ABSTRACT
Objective: To investigate associations between patients with borderline personality disorder (BPD)–related symptoms and their hospital presentations as well as the effect of inpatient length of stay (LOS) on time to hospital re-presentation.
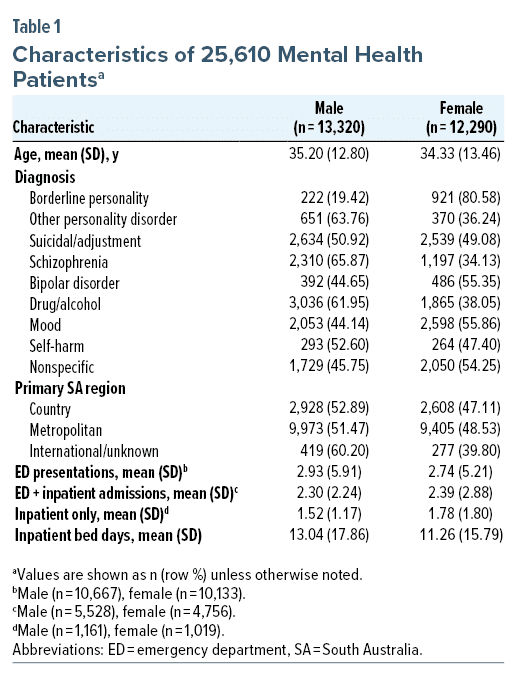
Methods: A retrospective cohort design was used to investigate mental health emergency department (ED) visits and inpatient admissions. The cohort comprised 13,320 men and 12,290 women with a follow-up period between January 1, 2014, and December 31, 2019.
Results: Across all presentations in the study period, approximately 4% of mental health patients were discharged from ED or inpatient admission with primary diagnosis of BPD. Both male and female patients with BPD were at higher risk of hospital re-presentation when compared to patients with any other type of mental disorder (P < .01). Patients with BPD who had LOS > 14 days in their first inpatient admission were, on average, more likely to experience a repeat ED or inpatient presentation 58 days sooner than patients who had LOS < 2 days (P = .036).
Conclusions: Findings suggest the need for (a) more accurate recording of BPD and related presentations, (b) more in-depth investigations of BPD care pathways, and (c) identifications of subpopulations who may benefit from a specific inpatient length of stay.
Prim Care Companion CNS Disord 2024;26(1):23m03559
Author affiliations are listed at the end of this article.
Borderline personality disorder (BPD) is a serious mental illness that is associated with considerable suffering and impairment. Of major concern, the mortality rate associated with BPD is around 3%–6%,1,2 and some studies have reported up to 10%.3,4 BPD patients frequently present with other co-occurring problems, including substance abuse, depression, anxiety, and bipolar affective disorder.5 Furthermore, BPD is associated with considerable psychosocial impairment, including poor social functioning, unemployment, and loss of income.6
Despite the literature suggesting that BPD is associated with significant impacts in terms of health care utilization, there is a paucity of studies exploring these factors in presentations to emergency departments (EDs) and inpatient services, especially in an Australian context. Most of the research in this field is derived from the international literature outside of Australia. For example, a diagnosis of BPD has been linked with frequent ED presentations7,8 and more frequent but shorter psychiatric admissions compared to non-BPD mental health diagnoses.9 Past research has indicated that acute inpatient admission (5 days or less) with structured crisis intervention may benefit BPD patients who are suicidal,10 while longer-term hospital stays may pose a risk of resulting in iatrogenic dependency.11 There has also been reported extensive variability in inpatient durations; for instance, the median length of stay for patients with a diagnosis of BPD within a UK psychiatric inpatient unit was 10 days with range from 1 to 249 days.12
In the Australian context, a recently published (2019) study by Lewis et al13 analyzed hospital admissions for 2,894 people presenting to hospital in NSW and found that patients with a personality disorder represented 20.5% of emergency presentations and 26.6% of inpatient separations. Furthermore, patients diagnosed with a personality disorder were 2.3 times more likely to re-present to hospital within 28 days. However, this study did not include data specific to a diagnosis of BPD. Improving the knowledge of rates of BPD in public health care settings and the potential to predict future re-presentations is important for guiding health care policy and service planning.14
Data acquired from routine hospital data collection represent one possible platform to enable longitudinal health studies, epidemiologic surveillance on mental health problems, and identification of high-risk groups of patients such as frequent presenters to EDs. Therefore, utilizing data from hospital databases in South Australia, the primary aim of this study was to investigate if any significant associations exist between patients with BPD-related presentations and their public hospital presentations. The study also reports on the effect of mental health inpatient length of stay on time to subsequent hospital re-presentation for patients with BPD. The nature of these inquiries opens opportunities to generate hypotheses for development of more comprehensive reviewing of the mental health community’s service needs and ultimately better BPD care pathways.
