Abstract
Objective: To test the effectiveness of a psychotherapeutic strategy—the want/ can/must (WCM) strategy—to mediate conflicts. This intervention aimed to (1) facilitate the collection and sharing of information among the individuals involved and with therapists; (2) comprehend what each person wants, can, and must do; (3) alleviate psychological distress associated with decision-making and action implementation; and (4) minimize harm to all parties involved in the conflict.
Methods: Thirty adult subjects experiencing a conflict situation participated in 8 cognitive-behavioral therapy sessions: 3 sessions for assessment and therapeutic bond building and 5 sessions to implement the WCM strategy. Depressive, anxious, and stress symptoms were assessed and compared before and after the intervention.
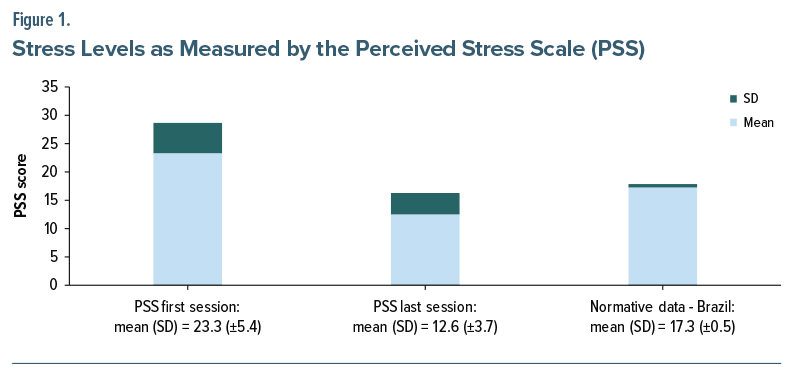
Results: Depending on client and contextual factors, employing the WCM strategy, it was possible to apply techniques that promote cognitive restructuring, psychological acceptance, defusion, and impulse control and that foster compassion and self-compassion, enhance empathetic connection, foster mindfulness in social interactions, and facilitate assertive communication. There was a statistically significant decrease in Perceived Stress Scale scores (P ≤ .05).
Conclusion: All participants reported that the WCM strategy aided in comprehending conflict variables, identifying how to collect information, sharing information about the conflict, accepting that there would be no “perfect solution,” and making a decision with the intention of minimizing harm to those involved in the conflict.
Prim Care Companion CNS Disord 2025;27(3):24m03895
Author affiliations are listed at the end of this article.
Problem and conflict are terms that have similar definitions, sounds, and respective meanings in several official languages of Western countries, including English, Spanish, Portuguese, German, Italian, and French. Although many people use these 2 words synonymously, the meanings are different. We consider that it is important to distinguish between what is a problem and what is a conflict to understand the relevance of this study for clinical practice. In this study, we considered a problem as a difficult-to-solve situation affecting some aspect of an individual’s life; a conflict was considered a disagreement/divergence of ideas, values, and expectations involving 2 or more parties.1
Problem-solving techniques have proved effective in addressing several complaints and improving disorders, especially when they are included together with other strategies in protocols2–4; however, they do not seem to be sufficient to help clients deal with conflict situations. Using the cognitive-behavioral approach and considering what problem-solving therapy proposes, it is clear that the problem-solving steps focus on rational logic and an individual’s perspective to try to repair or reduce harm.5
Experimental studies of cognitive-behavioral therapy (CBT) do not present a specific strategy to mediate conflicts. CBT guidebooks do not explain how to provide training regarding how to properly handle conflict situations that clients may be experiencing.5 Even considering that psychotherapy clients present different cultural, religious, ethnic, and social aspects, it is common for them to present conflict situations in therapy sessions. Faced with the need to understand and mediate a conflict, several therapeutic skills are necessary.
Considering the promising perspective of process based psychotherapy, we believe it is possible to enhance the training of cognitive-behavioral therapists to assist clients in mediating conflicts. To achieve this, several existing therapeutic tools, proven effective in addressing various psychological issues, can be utilized.4
The purpose of this study was to test the effectiveness of a psychotherapeutic strategy, the want/can/must (WCM) or, in Portuguese, quero/posso/devo (QPD) strategy. This intervention aimed to (1) facilitate the collection and sharing of information among the individuals involved and with therapists; (2) comprehend what each person wants, can, and must do; (3) alleviate psychological distress associated with decision-making and action implementation; and (4) minimize harm to all parties involved in the conflict.
