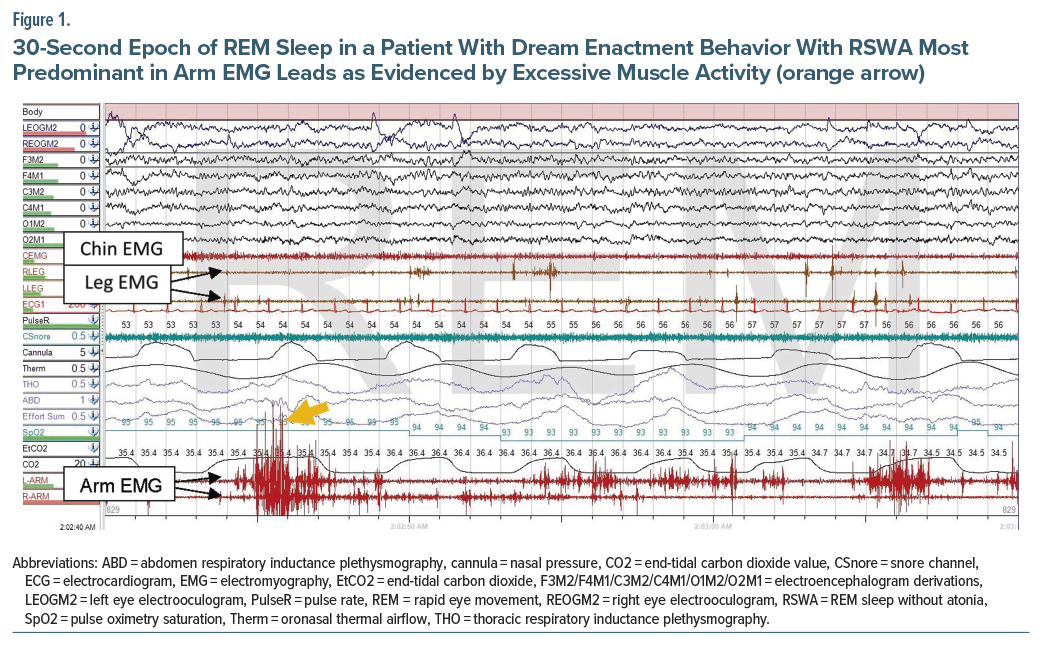
Rapid eye movement (REM) sleep behavior disorder (RBD) is a parasomnia, wherein affected individuals experience dream enactment while in REM sleep. Skeletal muscle atonia normally occurs in REM but is lost in patients with RBD. Diagnosis of RBD is made by dream enactment and REM sleep without atonia (RSWA) on polysomnography (PSG). A standard PSG typically includes the anterior tibialis and chin electromyography (EMG) leads. The use of arm leads is not standard and, in most centers, must specifically be requested. This case highlights the importance of adding arm EMG leads.
Case Report
A 73-year-old man with hypertension, coronary artery disease, and recent diagnosis of benign essential tremor by neurology presented to the sleep clinic for concern of obstructive sleep apnea (OSA). On initial presentation, he reported “night terrors,” which he described as episodes of dream enactment as well as poor short-term memory and an action tremor. His medications included metoprolol but no antidepressants. The dream enactment started prior to beta-blocker use. His examination was notable for right cogwheel rigidity, mildly slow serial finger tapping and rapid alternating movements, and mild dysphonia.
A PSG was ordered, which was negative for OSA with an apnea-hypopnea index of 4.3/hour and oxygen nadir of 90%. He had 73 minutes of REM sleep, accounting for 19.5% of total sleep. As shown in Figure 1, RSWA was present and seen predominantly with arm (flexor digitorum superficialis) EMG. The RSWA index (% of REM sleep epochs meeting criteria for RSWA) using the leg (anterior tibialis) and chin EMG was only 5%, which may not be considered clinically significant. However, the RSWA index with the addition of arm EMG increased the RSWA index to 64%.
Given the findings of RSWA along with his reports of dream enactment, the patient was diagnosed with RBD. Parasomnia safety precautions were reviewed. Due to past serious injury with RBD episodes and concern for additional injuries, the patient was started on melatonin. In the context of the clinical examination findings, RBD, and tremor (which may have been initially misdiagnosed as an essential tremor), the concern for an underlying α-synucleinopathy was discussed.
Discussion
The presence of RSWA on PSG with dream enactment is the hallmark feature of RBD.1 RSWA requires the presence of increased tonic or phasic muscle activity within a 30-second REM epoch.2 While leg EMG is a standard part of routine PSG, arm EMG is not performed routinely and often needs to be specifically requested. As demonstrated in this patient, the addition of arm EMG increases the chance of observing RSWA and can be of strong importance to solidify the diagnosis of RBD. The Sleep Innsbruck Barcelona (SINBAR) group evaluated which of 13 muscles showed the highest rates of phasic RSWA in 17 patients with RBD.3 The mentalis showed the highest rate of phasic EMG activity, but alone only detected an average of 41% of all mini-epochs with phasic activity. Flexor digitorum superficialis EMG showed the second highest rate of detection at 29%. Anterior tibialis EMG detected RSWA in approximately 17% of mini-epochs.