METHODS
Study Design and Setting
This retrospective cohort study was undertaken in South Australian (SA) metropolitan and country public hospitals to investigate mental health ED visits and inpatient admissions. The Australian Bureau of Statistics estimated that the resident population of South Australia on June 30, 2020, was 1,769,319 people. The study cohort comprised 13,320 men and 12,290 women with a follow-up period between January 1, 2014, and December 31, 2019. The dataset covered patient reporting from 20 public hospitals in metropolitan and regional areas in South Australia Local Health Networks. The study had ethics approval from The Southern Adelaide Clinical Human Research Ethics Committee (SAC HREC), Office for Research reference number 164.18. We used existing, routinely collected hospital data that were non-identifiable (individual identifiers had been permanently removed, and no specific individual could be identified). Individual patient consent was not required for this research purpose.
We accessed deidentified individual patient-level data from SA Health Emergency Department Data Collection (EDDC) in public hospitals. The collection is updated daily and includes all patients who present to a SA public hospital who seek help for a mental health problem. The dataset includes information on patient’s demographic characteristics and International Classification of Diseases (ICD) codes for routine diagnosis by trained mental health professionals on discharge from ED or inpatient admission. South Australia provides these data to the Commonwealth on an annual basis, where the nation’s information is collated and compared to ensure the best mental health care possible for all people needing mental health care. Definitions that are used in the data presented are from the National Health Data Dictionary (National Health Data Committee, 2003).
Diagnostic Groups
Major diagnostic groups were delineated into more specific features to better understand the heterogeneity of risk for repeated hospital presentations. The 9 subgroups consisted of the following: borderline personality disorder—at least 1 diagnosis of borderline personality disorder for an individual patient during time-period studied; personality disorder—at least 1 diagnosis of non-borderline personality disorder within individual patient during time-period studied; self-harm/suicidal ideation/adjustment disorder; schizophrenia/schizotypal/delusional disorders/schizoaffective disorders; bipolar disorder; substance use disorder (SUD); mood/anxiety disorders; suicidal ideation/self-harm—any suicidal ideation/self-harm in remaining non-specific presentations; and non-specific—patients who did not fit best into the main diagnostic groups, for example, those with “other specified behavioral and emotional disorders.” We note that self-harm and suicidal ideation are not diagnostic terms and may in fact include people whose underlying presentation was borderline personality disorder or other psychiatric diagnoses.
Statistical Analysis
All analyses were conducted using Stata, version 16,15 and used 2-tailed hypothesis tests with α = .05. Corresponding with the primary study aim, the analysis sought to investigate recurrent ED and inpatient events per individual across a 6-year follow-up period using mixed-effects parametric survival modeling. This approach accounts for the expectation that risk of presentation will increase with the accumulated number of previous presentations.16
Survival models were stratified by sex to examine separate magnitudes of associations.17 Independent variables for fixed effects were diagnosis (“exposure” variable) and covariate adjusted for sex, age, age-squared (non-linear effects), hospital length of stay (LOS), region (metropolitan versus regional), and hospital journey (ED only versus inpatient stay). Because each patient had an ED presentation or inpatient stay or both, we introduced a random coefficient on the binary variable “hospital event” (0 = ED only; 1 = inpatient admission ± ED) to predict an average effect for individual risk of re-presentation to either an ED or inpatient admission.