METHODS
Design and Ethical Considerations
This study proposes a novel strategy that aims to alleviate suffering caused by conflict, in which the psychotherapist, a specialist in CBT, acts as a facilitator, guiding the following processes: (1) collecting, organizing, and sharing information and (2) fostering reflection and more empathetic/assertive communication among the involved parties.
The WCM strategy draws inspiration from Plato’s reflections in “The Republic,” where he divided the human soul into 3 parts: (1) epithymetikon (appetite or desire): our impulses and desires, driven by the immediate pursuit of pleasure or relief from discomfort; (2) logistikon (reason): a sense of self and reality that enables us to understand who we are, what the world is like, and the limitations presented; and (3) thymoeides (spirit): a sense of justice, where anger, aggression, and strength prevail.
Permission was obtained for this experimental study by our local ethics committee (Comitê de Ética em Pesquisa do Instituto de Psiquiatria da Universidade Federal do Rio de Janeiro—CEP-IPUB/UFRJ – CAAE 59683422.4.0000.5263), which complied with the principles of the Declaration of Helsinki. We would like to have included a control group in this experimental research; however, we recognize that it would be unethical because there would be no intervention available to alleviate the distress experienced by participants. Given that no other psychotherapeutic strategy has demonstrated proven effectiveness in mediating conflicts, we assert that relying solely on problem solving techniques would be insufficient for addressing conflict situations. Additionally, opting for no intervention in the control group, such as providing only empathetic listening to participants experiencing conflict, could potentially worsen their suffering.
Participants, Inclusion Criteria, and Exclusion Criteria
Adult patients aged between 18 and 60 years who were experiencing a conflict situation were recruited. Individuals who did not meet the diagnostic criteria for any disorder or those meeting the diagnostic criteria for mood disorders (without psychotic symptoms), anxiety disorders, or stress-related disorders were included. Only participants who had never undergone CBT and who were not receiving any psychotherapeutic treatment during their participation in this study were accepted.
People with intellectual disabilities, schizophrenia, personality disorders, and habit and impulse disorders were excluded from this research. They were directed to visit other mental health treatment centers where they could receive more appropriate treatment. None of the following variables were considered as part of exclusion criteria: sex, gender, sexual orientation, ethnicity, race, religion or creed, education level, or economic situation.
Instruments
The Structured Clinical Interview for the DSM-5 (SCID-5) is a semistructured interview guide for making major DSM-5 diagnoses according to the diagnostic criteria published in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM).6
The Beck Depression Inventory-II (BDI-II) is a 21-item questionnaire that evaluates a variety of symptoms of depression on a scale from 0 to 3 during the last 7 days. Scores range from 0 to 63, with higher values signifying higher levels of depressive symptoms.7
The Beck Anxiety Inventory (BAI) consists of 21 self-reported items (scale from 0 to 3) used to assess the intensity of physical and cognitive anxiety symptoms during the past week. Scores range from 0 to 63. In this case, the higher the score, the greater the suffering from symptoms of anxiety.8
The Perceived Stress Scale (PSS-10) is a 10-item questionnaire used to assess stress levels. Scores range from 0 to 40. The final score is obtained by simple summation; however, the scores for items 4, 5, 7, and 8 must be reversed (eg, 0 = 4, 1 = 3, 2 = 2, 3 = 1, and 4 = 0).9
The questionnaire used to investigate the effectiveness of the WCM strategy was developed by the authors of this research.
Statistical Analysis
The statistical analysis was conducted using SPSS for Windows, Version 28 (SPSS Inc, Chicago, Illinois) to compare, correlate, and analyze the included scores. A paired t-test was employed to compare scores before and after the experimental intervention. The level of significance was defined as P ≤ .05.
Research Procedures
Psychotherapists, certified as specialists in CBT with more than 5 years of clinical experience, received 4 hours of training to understand how to apply the WCM strategy. Participants signed an informed consent form stating that they voluntarily agreed to participate in this research, which aimed to test the therapeutic efficacy of the WCM in conflict mediation. Then, an assessment interview was conducted using the SCID-5. If the inclusion criteria were met, the BDI, BAI, and PSS were applied in the first session. After 3 sessions to evaluate, develop a case conceptualization, and establish a good therapeutic relationship, the WCM strategy was applied in 5 sessions.
