Chorea, with its swift, aimless jerks from deep-brain irregularities, is often linked to Huntington disease but can also arise from various conditions, including arteriovenous malformations (AVMs).1 AVMs typically cause seizures or headaches; chorea is a rarer presentation.2 However, chronic chorea’s impact extends beyond motor issues, with research linking basal ganglia problems to depression.3 The unpredictable nature of chorea can significantly affect mental well-being, increasing the risk of depression.4 We present a rare case of persistent hemichorea from an AVM where syndromal depression emerged, likely due to the ongoing, disabling movements, significantly impacting the patient’s life and causing distress. This infrequent presentation highlights the need to recognize and manage psychiatric comorbidities like depression in movement disorders from structural brain lesions such as AVMs.
Case Report
A 30-year-old unmarried man presented with a 12-year history of rapid, involuntary jerky movements on his right side, exacerbated by stress and absent during sleep. He also reported several years of untreated low mood, hopelessness, poor concentration, anhedonia, fatigue, and insomnia. For 12 years, he relied on faith healing without relief. One month prior to presentation, the movements worsened, occurring every 2–3 minutes, significantly impairing his socio-occupational functioning and self-confidence, prompting him to seek medical help. Initially, in neurology, he was started on tablet tetrabenazine 25 mg 3 times/d. Twenty days later, movements extended to his left side, described as starting with right-hand sensory symptoms, progressing proximally, and culminating in a jerk overflowing to the left neck and upper limb. He was then referred to the psychiatry department.
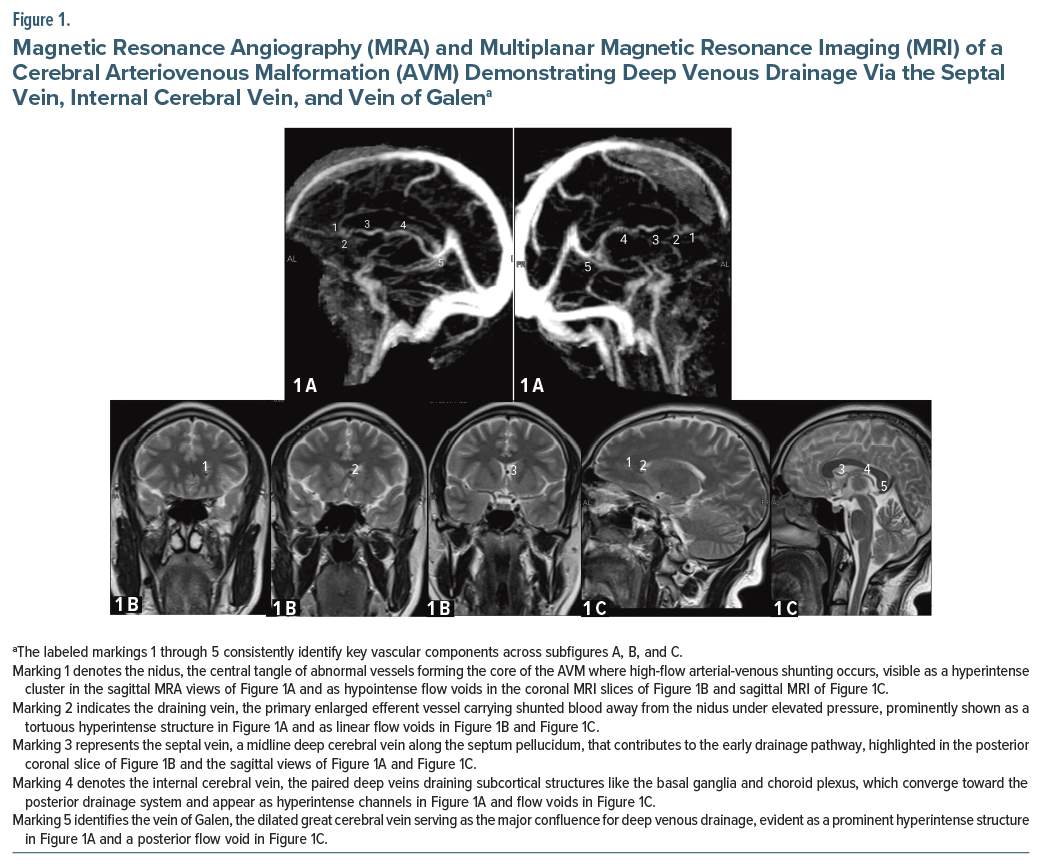
The patient had no vascular risk factors or family history of movement disorders. General physical examination was normal. Neurological examination revealed bilateral choreiform movements (predominantly right) and neck involvement, with normal cognitive function, strength, sensation, and cerebellar function. Pathological reflexes were absent. All blood investigations (complete blood count, liver function test, kidney function test, thyroid, homocysteine), electroencephalogram, and abdominal ultrasound were within normal limits. Brain magnetic resonance imaging with magnetic resonance venography suggested a small AVM (Figure 1); cerebral digital subtraction angiography was deferred due to cost. His initial Abnormal Involuntary Movement Scale (AIMS)5 score was 24, and his Montgomery-Asberg Depression Rating Scale (MADRS)6 score was 25 (moderate depression). Treatment included desvenlafaxine 25 mg once/d, haloperidol 0.25 mg twice/d, and tetrabenazine 25 mg 4 times/d. At 10-day follow-up, significant improvement in movements and mood was noted. After 6 weeks, AIMS and MADRS scores were both 12, confirming overall improvement.
