, hypothalamic-pituitary dysregulation, and increased inflammation, remain to be fully elucidated, indicating a multifactorial influence on psychiatric outcomes in PCOS.27
Only a limited number of studies, characterized by small sample sizes and other methodological limitations, have focused exclusively on psychiatric comorbidity in adolescent patients with PCOS.28–30 Most research has concentrated solely on adult patients or included a mix of adult and pediatric populations.13,31
Evidence suggests that adolescents with PCOS have higher odds of anxiety, depressive disorders, and body dysmorphic concerns relative to non-PCOS counterparts.28,30 The syndrome’s associated symptoms, including menstrual dysregulation and potential fertility impairment, significantly exacerbate stress levels in affected adolescents. Furthermore, the correlation between adverse body image perceptions—specifically perceived overweight status and dermatologic issues such as acne and hirsutism—leads to persistent psychological distress, ongoing dissatisfaction with physical appearance, and enduring reproductive anxieties.30
Our research is the first systematic examination of psychiatric comorbidities in hospitalized adolescents with PCOS using a large dataset. While our results may not represent the wider community, it is significant that no previous studies, to our knowledge, have directly compared the prevalence of depression, bipolar disorder, ADHD/conduct disorder, schizophrenia, and suicidal ideation between adolescents with and without PCOS.
In our study, schizophrenia prevalence showed no significant difference between PCOS and non-PCOS groups, consistent with Karjula et al,32 who found unchanged schizophrenia rates despite increased non schizophrenia psychoses in PCOS. Surprisingly, we observed no increase in suicidal ideation or attempts among hospitalized adolescents with PCOS, diverging from expected trends.30
The higher prevalence of PCOS observed in urban and privately insured adolescents may suggest an underdiagnosis in low-income and rural areas, potentially due to limited access to health care and variability in clinician awareness. However, these considerations are speculative and were not addressed by the current study design. Further targeted research is necessary to explore these potential disparities.
The absence of a significant difference in the rates of suicidal ideation or attempts between adolescents with PCOS and those without, as observed in this study, may be attributed to several methodological and contextual factors inherent to the study’s design and data source. First, utilizing the NIS dataset, which predominantly includes data from inpatient hospital stays excluding rehabilitation and long-term acute care facilities, may not capture the full spectrum of mental health conditions, particularly those managed outside the inpatient setting. This dataset may thus underrepresent the prevalence of suicidal ideation or attempts that do not result in hospitalization. Second, the study’s reliance on ICD-10-CM codes for identifying PCOS and psychiatric conditions, including suicidal ideation or attempts, could lead to underreporting due to coding inaccuracies or the omission of relevant codes. Third, propensity score matching aimed to control for confounding variables such as age and race. However, other unmeasured confounders related to socioeconomic status, access to mental health services, or the severity of PCOS symptoms might have influenced the findings. Moreover, despite the attempt to match these cohorts on demographic variables, the significant disparities observed in socioeconomic status indicators and insurance coverage between the PCOS and control groups suggest that socioeconomic factors may play a crucial role in the access to and quality of mental health care received by these populations. This, in turn, could impact the reported rates of psychiatric disorders and suicidal behaviors.
Our study highlights the significant impact of PCOS on the mental health of adolescents, revealing a higher prevalence of mood disorders and anxiety in this population compared to their non-PCOS counterparts. It underscores the essential need for targeted mental health screening and treatment strategies tailored explicitly to adolescents with PCOS. Despite finding no significant differences in schizophrenia prevalence and suicidal ideation rates, our research calls for a deeper examination of the complex relationship between PCOS and psychiatric outcomes in adolescents. By focusing on a large dataset, this study fills a critical gap in research on psychiatric comorbidity among adolescents with PCOS, emphasizing the urgency of early detection and intervention to enhance their mental health and overall quality of life.
STRENGTHS AND LIMITATIONS
The study, which utilizes the NIS dataset has made significant strides in analyzing psychiatric comorbidities in adolescents with PCOS, particularly focusing on females aged 14–17. Its rigorous methodology, including propensity score matching and adjustment for demographics, has not only minimized confounding but also strengthened its validity. By covering a wide range of psychiatric disorders and employing advanced statistical analyses, the study provides robust findings, thereby enhancing our understanding of the mental health challenges faced by this demographic.
