Abstract
Objective: To assess depression response and remission rates with electroconvulsive therapy (ECT) in a community clinic and to identify factors predicting success in treatment.
Methods: Thirty-five patients were identified by a retrospective chart review with a diagnosis of major depressive disorder or depressive disorder not otherwise specified (according to the DSM-IV-TR) who were treated with an acute series of ECT at a community ECT clinic from March 1, 2014, to March 9, 2015. Logistic regression examined associations between clinical variables and depression response (defined as ≥50% reduction in score on the Patient Health Questionnaire-9 [PHQ-9]) and remission (final PHQ-9 score <5) rates and anxiety response rates (based on the Generalized Anxiety Disorder 7 item).
Results: Depression response and remission rates were 54.3% and 31.4%, respectively. This was a highly treatment-resistant sample, with an average of 5.3 antidepressant trials prior to initiating ECT. Improvement in anxiety symptoms was associated with depression response (odds ratio: 1.41, 95% CI, 1.11–1.78). Additionally, patients with initial severe anxiety scores were less likely than other patients to exhibit a response in depression (P=.027).
Conclusion: Almost half of this sample of patients with treatment-resistant depression did not respond to ECT in this community-based clinic, highlighting the challenges of treating this condition. Comorbid anxiety symptoms may reduce the likelihood of depression response, as patients with severe anxiety were less likely to respond.
Prim Care Companion CNS Disord 2025;27(4):25m03939
Author affiliations are listed at the end of this article.
Electroconvulsive therapy (ECT) has been shown to be more effective and to provide a more rapid response in the treatment of depression than both placebo and medications in clinical trials.1–3 Despite its robust clinical effects, ECT remains underutilized in patients with depression.4–6 Fewer hospitals, particularly those treating largely publicly insured patients, conduct ECT, which has contributed to a decreased utilization of ECT.7 Due to a number of additional factors negatively associated with ECT use, including stigma, financial constraints, insurance barriers, legal and political policies, cognitive side effects, and transportation,8,9 ECT is often reserved for patients who have failed multiple medication trials (patients with treatment-resistant depression).10,11 Treatment-resistant depression is associated with poor quality of life, increased mortality, and negative clinical outcomes.12,13
While numerous studies have found robust depression response and remission rates with ECT, these findings are mostly from controlled clinical trials, as opposed to studies in community settings.14 Patients who present for ECT in community settings often have severe, treatment-resistant depression, and they tend to have a higher number of medical and psychiatric comorbidities than patients included in clinical trials.15,16 In contrast to the 70%–90% remission rates commonly cited for ECT, which are often based on highly selected patient populations in clinical trials, remission rates found in a large multisite prospective naturalistic study of community hospitals were 30.3%–46.7%.14 Similarly, response rates among patients who have not responded to 1 or more adequate medication trials are also lower than clinical trials—closer to 50%–60%.17–20
Optimizing treatment and understanding which patients would most likely benefit from ECT is important given that access to ECT can be challenging, with nearly 9 out of 10 general hospitals in the United States not conducting ECT.7 Administration of ECT in community clinics may vary in factors such as number of treatments, electrode placement, and length of seizure. However, overall, few characteristics have been identified as clinically useful predictors for successful ECT treatment.18 This study sought to examine depression response and remission rates, as well as clinical predictors of response to ECT, in a community setting.
METHODS
Study Participants
Pine Rest Christian Mental Health Services (PRCMHS), located in Grand Rapids, Michigan, is a large, not-for-profit, free-standing mental health organization. PRCMHS offers a spectrum of comprehensive psychiatric services ranging from inpatient and partial hospitalization to a network of outpatient clinics in the surrounding community. Patients are referred to the Pine Rest ECT Clinic from regional inpatient and outpatient settings. We performed a retrospective chart review to examine depression response and remission rates and to look at clinical factors associated with depression response. Medical records for patients treated with an acute series of ECT at Pine Rest ECT Clinic were reviewed. Approval for this study was obtained from Mercy Health Saint Mary’s Institutional Review Board.