Discussion
While AVMs typically cause intracranial hemorrhage, seizures, or headaches, they infrequently present with choreiform movements.2 AVMs are often congenital but may manifest later, commonly in the third or fourth decade.2 The Spetzler-Martin classification guides AVM treatment strategies.1,2 Reports of AVM-induced chorea are few, and depression secondary to chorea is, to our knowledge, undocumented. Our case involved an AVM near the contralateral caudate nucleus, complicated by depression likely secondary to chorea. Combination therapy with tetrabenazine, desvenlafaxine, and haloperidol significantly improved both chorea and mood, unlike tetrabenazine monotherapy.3
The basal ganglia, including the caudate nucleus, are crucial for motor control; disruption can cause chorea. Mechanisms for AVM-induced chorea are not fully elucidated but may involve disrupted inhibitory pathways or the “steal” phenomenon, where abnormal blood flow through the AVM diverts blood from surrounding brain tissue, leading to ischemia and dysfunction in adjacent areas such as the caudate nucleus.1 In our patient, the AVM’s proximity to the caudate nucleus likely caused his hemichorea, which generalized. Comorbid depression, likely from chronic chorea, requires holistic assessment, as addressing it psychiatrically proved vital for this patient’s improvement. The patient’s initial reliance on faith healing highlights the importance of psychoeducation. In conclusion, this report details a rare case of AVM-induced chorea complicated by secondary depression, emphasizing comprehensive neurological and psychiatric treatment. Recognizing depression in chronic movement disorders from brain lesions like AVMs is crucial for better outcomes. Further research on this interplay is needed
Article Information
Published Online: December 4, 2025. https://doi.org/10.4088/PCC.25cr03999
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(6):25cr03999
Submitted: May 11, 2025; accepted July 24, 2025.
To Cite: Jain A, Garg S, Sharma R. Neurological and psychiatric manifestations of cerebral arteriovenous malformation: a case of hemichorea and depression. Prim Care Companion CNS Disord 2025;27(6):25cr03999
Author Affiliations:Department of Psychiatry, Shri Guru Ram Rai Institute of Medical and Health Sciences, Shri Guru Ram Rai University, Dehradun, Uttarakhand, India (Jain, Garg); Department of Neurology, Shri Guru Ram Rai Institute of Medical and Health Sciences, Shri Guru Ram Rai University, Dehradun, Uttarakhand, India (Sharma).
Corresponding Author: Shobit Garg, MD, DPM, Department of Psychiatry, Shri Guru Ram Rai Institute of Medical and Health Sciences, Shri Guru Ram Rai University, Dehradun, Uttarakhand, 248001, India ([email protected])
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect patient anonymity.
References (6)

- Jurinović P, Jadrijević E, Repić-Buličić A, et al. Chorea caused by unruptured arteriovenous malformation:case report and review of literature. Acta Clin Croat. 2017;56(3):561–565. PubMed
- Bokhari MR, Bokhari SRA. Arteriovenous malformation of the brain. In: StatPearls [Internet]. StatPearls Publishing; 2025. Accessed May 1, 2025. https://www.ncbi.nlm.nih.gov/books/NBK430744/
- Azizi H, Kilpatrick A, Olayinka O, et al. On neuropsychiatric manifestations of basal ganglia injury: a report of three cases and literature review. Case Rep Neurol Med. 2019;2019:3298791. PubMed CrossRef
- Gibson JS, Springer K. Social withdrawal in Huntington’s disease:a scoping review. J Huntingtons Dis. 2022;11(1):17–24. PubMed CrossRef
- Guy W. Abnormal Involuntary Movement Scale (AIMS). ECDEU Assess Man Psychopharmacol. 1976;338:534–537.
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!