However, the study has several limitations. The study’s cross-sectional nature limits its ability to establish causality between PCOS and psychiatric disorders, only allowing for the observation of associations. Excluding patients with missing data may introduce bias, affecting the study’s accuracy and representativeness. The lack of longitudinal data prevents analysis of the temporal relationship between PCOS and psychiatric conditions. Significant socioeconomic and health care access differences were noted but not thoroughly examined as potential influencers. The study’s omission of medication history and reliance on visit records rather than on individual patient data raise concerns about the potential for duplicate counts and unaccounted pharmacologic effects. Despite using propensity score matching to balance groups, the possibility of residual confounding by unmeasured factors could still influence the results.
CONCLUSION
This study provides strong evidence that adolescents with PCOS have increased psychiatric comorbidities, especially mood and anxiety disorders. The PCOS-related hormonal changes and psychosocial challenges during adolescence likely contribute to this vulnerability. These findings underscore significant unmet mental health needs in this high-risk group that demand urgent attention. Our results advocate proactive psychiatric screening and multimodal care integrating medical, psychological, and social factors for adolescents with PCOS. Ultimately, this study reinforces the critical need for a comprehensive, multidimensional approach to the clinical management of PCOS that addresses both physical and psychiatric morbidities.
Article Information
Published Online: November 7, 2024. https://doi.org/10.4088/PCC.24m03760
© 2024 Physicians Postgraduate Press, Inc.
Submitted: April 18, 2024; accepted July 11, 2024.
To Cite: Trivedi C, Rizvi A, Ashraf S, et al. Psychiatric comorbidities in hospitalized adolescents with polycystic ovary syndrome: a cross-sectional study using the National Inpatient Sample. Prim Care Companion CNS Disord. 2024;26(6):24m03760.
Author Affiliations: Department of Psychiatry, Texas Tech University, Health Science Center at Odessa/Permian Basin Odessa, Odessa, Texas (Trivedi, Ashraf, Husain, Yadav, Perugula, Nabi, Jain); Department of Psychiatry, Texas Tech University, Health Science Center, Lubbock, Texas (Adams); Department of Psychiatry, West Virginia School of Medicine, Morgan Town, West Virginia (Rizvi); Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut (Mansuri).
Corresponding Author: Chintan Trivedi, MD, MPH, Department of Psychiatry, Texas Tech University Health Science Center, Midland, 2301 W Michigan Ave, Midland, TX 79701 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Routine mental health screenings for psychiatric disorders, specifically mood and anxiety disorders, should be integrated into the care regimen for adolescents with polycystic ovary syndrome (PCOS).
- Effective management of PCOS should involve a multidisciplinary approach that includes addressing psychiatric comorbidities and providing psychological support.
- Enhanced access to care and increased awareness of the psychological impacts of PCOS should be ensured, especially in underserved populations.
References (32)

- Shrivastava S, Conigliaro RL. Polycystic ovarian syndrome. Med Clin North Am. 2023;107(2):227–234. PubMed CrossRef
- Christensen SB, Black MH, Smith N, et al. Prevalence of polycystic ovary syndrome in adolescents. Fertil Steril. 2013;100(2):470–477. PubMed CrossRef
- Hickey M, Doherty DA, Atkinson H, et al. Clinical, ultrasound and biochemical features of polycystic ovary syndrome in adolescents: implications for diagnosis. Hum Reprod. 2011;26(6):1469–1477. PubMed CrossRef
- Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018;14(5):270–284. PubMed CrossRef
- Harada M. Pathophysiology of polycystic ovary syndrome revisited: current understanding and perspectives regarding future research. Reprod Med Biol. 2022;21(1):e12487. PubMed CrossRef
- Teede HJ, Misso ML, Costello MF, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602–1618. PubMed CrossRef
- Witchel SF, Oberfield SE, Peña AS. Polycystic ovary syndrome: pathophysiology, presentation, and treatment with emphasis on adolescent girls. J Endocr Soc. 2019;3(8):1545–1573. PubMed CrossRef