We also sought to examine whether a specific length of a patient’s first inpatient stay influenced the average change in time to any subsequent inpatient or ED presentation. Cut-scores were used to classify study patients with BPD or other personality disorder into 1 of 4 LOS groups: 0, < 2 days; 1, 2–7 days; 2, 8–14 days; and 3, > 14 days. To address this exploratory analysis using observational data, LOS effects on time to hospital event were considered in a counterfactual framework. The goal was to mimic randomization of patients to different LOS groups. For multivalued inpatient lengths of stay, estimates were produced for the potential‐outcome means (POMs), and average treatment effects (ATEs) using inverse‐probability–weighted regression adjustment (IPWRA). Covariate selection used only baseline variables for the ATE models and was therefore not impacted by the exposure variable during follow-up. To check for covariate balance over LOS groups after estimation by IPWRA, standardized differences and variance ratios were evaluated.18
RESULTS
Descriptive Statistics
In the study period, there were a total of 86,740 ED and inpatient episodes of care for 25,610 mental health patients. For each patient, a single record comprised of either ED presentation or inpatient admission (± ED presentation). The number of hospital events ending on or before the entry time for risk of onset was 4,147; these were not included in the survival analysis. Eight patients had both male and female recorded as their sex: 5 patients had male sex recorded on at least 67% of occasions were therefore assigned “‘male’”; 3 patients had equal numbers of male and female records and were randomly assigned to either one or the other. The final dataset comprised 13,320 male patients with 43,489 observations and 12,290 female patients with 39,104 observations (Table 1).
Risk Modeling
The application of mixed-effects survival analysis was used to model multiple hospital presentations and account for the underlying risk for individuals to vary across the 6-year follow-up period.
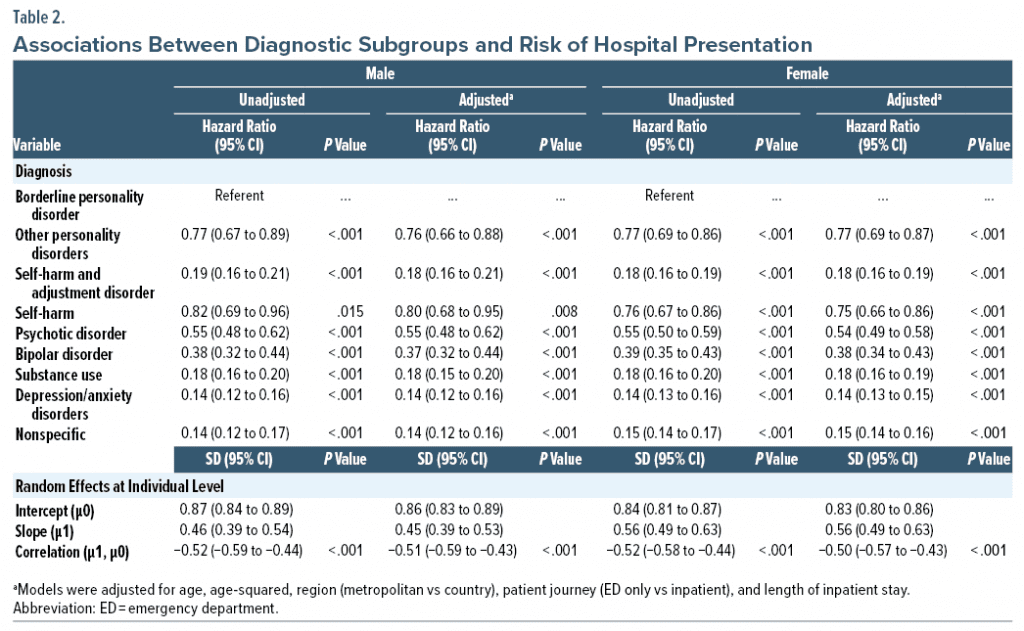
Table 2 provides estimated hazards ratios for diagnostic subgroups after adjusting for covariates. The overall test of diagnosis is significant for both male (χ28 = 3210, P < .001) and female patients (χ28 = 3697.1, P < .001). The BPD group is the referent category. With a hazard ratio less than 1, all non-BPD diagnostic groups are associated with a lower risk of hospital re-presentation when compared to patients with borderline personality disorder. Contrasts were performed to focus on different levels of diagnosis. The first test compared self-harm versus non-BPD personality disorder. This difference was not significantly different for male (P = .457) or female patients (P = .738). The second contrast compared self-harm versus self-harm/adjustment disorder. This difference was significantly different for both male and female patients (P < .001). Those with self-harm had a significantly higher risk of hospital re-presentation than those with self-harm/adjustment disorder.