WCM Strategy for Conflict Mediation
The first 3 assessment sessions are crucial for establishing a good therapeutic bond with mutual trust, respect, and empathy. In this initial phase, the therapist seeks to understand the patient’s problem by gathering detailed information about their thoughts, feelings, and behaviors.
In the first session, through open-ended questions and active listening, the therapist creates a safe environment for the patient to express themselves freely. Techniques like the downward arrow can help identify deeper-rooted beliefs that may be contributing to the patient’s distress (see Supplementary Figure 1).
Based on the information gathered, the therapist can present in the second session the identified anxious, depressive, and excessive stress symptoms. Following this, the cognitive conceptualization diagram can be introduced. It is a visual tool that presents a conceptual model of the case, explaining how the patient’s core beliefs, thoughts, emotions, and behaviors are interconnected (see Supplementary Figure 2).
The third assessment session focuses more on understanding the current conflict: When and how did it start, who is involved, and what is the history of the relationship with the other people involved? At this point, it is important to also try to understand the patient’s communication skills, ability to connect empathically, and personal values.
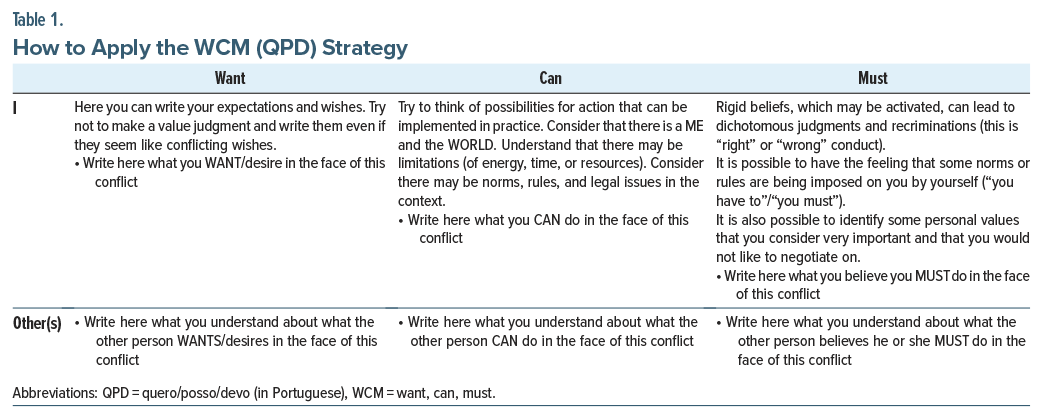
Below, we present a guide on how the WCM strategy was applied throughout the 5 sessions, considering 3 steps:
First, to understand the context, the following questions are asked: What is happening? Since when? Who is involved in the conflict? What kind of damage has the conflict caused/is causing/will cause?
Step 1: Three questions to ask oneself: (1) What do I want to do? (2) What can I do? (3) What must I do? In this first stage, it is important for the client to understand the following: (1) Do their desires seem to be minimally compatible with reality and with the desires of the other people involved? (2) Are there limits, impediments, or restrictions imposed in reality that make any alternative unfeasible? (3) What are the possible beliefs that may be being activated? Are there all-or-nothing thoughts (containing words like always, never, nothing, everything, every time) or with accusation or recrimination content (I have to, I must, I should)? What are the values that guide the subjects, over which there is no negotiation? At this step, depending on the characteristics of the client and the context, it is possible to use strategies that can favor cognitive restructuring, psychological acceptance, defusion, impulse control, and the activation of compassion and self-compassion.
Step 2: Three questions that need to be answered after communicating with the other party: (1) What does the other person think that they want? (2) What does the other person think they can do? (3) What does the other person believe they must do? The reflection at this step aims to assist the patient in understanding the following: (1) Does what the other person wants seem to be minimally compatible with reality and with the desires that the other parties may present? (2) Are there limitations, impediments, or restrictions imposed in reality that make some alternative unfeasible? (3) What are the other person’s beliefs that may be activated? Is the other person expressing thoughts that contain absolutist language (always, never, nothing, everything, every time)? What are the other person’s values that, in his or her view, could be affected and that he or she is not willing to negotiate on? Depending on the client and contextual factors, in the second stage, some other clinical practices may be appropriate: providing psychoeducation on empathy; offering training to enhance empathic connections; promoting mindfulness in social interactions; delivering training to improve assertive communication; and implementing interventions that support psychological acceptance and compassion.