- Deeks AA, Gibson-Helm ME, Teede HJ. Anxiety and depression in polycystic ovary syndrome: a comprehensive investigation. Fertil Steril. 2010;93(7):2421–2423. PubMed CrossRef
- Himelein MJ, Thatcher SS. Polycystic ovary syndrome and mental health: a review. Obstet Gynecol Surv. 2006;61(11):723–732. PubMed CrossRef
- Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:41. PubMed CrossRef
- Månsson M, Holte J, Landin-Wilhelmsen K, et al. Women with polycystic ovary syndrome are often depressed or anxious—a case control study. Psychoneuroendocrinology. 2008;33(8):1132–1138. PubMed
- Bhattacharya SM, Jha A. Prevalence and risk of depressive disorders in women with polycystic ovary syndrome (PCOS). Fertil Steril. 2010;94(1):357–359. PubMed CrossRef
- Cooney LG, Lee I, Sammel MD, et al. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2017;32(5):1075–1091. PubMed CrossRef
- Yadav S, Delau O, Bonner AJ, et al. Direct economic burden of mental health disorders associated with polycystic ovary syndrome: systematic review and meta analysis. ELife. 2023;12:e85338. PubMed CrossRef
- Rodriguez-Paris D, Remlinger-Molenda A, Kurzawa R, et al. Psychiatric disorders in women with polycystic ovary syndrome. Psychiatr Pol. 2019;53(4):955–966. PubMed CrossRef
- Trent ME, Rich M, Austin SB, et al. Quality of life in adolescent girls with polycystic ovary syndrome. Arch Pediatr Adolesc Med. 2002;156(6):556–560. PubMed CrossRef
- Peña AS, Witchel SF, Hoeger KM, et al. Adolescent polycystic ovary syndrome according to the international evidence-based guideline. BMC Med. 2020;18(1):72. PubMed
- HCUP. Healthcare Cost and Utilization Project (HCUP) - National Inpatient Sample. Healthcare Cost and Utilization Project. 2020.
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2020. Accessed September 20, 2022. https://www.R-project.org/
- Jones GL, Hall JM, Balen AH, et al. Health-related quality of life measurement in women with polycystic ovary syndrome: a systematic review. Hum Reprod Update. 2008;14(1):15–25. PubMed CrossRef
- Hollinrake E, Abreu A, Maifeld M, et al. Increased risk of depressive disorders in women with polycystic ovary syndrome. Fertil Steril. 2007;87(6):1369–1376. PubMed CrossRef
- Eggers S, Kirchengast S. The polycystic ovary syndrome–a medical condition but also an important psychosocial problem. Coll Antropol. 2001;25(2):673–685. PubMed
- Jedel E, Gustafson D, Waern M, et al. Sex steroids, insulin sensitivity and sympathetic nerve activity in relation to affective symptoms in women with polycystic ovary syndrome. Psychoneuroendocrinology. 2011;36(10):470–1479. PubMed CrossRef
- Jedel E, Waern M, Gustafson D, et al. Anxiety and depression symptoms in women with polycystic ovary syndrome compared with controls matched for body mass index. Hum Reprod. 2010;25(2):450–456. PubMed CrossRef
- Klimczak D, Szlendak-Sauer K, Radowicki S. Depression in relation to biochemical parameters and age in women with polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol. 2015;184:43–47. PubMed CrossRef
- Annagür BB, Tazegül A, Uguz F, et al. Biological correlates of major depression and generalized anxiety disorder in women with polycystic ovary syndrome. J Psychosom Res. 2013;74(3):244–247. PubMed
- Farrell K, Antoni MH. Insulin resistance, obesity, inflammation, and depression in polycystic ovary syndrome: biobehavioral mechanisms and interventions. Fertil Steril. 2010;94(5):1565–1574. PubMed CrossRef
- Almis H, Orhon FŞ, Bolu S, et al. Self-concept, depression, and anxiety levels of adolescents with polycystic ovary syndrome. J Pediatr Adolesc Gynecol. 2021;34(3):311–316. PubMed CrossRef
- Emeksiz HC, Bideci A, Nalbantoğlu B, et al. Anxiety and depression states of adolescents with polycystic ovary syndrome. Turk J Med Sci. 2018;48(3):531–536. PubMed CrossRef
- Hsu TW, Kao YC, Tsai SJ, et al. Suicide attempts after a diagnosis of polycystic ovary syndrome: a cohort study. Ann Intern Med. 2024;177(3):335–342. PubMed CrossRef
- Brutocao C, Zaiem F, Alsawas M, et al. Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine. 2018;62(2):318–325. PubMed CrossRef
- Karjula S, Arffman RK, Morin-Papunen L, et al. A population-based follow-up study shows high psychosis risk in women with PCOS. Arch Womens Ment Health. 2022;25(2):301–311. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!