Eligible participants were patients aged 18 years and older who were treated with an acute series of ECT from March 1, 2014, to March 9, 2015. Inclusion criteria were a primary diagnosis of major depressive disorder or depressive disorder not otherwise specified (NOS) according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR).21 If a patient had received another series of ECT treatments within the prior 6 months, they were excluded from the study. Patients with an initial score of less than 20 on the 9-item Patient Health Questionnaire (PHQ-9)22 and patients with a DSM-IV-TR diagnosis of bipolar disorder, schizophrenia, schizoaffective disorder, or dementia were excluded. Ninety-two patients were identified who had a diagnosis of major depressive disorder or depressive disorder NOS, and their charts were screened for inclusion. Of these, 57 patients were excluded (37 had a PHQ-9 score of less than 20, 7 had a diagnosis of dementia, 6 had a diagnosis of bipolar disorder, 3 were unable to complete a PHQ-9 assessment, 3 received ECT treatment within the prior 6 months, and 1 patient did not have any follow-up PHQ-9 scores). Thirty-five patients were included in the study.
ECT Treatment Procedure
The acute series of ECT treatment involved treatments 3 times per week, typically on a Monday, Wednesday, and Friday schedule. A complete acute series was defined as completion of 12 treatments. Patients were started with bilateral or right unilateral electrode placement, based on the recommendation of the primary treating psychiatrist or the psychiatrist providing the second opinion for ECT. Based on clinical discretion, some patients were switched from bilateral to right unilateral electrode placement, others switched from right unilateral to bilateral electrode placement, and others did not switch electrode placement during the course of treatment. Patients could receive ECT treatment while psychiatrically hospitalized or on an outpatient basis.
All patients were treated using the Thymatron System IV machine, manufactured by Somatics, LLC, with a pulse width of 0.50 ms and a current of 0.90 A. Methohexital was the medication of choice for induction of anesthesia, but etomidate was used if there was difficulty achieving seizure, if the patient was taking an antiepileptic medication or benzodiazepine, or if the patient had received ECT previously with etomidate. Succinylcholine was used to induce paralysis. Charge dose was determined by the psychiatrist providing ECT treatment. In general, a therapeutic dose was considered approximately 1½ to 2½ times the seizure threshold when giving bilateral treatments and approximately 5–7 times the seizure threshold when giving right unilateral treatments.
Data Collection and Outcome Measures
Study data including sex, age, diagnosis, electrode placement, number of treatments, number of antidepressant medication trials, and scores on assessment tools were obtained by review of the medical record for the first 12 treatments received during the acute series. Patients completed the PHQ-923 and the Generalized Anxiety Disorder 7-item scale (GAD-7)24 prior to each ECT treatment. The Hamilton Depression Rating Scale (HAMD-17)24 and the Montreal Cognitive Assessment (MoCA)25 were administered before the first, sixth, and last ECT treatments. Response for depression was defined as a 50% or greater reduction of the PHQ-9 score. A secondary measure of response for depression was a 50% or greater reduction in the HAMD-17 score. Response for anxiety was defined as a 50% or greater reduction in GAD-7 scores. Remission for depression was defined as PHQ-9 score <5,23 with a secondary measure for remission being a score ≤7 on the HAMD-17.26 Change scores were calculated for PHQ-9 and GAD-7 scores by subtracting final scores from initial scores for each patient at the conclusion of the acute series of ECT.
Statistical Analysis
Descriptive statistics were analyzed for demographic and treatment variables. Based on previously reported response rates of 50%–60% for patients who had not responded to 1 or more adequate medication trials,17–20 χ² goodness-of-fit tests were used to compare response rates in this study to a 55% response rate. Chi-square goodness-of-fit tests were also utilized to assess remission rates and used a comparison remission rate of 38.5%, the midpoint of the remission rates range found in a prior study of ECT in community hospital settings.14 Chi-square tests of independence were used to compare response rates between patients differing in demographic and treatment variables, including initial electrode placement, initial treatment location, age, MoCA scores, and initial anxiety scores (above or below screening score). Additional logistic regression analyses were utilized to determine predictors of PHQ-9 response. Patients missing the first or second HAMD-17 score were excluded from analyses. When final scores for the HAMD-17 or PHQ-9 were missing, last observation carried forward was used for analyses.