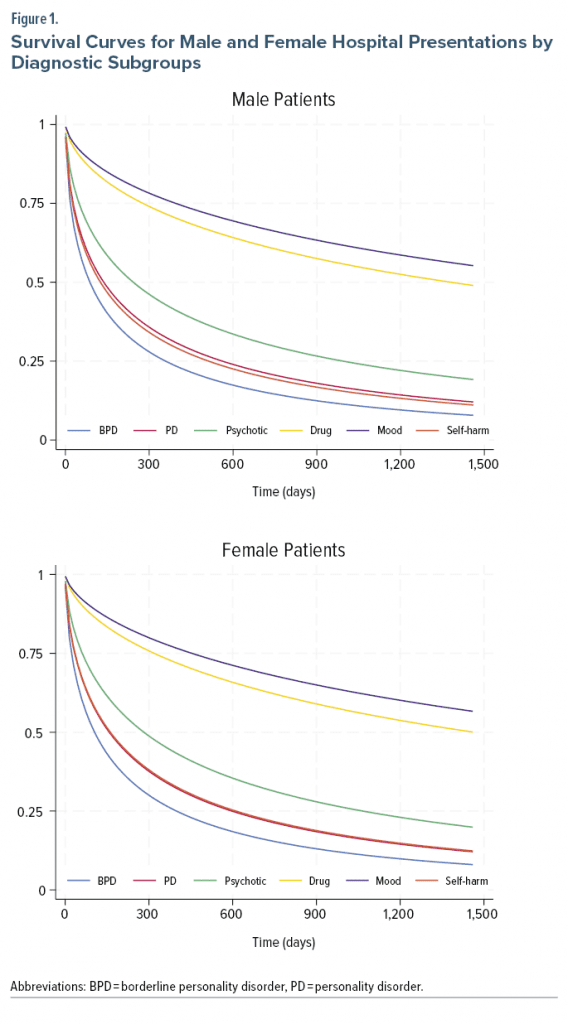
The predictions from the survival models can be visualized using survivor curves as shown in Figure 1. We see that the survivor function for both male and female patients with BPD is below the survivor function for all other diagnostic groups, which means that BPD sufferers have a greater probability of having an episode by study time t (number of days). In contrast, the survivor function for people who presented with mood disorder is above the survivor function for all other diagnoses, which means that these patients have a greater probability of not having an episode by study time t.
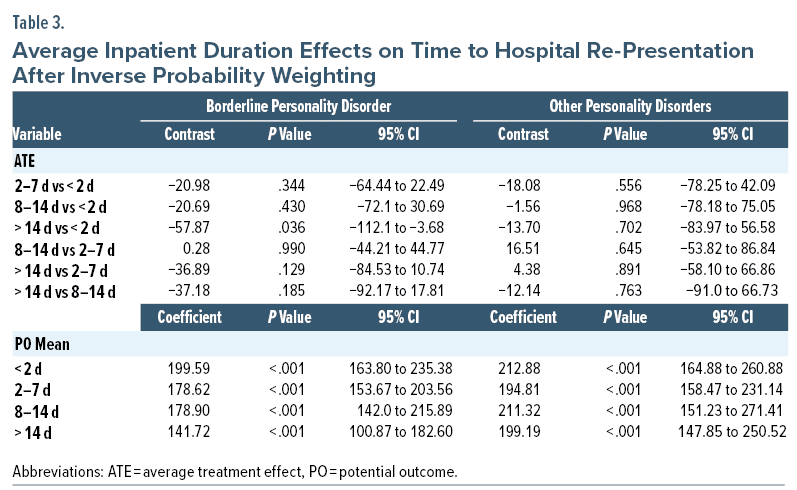
Inpatient Length of Stay
For patients with BPD or other personality disorder, we examined whether their LOS at first inpatient admission (< 2 days, 2–7 days, 8–14 days, 14+ days) influenced the average change in time to a second ED or inpatient presentation, or both. To address observational data, inpatient LOS effects were considered in a counterfactual framework by permitting covariates such as age and sex to be related to the potential outcomes and LOS group. The ATE model findings for study outcome, incorporating the establishment of reasonable covariate balance and meeting the overlap assumption, are presented in Table 3. For BPD patients with LOS < 2 days, the mean time to a second ED and/or inpatient admission was 199 days. The mean time to a second hospital visit was 179 days for LOS groups 2–7 days and 8–14 days. For the heavy user group (14+ days), the mean time to a second hospital presentation was 142 days. The mean time to a second hospital visit was 58 days sooner when all the patients had LOS > 14 days than when all the patients had LOS < 2 days (P = .036). No other contrasts were statistically significant. For patients with other personality disorders, the mean time to a second hospital visit ranged from 199 days to 213 days across groups. There was no statistically significant difference between pairwise comparisons.