Step 3: Choosing and implementing actions and monitoring the consequences. If there is more empathetic connection, assertive communication between the parties, and psychological acceptance (understanding of the variables over which they have or do not have the possibility to control), there will be a tendency to select actions with the intention of minimizing harm to all individuals involved in the conflict. In this final phase, it is crucial for both parties to acknowledge the efforts made by each individual in the following aspects: understanding the conflict from the other person’s perspective, effectively communicating intentions and expectations regarding actions and potential outcomes, and accepting that there may be inevitable harm to oneself, the other person, or both parties, with the understanding that such harm can be mitigated over time (Table 1).
RESULTS
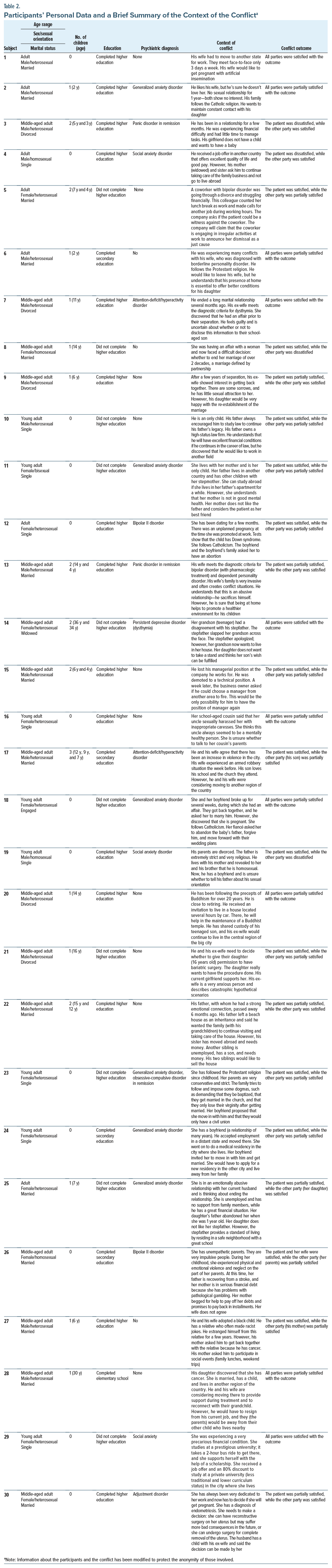
Thirty-two subjects were evaluated. Two people were excluded from the research: a woman who met the diagnostic criteria for borderline personality disorder and a man who suffered from substance abuse and paranoid personality disorder.
Table 2 presents data from the 30 subjects and a brief summary explaining the context of the conflict. The mean age was 38.3 years, with an SD of 11.9. The sample was composed of 17 men and 13 women. Regarding sexual orientation, 15 subjects were heterosexual, 4 were homosexual, and 1 was bisexual. Considering marital status, 14 subjects were married, 10 were single, 5 were divorced, and 1 was widowed (Table 2).
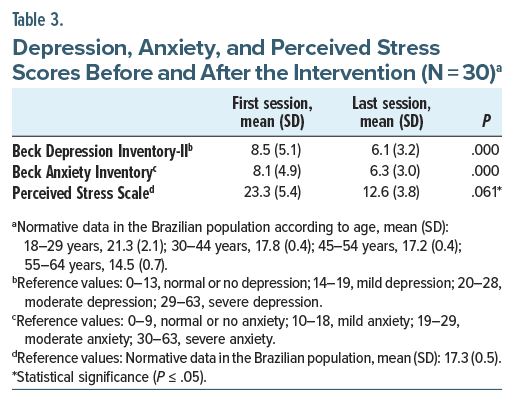
Table 3 presents the mean (SD) of the scores of the instruments that were used to assess depression and anxiety symptoms and perceived stress at 2 time points: at the first session and after the last session.
There was no significant difference when comparing depression and anxiety scores before and after the intervention. However, there was a statistically significant reduction in perceived stress scores.
