Objective: The present study examined the efficacy, safety, and durability of repeated ketamine infusions for the treatment of comorbid posttraumatic stress disorder (PTSD) and treatment-resistant depression (TRD) in a sample of veterans.
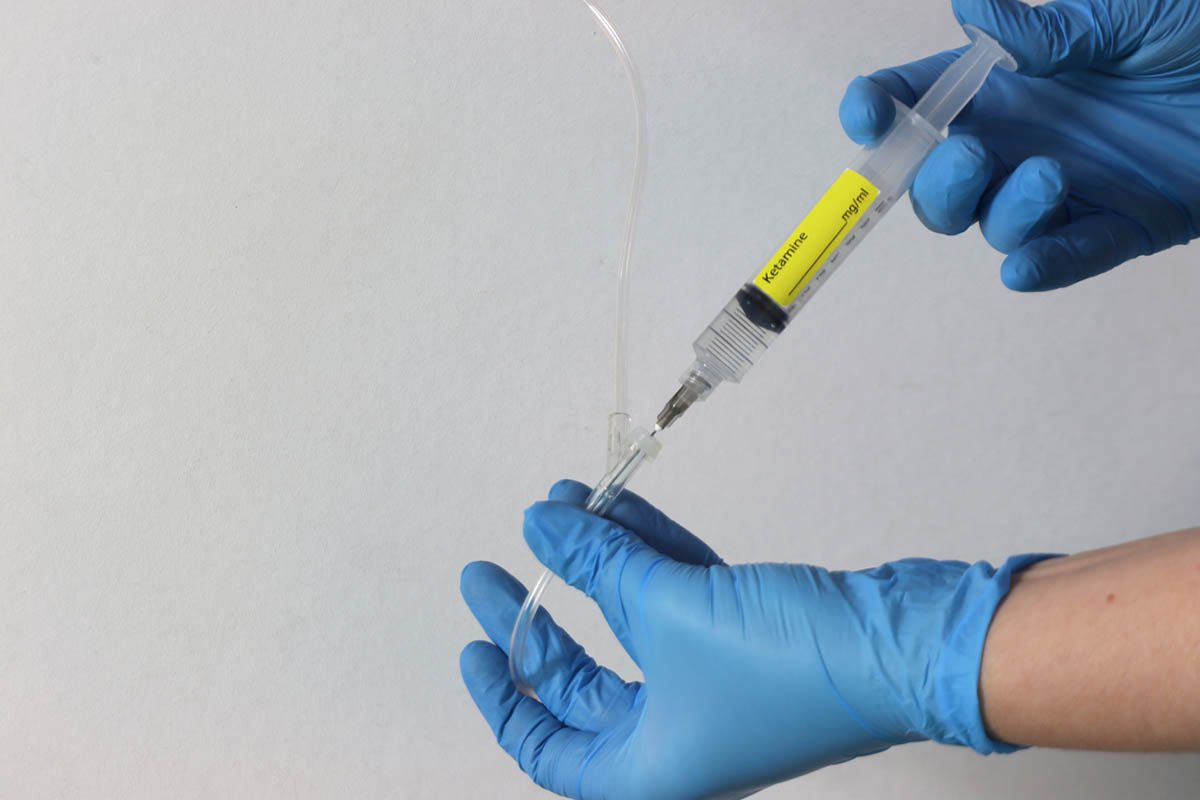
Methods: Individuals with comorbid DSM-5-defined PTSD and DSM-IV-defined major depressive disorder (N = 15) received 6 intravenous ketamine infusions (0.5 mg/kg) on a Monday-Wednesday-Friday schedule over a 12-day period from May 2015 to June 2016. Data from outcome measures were collected before and 24 hours after each infusion and weekly for 8 weeks following the final infusion.
Results: Continuous measures of symptom change were significant for both disorders and were associated with large effect sizes (mean decrease in PTSD Checklist for DSM-5 score = 33.3 points [95% CI, 23.0-43.5 points], P < .0005, sample size-adjusted Cohen d [d’ ²] = 2.17; mean decrease in Montgomery-Asberg Depression Rating Scale score = 26.6 points [95% CI, 23.0-30.2 points], P < .0005, d’ ² = 4.64). The remission rate for PTSD was 80.0%, and the response rate for TRD was 93.3%. Participants in remission from PTSD after the infusion series (n = 12) had a median time to relapse of 41 days. Similarly, participants whose depression symptoms responded to the infusion series (n = 14) had a median time to relapse of 20 days. Repeated ketamine infusions were associated with transient increases in dissociative symptoms. No participant reported worsening of PTSD symptoms over the study duration.
Conclusions: This study, the first open-label study of repeated ketamine infusions in a comorbid population, found rapid and sustained improvement in PTSD and depression symptoms. This report suggests that repeated ketamine treatments are safe and may represent an efficacious treatment for individuals with comorbid PTSD and TRD.
Trial Registration: ClinicalTrials.gov identifier: NCT02577250
Members Only Content
This full article is available exclusively to Professional tier members. Subscribe now to unlock the HTML version and gain unlimited access to our entire library plus all PDFs. If you're already a subscriber, please log in below to continue reading.
Please sign in or purchase this PDF for $40.00.
Already a member? Login