DISCUSSION
The current study explored the health service utilization of patients who had received a diagnosis of BPD compared to patients who had received other diagnoses across public hospitals spanning metropolitan and country regions in South Australia. In particular, the study aimed to predict risk of hospital re-presentations for patients with a diagnosis of BPD in comparison to patients with other psychiatric conditions. It was found that, across all presentations in the study period, approximately 4% of mental health patients were discharged from an ED or inpatient admission with a primary diagnosis of BPD. The main findings indicated that patients with BPD were at higher risk of hospital re-presentation when compared to patients with any other type of mental disorder.
We also found that patients diagnosed with self-harm presentations had a significantly higher risk of hospital re-presentation than those with self-harm with adjustment disorder. Adjustment disorder is a condition commonly encountered by clinicians in EDs and liaison psychiatry settings and has been frequently reported among patients presenting with suicidal behaviors. A number of previous studies have also noted the strong association between suicidal ideation and behaviors and adjustment disorder.19 While in this study we focused on Axis I diagnosis, previous research has shown that, for example, almost 40% of patients with primary discharge diagnosis of adjustment disorder had Axis II borderline personality disorder.20 This may to some extent explain the lower numbers of BPD diagnosis in this study (for example, as found by Lewis et al13) and the potential for “underappreciating” or misdiagnosing it as a co-occurring condition in a public hospital.9,21
For inpatient admissions, data from our study suggested that a patient’s initial inpatient length of stay for BPD predicted number of days to subsequent re-presentation. For example, the average time to a second hospital visit was 58 days sooner when patients had a LOS > 14 days than when patients had LOS < 2 days (P = .036). While hospital admissions are not generally recommended as a primary treatment for patients with a diagnosis of BPD, clinical guidelines suggest that an inpatient admission may at times be necessary.22 Also, some people with a diagnosis of BPD may benefit from inpatient treatment, particularly when complex comorbidities are evident.13 However, clinicians are cautious about admission of patients with BPD for longer than 2 days owing to a potentially increased risk of regression, self-harming behavior, and clinical deterioration in such a setting. Previous research has indicated that patients with BPD can experience more frequent admissions than their non-BPD counterparts and are more likely to be admitted in the previous year, but with shorter lengths of stay.9
Limitations
The results should be interpreted in the context of 2 main methodological limitations. First, the findings are limited to a small number of patient characteristics. Other variables such as ethnicity, education levels, social support networks, unemployment, and homelessness may provide further insights into the complex interplay of factors associated with BPD and ED/hospital presentation. Second, the retrospective cohort design means that we are unable to determine causal pathways between patient characteristics and hospital presentations. For example, other risk factors (confounders) may have been present that were not measured. Future research should also investigate the longitudinal trajectories of individual BPD sufferers to test the differential effects of patient characteristics from proximal factors (eg, unexpected job loss) and risk factors further back in the causal chain (distal influences such as social determinants, eg, early childhood experiences and development).
Further limitations include that this study was restricted to one Australian state and may not be generalizable to other contexts. Also, while a great strength of this study was its capacity to capture data from a wide range of public hospitals in both metropolitan and country regions, it did not include private hospital data. In a national study, 16% of Australians with a diagnosis of BPD reported only using private hospital services,23 and therefore the capacity to estimate the full extent of health care service utilization in South Australia is limited.