The initial evaluation revealed that 6 subjects presented with mild depression, and 7 presented with mild anxiety. The remaining participants had subclinical levels of depression and anxiety. In contrast, the final assessment revealed that only 2 participants exhibited mild depression scores, and another 2 presented with mild anxiety scores.
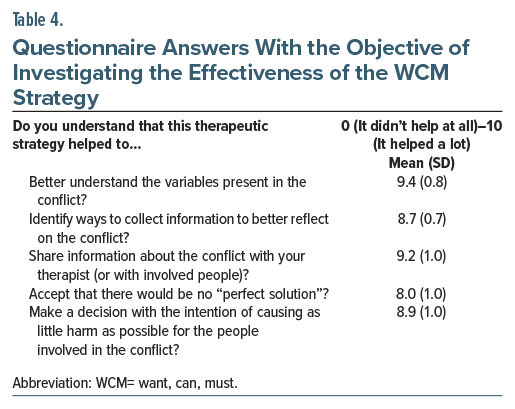
Table 4 shows how the subjects responded to the questionnaire designed to assess the effectiveness of the WCM strategy. When the subjects were asked if they noticed any adverse effects, discomfort, or worsening of the condition, all responded that there were none.
DISCUSSION
The WCM strategy was well evaluated by participants in the areas it aimed to assist: understanding the variables present, gathering information, sharing information, and taking actions intended to cause the least possible harm to everyone. The choice of psychotherapeutic strategies depended on the patient’s profile and their specific context. The process-based approach to CBT aligns with these principles. It is an integrative therapeutic approach that seeks to understand and modify the psychological processes underlying the client’s problems.4 After a thorough assessment and conceptualization of the case, it becomes possible to select various psychotherapeutic tools, provided that these strategies have demonstrated scientific effectiveness, the therapist possesses the necessary expertise to apply them, and they are also suitable for the patient’s profile.
The patients presented diverse needs, and the WCM strategy facilitated the psychotherapist’s selection of appropriate strategies by considering the client’s profile and their specific context. These psychotherapeutic strategies aimed to promote mindfulness, empathic connection, compassion, assertiveness, acceptance, modification of distorted thoughts/beliefs, and decision-making after analyzing the pros and cons.
Most patients needed social skills training to talk to the other person involved in the conflict, with the aim of better understanding what the other person would like, as well as what the other person understands could be done and believes should be done. Training to stimulate mindfulness in social interaction contributed greatly to fostering empathic connection for patients who had this difficulty, promoting more and better present moment and harmony with the speech, facial expressions, and body language of the person with whom they were interacting.
The questioning of thoughts helped to make all-or-nothing thinking, which triggers intense emotions and tends to worsen conflict, more adaptable and flexible. However, the work aimed at psychological acceptance was even more relevant. The patient accepted that (1) there are variables that are not under our control; (2) given the actions implemented, it is very likely that there will be discomfort for one, the other, or both; and (3) there will be less harm if both parties intend to cause the least harm to everyone involved in the conflict.
It is worth noting that depression and anxiety scores were initially low on average (subclinical) at the start of the intervention, making a significant reduction after the intervention unlikely. The participants’ stress levels were slightly higher than the average level reported in a study examining subjects from the Brazilian population.
The decrease in PSS scores suggests that the intervention aided individuals in coping with internal and external stressors. The bar graph in Figure 1 illustrates that following the intervention, participants’ stress levels were slightly below the normative values of the population.
Five sessions were sufficient to apply the WCM strategy. The questionnaire assessing the effectiveness of the strategy in several aspects indicates that the tool was useful for its intended purpose. Of course, if a conflict required more long-term time management, more sessions would be necessary to monitor reflections and decision-making. For example, a conflict involving a legal process that took many months to reach a verdict would necessitate additional sessions.
We believe that, for this initial study, it was a good idea to exclude patients who met the diagnostic criteria for personality disorder. This is because these individuals experience greater difficulty with empathic connection and hold more rigid beliefs. These factors contribute to the generation and intensification of interpersonal conflicts.
FINAL CONSIDERATIONS
The description of problem-solving steps may not be sufficient to assist clients with conflict contexts. It is crucial to provide a comprehensive guide for training therapists on effectively managing conflict situations in clinical practice, especially for less experienced therapists. The WCM strategy encompasses techniques for collecting, organizing, and sharing information; selecting the most suitable psychotherapeutic strategies at each stage of the process; and facilitating reflective discussions on the conflict with the aim of minimizing harm to all parties involved.