Groups of 3 muscles were evaluated, with the highest rate of RSWA detection being when mentalis, flexor digitorum superficialis, and extensor digitorum brevis were combined, with 82% of all mini-epochs with phasic activity detected.4 The SINBAR group reported in a later study that 94.4% of motor and vocal manifestations were detected with this 3-muscle EMG combination.3
RBD is strongly associated with α-synucleinopathies, which include dementia with Lewy bodies, Parkinson disease, and multiple system atrophy.5 RBD often precedes the development of these conditions by a median time of 11 years.5 The presence of RBD can aid in the diagnosis of an α-synucleinopathy, such that the presence of RSWA can be helpful when the diagnosis of an α-synucleinopathy is in question.
Our case highlights RBD as a possible early feature of an α-synucleinopathy, particularly Parkinson disease.6 At autopsy, 94% of patients with RBD have evidence of an α-synucleinopathy.7 α-synuclein deposits in an ascending fashion within various regions of the brain, with the locus coeruleus being impacted prior to the substantia nigra.8 In both human imaging studies and animal models, the locus coeruleus/subcoeruleus complex was found to play a role in inhibiting muscle tone during typical REM sleep, which is lost in RBD.9 This part of the brain stem is susceptible to damage in individuals with Parkinson disease.9
RBD is often underdiagnosed and carries significant diagnostic delay.10 These factors underscore the importance of routinely screening for and treating parasomnias among patients with α-synucleinopathies as well as assessing people with RBD for signs and symptoms of α-synucleinopathies.
Article Information
Published Online: February 17, 2026. https://doi.org/10.4088/PCC.25cr04089
© 2026 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2026;28(1):25cr04089
Submitted: September 20, 2025; accepted November 10, 2025.
To Cite: Das JA, Johal A, Stahl SM. Importance of utilization of arm electromyography leads for the detection of rapid eye movement sleep without atonia. Prim Care Companion CNS Disord 2026;28(1):25cr04089.
Author Affiliations: Department of Medicine, Western Reserve Hospital, Cuyahoga Falls, Ohio (Das); Department of Family Medicine, Indiana University School of Medicine, Indianapolis, Indiana (Johal); Division of Pulmonary, Critical Care, Sleep and Occupational Medicine, Department of Medicine, Indiana University School of Medicine, Indianapolis, Indiana (Stahl); Department of Neurology, Indiana University School of Medicine, Indianapolis, Indiana (Stahl).
Corresponding Author: John A. Das, MD, Department of Medicine Western Reserve, Hospital 1900 23rd St, Cuyahoga Falls, OH 44223 ([email protected]).
Financial Disclosure: None.
Funding/Support: None.
References (10)

- International Classification of Sleep Disorders. American Academy of Sleep Medicine; 2014.
- Berry R, Quan S, Abreu A. The AASM Manual for the Scoring of Sleep and Associated Events Rules, Terminology and Technical Specifications. American Academy of Sleep Medicine; 2020.
- Frauscher B, Iranzo A, Gaig C, et al. Normative EMG values during REM sleep for the diagnosis of REM sleep behavior disorder. Sleep. 2012;35(6):835–847. PubMed CrossRef
- Fernández-Arcos A, Iranzo A, Serradell M, et al. Diagnostic value of isolated mentalis versus mentalis plus upper limb electromyography in idiopathic REM sleep behavior disorder patients eventually developing a neurodegenerative syndrome. Sleep. 2017;40(4).
- Iranzo A, Fernández-Arcos A, Tolosa E, et al. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PloS One. 2014;9(2):e89741. PubMed CrossRef
- Zhang X, Molsberry SA, Pavlova M, et al. Association of sleepwalking and REM sleep behavior disorder with Parkinson disease in men. JAMA Netw Open. 2021;4(4):e215713. PubMed CrossRef
- Boeve BF, Silber MH, Ferman TJ, et al. Clinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorder. Sleep Med. 2013;14(8):754–762. PubMed CrossRef
- Boeve BF, Saper CB. REM sleep behavior disorder: a possible early marker for synucleinopathies. Neurology. 2006;66(6):796–797. PubMed CrossRef
- García-Lorenzo D, Longo-Dos Santos C, Ewenczyk C, et al. The coeruleus/subcoeruleus complex in rapid eye movement sleep behaviour disorders in Parkinson’s disease. Brain. 2013;136(7):2120–2129. PubMed CrossRef
- Rolinski M, Szewczyk-Krolikowski K, Tomlinson PR, et al. REM sleep behaviour disorder is associated with worse quality of life and other non-motor features in early Parkinson’s disease. J Neurology, Neurosurg Psychiatry. 2013;85(5):560–566. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!