Implications for Future Research
In a large cohort of mental health patients, the current modeling of multiple records per individual has led to a more thorough understanding of mental health hospital use (ED and inpatient) trajectories. The findings highlight specific diagnostic and symptom subgroups that are at greater risk of hospital re-presentation. However, the findings do not tell us about the care pathways the patients took through those services. For example, the data do not show the potential increased rates of people with features of BPD, including adolescents with early features of BPD in primary care and EDs and whether they receive the right level of care. This type of information could otherwise result in early referral to specialist, specialized, and allied health services for thorough assessment and earlier diagnosis, in turn leading to prompt support and treatment.
The reconfiguration of the patient’s journey in hospital from the patient’s perspective such as through process mapping would allow clinicians and managers to “see” and understand patients’ experience by separating the management of a specific psychiatric condition and treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example).24 This approach would also need to address BPD-related questions about sex and gender, such as how do sex and gender intersect with age, race and ethnicity, and other sociocultural factors as well as determine outcomes.25 The synthesis of this type of information with data such as from the current study would provide deeper insights into patient journeys, including when things went right and when they did not. Of particular interest is the association between initial inpatient length of stay and subsequent readmissions. A more detailed pathway analysis could determine factors that predicted whether, for BPD, any overnight stay and stays of less or greater than 2 days were associated with harm or benefit.
Article Information
Published Online: January 9, 2024. https://doi.org/10.4088/PCC.23m03559
© 2024 Physicians Postgraduate Press, Inc.
Submitted: May 5, 2023; accepted August 17, 2023.
To Cite: Smith D, Cammell P, Battersby M, et al. Recurrent mental health presentations to public hospital services: a focus on borderline personality disorder. Prim Care Companion CNS Disord. 2024;26(1):23m03559
Author Affiliations: College of Medicine and Public Health, Flinders University, Adelaide, South Australia, Australia (Smith, Battersby, Stevenson, Bastiampillai); Royal Melbourne Hospital Head of Psychotherapy Training, St Vincent’s Health, Melbourne, Victoria, Australia (Cammell); Southern Adelaide Local Health Network, Mental Health Division, Adelaide, South Australia, Australia (Battersby, Bastiampillai); School of Psychology, University of Adelaide, Adelaide, South Australia, Australia (Bartsch).
Corresponding Author: David Smith, BSc, MNurs, MAppStat, PhD, Senior Researcher, Discipline of Psychiatry, College of Medicine and Public Health, Flinders University, GPO Box 2100, ADELAIDE SA 5001, Australia ([email protected]).
Author Contributions: Conceptualization: Smith, Cammell, Battersby, Bartsch, Stevenson, Bastiampillai; methodology: Smith, Cammell, Bastiampillai; formal analysis and investigation: Smith, Stevenson; writing—original draft preparation: Smith, Cammell, Battersby, Bartsch, Bastiampillai; writing—manuscript editing: Smith, Cammell, Battersby, Bartsch, Stevenson, Bastiampillai. All authors read and approved the final manuscript.
Relevant Financial Relationships: The authors have no conflicts of interest or competing interests to declare.
Funding/Support: Research reported in this publication was commissioned by the South Australian Borderline Personality Disorder Collaborative (contract number: SAH2019-1146) through funding received from the Barossa Hills Fleurieu Local Health Network. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the South Australian Borderline Personality Disorder Collaborative or the Barossa Hills Fleurieu Local Health Network.
Role of the Funders/Sponsors: The funder had no oversight on study data analysis and interpretation.
Data Availability: The dataset analyzed during the current study are not publicly available due to lack of participant informed consent and ethics approval to deposit the data in a public repository but are available from the corresponding author on reasonable request.
Clinical Points
- Patients with borderline personality disorder were at higher risk of hospital re-presentation when compared to patients with any other type of mental disorder.
- The mean time to a second hospital visit was 58 days sooner for patients with a length of stay (LOS) > 14 days for the initial hospital visit than for patients with LOS < 2 days.
References (25)

- Paris J, Zweig-Frank H. A 27-year follow-up of borderline patients. Compr Psychiatry. 2001;42:482–487. PubMed CrossRef
- Stone MH. The Fate of Borderline Patients: Successful Outcome and Psychiatric Practice. Guilford Press; 1990.