There was a significant reduction in the participants’ stress levels comparing before and after the intervention. The participants reported that the WCM strategy helped them (1) better understand the variables present in the conflict, (2) identify ways to gather information to gain deeper insight into the conflict, (3) share information about the conflict with their therapist (or with the people involved), (4) accept that there would be no “perfect solution,” and (5) make decisions with the intention of causing as little harm as possible to the people involved in the conflict. It is extremely common for individuals to bring conflict situations into therapy, where 2 or more people have disagreements in interests, values, or expectations.
Despite numerous studies highlighting the effectiveness of problem-solving techniques, there is a significant lack of research addressing conflict mediation within the realm of CBT. Additionally, there are no available guidelines to assist cognitive-behavioral therapists in managing conflict situations. In this article, we present steps for therapists to train and apply a strategy to help mediate conflicts brought into the therapeutic setting by clients.
Considering the promising principles of process based psychotherapy, the WCM strategy proposes the use of various psychotherapeutic tools tailored to the client’s context and personality characteristics. In future studies, expanding the sample size and testing the WCM strategy among individuals with more severe depression, within the context of couples therapy, and among subjects meeting the diagnostic criteria for personality disorders could provide valuable insights.
Article Information
Published Online: June 26, 2025. https://doi.org/10.4088/PCC.24m03895
© 2025 Physicians Postgraduate Press, Inc.
Submitted: November 22, 2024; accepted March 7, 2025.
To Cite: Costa RTD, Carvalho MRD, Nardi AE. Conflict mediation by cognitive-behavioral therapy: a new psychotherapeutic strategy. Prim Care Companion CNS Disord 2025;27(3):24m03895.
Author Affiliations: Instituto de Psiquiatria, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil (Costa); Departamento de Psicologia Clínica/Instituto de Psicologia, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil (Carvalho); Medical School/Instituto de Psiquiatria, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil (Nardi).
Corresponding Author: Rafael Thomaz da Costa, PhD, Laboratório de Pânico e Respiração, Instituto de Psiquiatria, Universidade Federal do Rio de Janeiro, Venceslau Brás Ave, 71 – Botafogo, CEP 22290-140, Rio de Janeiro – RJ, Brazil ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- The want/can/must (WCM) strategy can be a useful tool for assisting with conflict mediation in psychotherapy, especially providing guidance on (1) collecting, organizing, and sharing information; (2) engaging in more empathetic or assertive communication; and (3) making decisions with less time and with the intention of causing the least possible harm to everyone involved.
- During the application of the WCM strategy, depending on the context and the client’s profile, several other complementary psychotherapeutic strategies may be necessary to alleviate suffering while experiencing the conflict.
- To obtain good results, it is often necessary to work with clients to achieve greater psychological acceptance, enhance empathic connection, reduce rigid thinking, and foster assertive communication.
References (9)

- Cambridge International Dictionary of English. Cambridge University Press; 1995.
- Barlow DH, Farchione TJ, Bullis JR, et al. The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: a randomized clinical trial. JAMA Psychiatry. 2017;74(9):875–884. PubMed CrossRef
- Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597–609. PubMed CrossRef
- Hayes S, Hofmann S. Process Based CBT. New Harbinger Publications; 2018.
- Costa RT, Carvalho MR, Nardi AE. Systematic review on problem solving and conflict mediation by cognitive-behavioral therapy. Braz J Psychiatry. 2023;6:1–9.
- First MB, Williams JBW, Karg RS, et al. User’s Guide for the SCID-5-CV Structured Clinical Interview for DSM-5 Disorders: Clinical Version. APPI; 2016.
- Faro A, Pereira CR. Factor structure and gender invariance of the Beck Depression Inventory - second edition (BDI-II) in a community-dwelling sample of adults. HPBM. 2020;8(1):16–31. PubMed CrossRef
- de Lima Osório F, Crippa JA, Loureiro SR. Further psychometric study of the Beck Anxiety Inventory including factorial analysis and social anxiety disorder screening. Int J Psychiatry. 2011;15(4):255–262.
- Reis RS, Hino AA, Añez CR. Perceived Stress Scale: reliability and validity study in Brazil. J Health Psychol. 2010;15(1):107–114. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!