RESULTS
Patient Demographics and Clinical Features
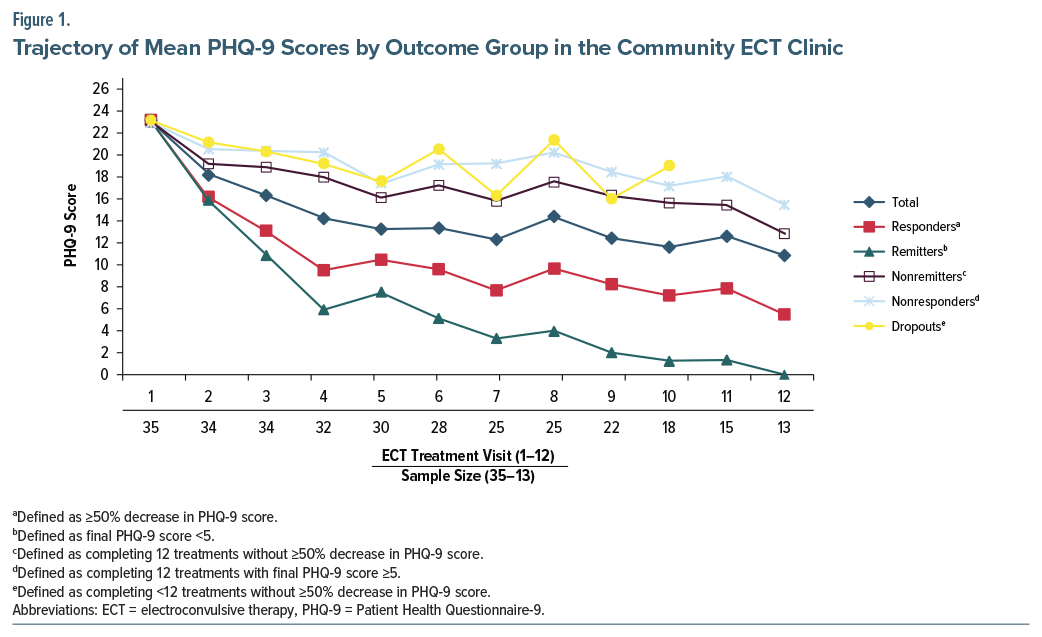
Of the 35 patients included in the study, 22 were women, 13 were men, and the mean age was 52.9 (SD=12.9) years. The mean number of treatments was 9.3 (SD=3.0). Although an exhaustive previous medication trial history, including duration and dose of medication use, was not elicited by psychiatric providers in a standardized manner, from available data recorded in psychiatric assessments, the mean number of antidepressant medication trials was 5.3 (SD=2.4). Twenty-four patients (68.6%) started treatment while on an inpatient psychiatric unit, and 22 (62.9%) started with bilateral electrode placement. Thirteen patients completed at least 12 treatments, and of these, 6 responded and 2 remitted. Of the 21 patients who did not complete 12 treatments, 13 responded and 9 remitted. Eight patients dropped out of treatment without responding before completing 12 treatments. See Figure 1 for the trajectory of mean PHQ-9 scores by outcome group.
Electrode placement was based on clinical judgement by the primary treating psychiatrist, and a total of 8 patients switched electrode placement during the course of treatment. Of the 22 patients who started with bilateral treatment, 3 patients switched to right unilateral treatment; of the 13 patients who started with right unilateral, 5 switched to bilateral. Among patients who started with bilateral treatment, 11 (50.0%) had a response in their depressive symptoms, compared to 8 of the 13 patients who started with right unilateral (61.5%); however, this difference was not statistically significant, χ²1 (N = 35) = 0.44, P = .51. Eight of the 23 patients who started on an inpatient psychiatric unit switched to outpatient. Response rates on the PHQ-9 for those patients who started ECT while inpatients (67.6%) did not significantly differ from response rates for patients who started ECT while outpatients (32.4%), χ²1 (N = 34) = 1.79, P = .18. Similarly, there was no difference found in PHQ-9 response rates when comparing those age 65 years and older (42.9%) with those younger than 65 years (57.1%), χ²1 (N = 35) = 0.461, P = .497.
Although patients with a diagnosis of dementia were excluded from the study, 6 of the 31 patients who completed the MoCA (19.4%) had a score <22 prior to ECT, which is a score consistent with a likely diagnosis of neurocognitive disorder.27 While only 16.7% of patients with a MoCA score <22 responded on the PHQ-9, 56.0% of those with a score ≥22 responded; this difference approached statistical significance, χ²1 (N=31)=3.0, P=.083. Similarly, those with a score <22 were found to be less likely to respond on the HAMD-17 (0%) than those with a score ≥22 (57.1%), χ²1 (N=25)=4.40, P=.036.
Response and Remission Rates
Overall, 19 patients (54.3%) had depression response on the PHQ-9, which was the primary response measure. A total of 11 patients (31.4%) met remission criteria as measured by the PHQ-9, and 23.1% of patients remitted as measured by the HAMD-17. Initial PHQ-9 scores did not predict PHQ-9 response rates (odds ratio [OR] = 1.062, 95% CI, 0.780–1.446, P = .701), suggesting that among this group of patients with severe depression, initial depression severity was not predictive of response to treatment.