- Gunderson JG, Stout RL, McGlashan TH, et al. Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Arch Gen Psychiatry. 2011;68(8):827–837. PubMed CrossRef
- Temes CM, Frankenburg FR, Fitzmaurice GM, et al. Deaths by suicide and other causes among patients with borderline personality disorder and personality-disordered comparison subjects over 24 years of prospective follow-up. J Clin Psychiatry. 2019;80(1):18m12436. PubMed CrossRef
- Zanarini MC, Frankenburg FR, Dubo ED, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155(12):1733–1739. PubMed CrossRef
- Ansell EB, Sanislow CA, McGlashan TH, et al. Psychosocial impairment and treatment utilization by patients with borderline personality disorder, other personality disorders, mood and anxiety disorders, and a healthy comparison group. Compr Psychiatry. 2007;48(4):329–336. PubMed CrossRef
- Pascual JC, Córcoles D, Castaño J, et al. Hospitalization and pharmacotherapy for borderline personality disorder in a psychiatric emergency service. Psychiatr Serv. 2007;58(9):1199–1204. PubMed CrossRef
- Vandyk AD, VanDenKerkhof EG, Graham ID, et al. Profiling frequent presenters to the emergency department for mental health complaints: socio-demographic, clinical, and service use characteristics. Arch Psychiatr Nurs. 2014;28(6):420–425. PubMed CrossRef
- Leontieva L, Gregory R. Characteristics of patients with borderline personality disorder in a state psychiatric hospital. J Pers Disord. 2013;27(2):222–232. PubMed CrossRef
- Berrino A, Ohlendorf P, Duriaux S, et al. Crisis intervention at the general hospital: an appropriate treatment choice for acutely suicidal borderline patients. Psychiatry Res. 2011;186(2–3):287–292. PubMed CrossRef
- National Collaborating Centre for Mental Health (UK). Borderline personality disorder: treatment and management. NICE Clinical Guidelines. 2009;(78):1854334778.
- Shoka A, Lazzari C, Gower K. Length of admission into psychiatric hospitals according to diagnoses. Eur Psychiatry. 2017;41(S1):S250. CrossRef
- Lewis KL, Fanaian M, Kotze B, et al. Mental health presentations to acute psychiatric services: 3-year study of prevalence and readmission risk for personality disorders compared with psychotic, affective, substance or other disorders. BJPsych Open. 2019;5(1):e1. PubMed CrossRef
- Chen S, Kong N, Sun X, et al. Claims data-driven modeling of hospital time-to-readmission risk with latent heterogeneity. Health Care Manage Sci. 2019;22(1):156–179. PubMed CrossRef
- Stata Statistical Software. Release 16.1. StataCorp LLC; 2019.
- Westbury LD, Syddall HE, Simmonds SJ, et al. Identification of risk factors for hospital admission using multiple-failure survival models: a toolkit for researchers. BMC Med Res Methodol. 2016;16(1):46. PubMed CrossRef
- Clayton JA, Tannenbaum C. Reporting sex, gender, or both in clinical research? JAMA. 2016;316(18):1863–1864. PubMed CrossRef
- Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. PubMed CrossRef
- Fegan J, Doherty AM. Adjustment disorder and suicidal behaviours presenting in the general medical setting: a systematic review. Int J Environ Res Public Health. 2019;16(16):2967. PubMed CrossRef
- Kryzhanovskaya L, Canterbury R. Suicidal behavior in patients with adjustment disorders. Crisis. 2001;22(3):125–131. PubMed CrossRef
- Gregory R, Sperry SD, Williamson D, et al. High prevalence of borderline personality disorder among psychiatric inpatients admitted for suicidality. J Pers Disord. 2021;35(5):776–787. PubMed CrossRef
- National Health and Medical Research Council. Clinical Practice Guideline for the Management of Borderline Personality Disorder 2012. https://www.nhmrc.gov.au/about-us/publications/clinical-practice-guideline-borderline-personality-disorder
- Lawn S, McMahon J. Experiences of care by Australians with a diagnosis of borderline personality disorder. J Psychiatr Ment Health Nurs. 2015;22(7):510–521. PubMed CrossRef
- Trebble TM, Hansi N, Hydes T, et al. Process mapping the patient journey: an introduction. BMJ. 2010;341(aug13 1):c4078. PubMed CrossRef
- Stefanick ML, Schiebinger L. Analysing how sex and gender interact. Lancet. 2020;396(10262):1553–1554. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!