Nineteen patients (54.3%) had response of anxiety symptoms, as measured by 50% reduction in GAD-7 score. Among patients who exhibited a response on the PHQ-9, 84.2% also exhibited a response on the GAD-7. Logistic regression analysis found that both PHQ-9 and HAMD-17 response rates were significantly associated with improvements in GAD-7, with ORs of 1.407 (95% CI, 1.113–1.779, P=.004) and 1.281 (95% CI, 1.033–1.588, P=.024), respectively. Initial GAD-7 scores did not predict PHQ-9 response rates, OR=0.950 (95% CI, 0.812–1.112, P=.523). Additionally, correlations between initial GAD-7 and PHQ-9 scores (r33 =0.299, P=.081) were not statistically significant and were of a lesser magnitude than the correlation between GAD-7 change scores and PHQ-9 change scores (r33 =0.744, P<.001), indicating that amount and direction of change in 1 measure was positively associated with amount and direction of change in the other measure. Patients with initial severe anxiety scores (GAD-7≥15) were less likely than other patients to exhibit a response in depression as measured by the PHQ-9 (χ²1 [N=35]=4.900, P=.027 [41.7% vs 81.8%]).
DISCUSSION
In this highly treatment-resistant community sample, with an average of 5.3 antidepressant trials prior to initiating ECT, the response and remission rates for depression with ECT treatment were 54.3% and 31.4%, respectively. Our remission rate is much lower than the 70%–90% remission rates reported by controlled clinical trials but is more consonant with similar studies assessing community samples.
For example, one 7-hospital multisite study reported remission rates of 30.3%–46.7%,14 and 1 large-scaled population-based cohort study conducted among 6,998 patients drawn from the Swedish National Quality Register for ECT reported that 2,749 patients (39.3%) achieved remission after ECT.28 Moreover, both our response and remission rates are more comparable to similar small-scaled community studies reporting remission rates ranging from 27% to 58.1% and response rates ranging from 41.3% to 84.3%.29–31 However, some of the discrepancy in these figures with our own may be secondary to clinical heterogeneity at baseline and best explained by the strong treatment resistance among our patient population. The average number of documented antidepressant trials was 5.3, suggesting that the patients in this study had significant medication resistance. Not only is resistance to medication trials a predictor of poor response to ECT treatment, but the degree of resistance to previous treatments has been found to be the strongest predictor of nonresponse to ECT.32 For example, the response rate reported in a meta-analysis conducted on 32 studies and published in 2015 was 58% for those with a prior documented medication failure and 70% for those without prior medication failure.18
While success rates for depression treatment were similar to results from comparable studies, these rates are lower than the robust success rates commonly reported for ECT treatment of depression. This finding underscores the clinical challenge encountered with treatment-resistant depression and with patients presenting for treatment in community ECT clinics. Several explanations have been suggested for the discrepancy between outcomes in prospective research trials compared to community treatments with ECT, with earlier discontinuation of treatments in community settings having been proposed as a likely contributor.14 In this study, 8 of the 35 patients dropped out of treatment without responding. Reasons for early patient discontinuation should be further evaluated, as this may contribute to lower than expected depression response rates. Another possible explanatory factor is that patients undergoing ECT in clinical trials may be more likely to be taking prescribed medications during the course of ECT than nonresearch patients. Similarly, patients who self-select for participation in a clinical trial may be more likely to be adherent to treatment recommendations than those in unselected community samples.33,34 It should be noted that while the results are not as robust as would be hoped for, the ECT response rates were still higher than those found for additional medication trials in patients with treatment-resistant depression,13 suggesting ECT is likely underutilized and not used early enough in the treatment course in patients with treatment-resistant depression. This study highlights the need to find ways to maximize ECT benefit and identify factors that predict ECT success.
This study also detected an association between the improvement in anxiety with the improvement of depression during the course of ECT treatment. Anxiety is often comorbid with depression, with the US National Comorbidity Survey Replication study finding the prevalence of 12-month comorbidity of an anxiety disorder among those with major depressive disorder to be 53.3%–61.7%.35 Additionally, in patients with depression, comorbid anxiety has been found to adversely affect outcomes not only with medication treatment36,37 but also with ECT.38,39 As of yet, limited data regarding anxiety symptom response with ECT exist,40–42 and given its prevalence in patients with depression, this warrants further investigation. We found that patients who experienced a response in depressive symptoms were also more likely to demonstrate a response in anxiety symptoms.
Patients with high anxiety scores were less likely to experience a response in depressive symptoms than were other patients, with approximately half as many patients with high anxiety experiencing response than those without high anxiety. Of note, these findings were based on anxiety evaluated at first ECT treatment and thus did not differentiate between anxiety related to starting ECT and anxiety unrelated to ECT treatment. However, assessing anxiety level prior to first ECT treatment may be informative in predicting which patients are more likely to have depression that is responsive to ECT treatment. While severity of depression (assessed by initial PHQ-9 scores) did not predict depression response rates, this may be due, in part, to a restricted range of initial PHQ-9 scores due to excluding patients with initial PHQ-9 scores below 20. While previous studies have found demographic factors43 and electrode placement44 to predict depression response, this study did not find these factors to be predictive of depression response. This may be due to a small sample size that limited the power to detect effects of electrode placement, age, and sex.
To help address some of these questions, future research recommendations include evaluating depression response rates in a prospective ECT trial involving adjunctive treatment of anxiety. Evaluating anxiety scores prior to referral to ECT may help differentiate baseline anxiety from anxiety related to ECT. There is a paucity of research evaluating ECT for treatment of anxiety in general and further evaluating this would be of clinical benefit.
There are several limitations to this study. The small sample size limited the power in analyses. Additionally, only 13 of the 35 patients completed 12 sessions, and data regarding reason for early discontinuation were missing. Finally, there was a lack of standardization in the provision of the ECT treatment, and psychiatrists administering treatment may not have titrated treatments in the same way or made recommendations about right unilateral versus bilateral electrode placement consistently. Due to the limited sample size, we were unable to evaluate these potential effects by provider or treatment titration approach.
CONCLUSIONS
Approximately half of the patients in this community sample of patients with highly treatment-resistant depression responded with ECT treatment, and one-third achieved remission. These results, although comparable to success rates of patients in community settings, are lower than what are commonly cited with ECT in clinical trials. Anxiety response rates were similar to depression response rates, and improvement in anxiety symptoms was associated with response in depressive symptoms. Fewer patients with severe anxiety achieved depression response than those without severe anxiety. Further work is needed to understand the reasons for lower response and remission rates in community settings as well as the impact of anxiety on treatment response with ECT.
Article Information
Published Online: August 28, 2025. https://doi.org/10.4088/PCC.25m03939
© 2025 Physicians Postgraduate Press, Inc.
Submitted: February 12, 2025; accepted May 5, 2025.
To Cite: VanBronkhorst SB, Keller JJ, Edwards EM, et al. Depression remission and response rates and anxiety response as a predictor of depression response in a community electroconvulsive therapy clinic. Prim Care Companion CNS Disord 2025;27(4):25m03939.
Author Affiliations: Division of Child and Adolescent Psychiatry, New York State Psychiatric Institute, Columbia University Medical Center, New York, New York (VanBronkhorst); Department of Psychiatry, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, Michigan (Keller, Achtyes); University of Washington, Psychiatry Residency Training Program, Seattle, Washington (Keller); Department of Outpatient and Recovery Services, Pine Rest Christian Mental Health Services, Grand Rapids, Michigan (Edwards, Saleem, Evans, Nykamp, Sanders); Department of Psychiatry, Michigan State University College of Human Medicine, Grand Rapids, Michigan (Edwards, Saleem, Evans, Nykamp, Sanders).
Corresponding Author: Joseph J. Keller, MD, PhD, MS, MPH, University of Washington, Psychiatry Residency Training Program, Northwest Hospital 1550 North 115th St, Seattle, WA 98133-9733 ([email protected]).
VanBronkhorst and Keller are co-authors.
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: These data were presented as a poster presentation at the American Psychiatric Association Annual Meeting; San Diego, California; May 20–24, 2017.
Clinical Points
- Electroconvulsive therapy (ECT) remains an important clinical option for treatment-resistant depression in the community setting, with approximately half of patients achieving depression response.
- Anxiety symptoms may be a factor correlated with treatment response, suggesting potential utility in screening for anxiety symptoms in assessing likelihood of success with ECT treatment.
References (44)

- Fink M. What was learned: studies by the consortium for research in ECT (CORE) 1997-2011. Acta Psychiatr Scand. 2014;129(6):417–426. PubMed CrossRef
- Kho KH, van Vreeswijk MF, Simpson S, et al. A meta-analysis of electroconvulsive therapy efficacy in depression. The J ECT. 2003;19(3):139–147. PubMed CrossRef
- Carney S, Cowen P, Dearness K, et al. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361:799–808.
- Wilkinson ST, Agbese E, Leslie DL, et al. Identifying recipients of electroconvulsive therapy: data from privately insured Americans. Psychiatr Serv. 2018;69(5):542–548. CrossRef
- Sackeim H. Modern electroconvulsive therapy: vastly improved yet greatly underused. JAMA Psychiatry. 2017;74(8):779–780. CrossRef
- Taylor S.. Electroconvulsive therapy: a review of history patient selection, technique, and medication management. South Med J. 2007;100(5):494–498. PubMed CrossRef
- Case BG, Bertollo DN, Laska EM, et al. Declining use of electroconvulsive therapy in United States general hospitals. Biol Psychiatry. 2013;73(2):119–126. PubMed CrossRef
- Livingston R, Anandan S, Moukaddam N. Electroconvulsive therapy, transcranial magnetic stimulation, and deep brain stimulation in treatment-resistant depression. Psychiatr Ann. 2016;46(4):240–246. CrossRef
- Philpot M, Treloar A, Gormley N, et al. Barriers to the use of electroconvulsive therapy in the elderly: a European survey. Eur Psychiatry. 2002;17(1):41–45. PubMed CrossRef
- Heijnen W, Birkenhäger TK, Wierdsma A, et al. Antidepressant pharmacotherapy failure and response to subsequent electroconvulsive therapy: a meta-analysis. J Clin Psychopharmacol. 2010;30(5):616–619. PubMed CrossRef
- Alpert JE. Improving depression outcome: new concepts, strategies and technologies. J Psychopharmacol. 2006;20(3 suppl):3–4. PubMed CrossRef
- Fekadu A, Wooderson S, Markopoulo K, et al. What happens to patients with treatment-resistant depression? A systematic review of medium to long term outcome studies. J Affect Disord. 2009;116(1–2):4–11. PubMed CrossRef
- Sinyor M, Schaffer A, Levitt A. The Sequenced Treatment Alternatives to Relieve Depression (STAR* D) trial: a review. Can J Psychiatry. 2010;55(3):126–135. CrossRef
- Prudic J, Olfson M, Marcus SC, et al. Effectiveness of electroconvulsive therapy in community settings. Biol Psychiatry. 2004;55(3):301–312. PubMed CrossRef
- Abrams R.. Electroconvulsive Therapy. 4th ed. Oxford University Press; 2002.
- American Psychiatric Association. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging: A Task Force Report of the American Psychiatric Association. 2nd ed. American Psychiatric Association; 2001.
- Sackeim HA, Prudic J, Devanand DP, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral electroconvulsive therapy at different stimulus intensities. Arch Gen Psychiatry. 2000;57(5):425–434. PubMed CrossRef
- Haq AU, Sitzmann AF, Goldman ML, et al. Response of depression to electroconvulsive therapy: a meta-analysis of clinical predictors. J Clin Psychiatry. 2015;76(10):1374–1384. PubMed CrossRef
- Prudic J, Haskett RF, Mulsant B, et al. Resistance to antidepressant medications and short-term clinical response to ECT. Am J Psychiatry. 1996;153(8):985–992. PubMed CrossRef
- Devanand DP, Sackeim HA, Prudic J. Electroconvulsive therapy in the treatment-resistant patient. Psychiatr Clin North Am. 1991;14(4):905–923. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Fourth Edition, Text Revision. American Psychiatric Association; 2000.
- Kocalevent RD, Hinz A, Brähler E. Standardization of the depression screener Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2013;35(5):551–555. PubMed CrossRef
- Coley RY, Boggs JM, Beck A, et al. Defining success in measurement-based care for depression: a comparison of common metrics. Psychiatr Serv. 2020;71(4):312–318. CrossRef
- Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. PubMed CrossRef
- Freitas S, Simões MR, Alves L, et al. Montreal Cognitive Assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord. 2013;27(1):37–43. PubMed CrossRef
- Leentjens AF, Verhey FR, Lousberg R, et al. The validity of the Hamilton and Montgomery-Asberg depression rating scales as screening and diagnostic tools for depression in Parkinson’s disease. Int J Geriatr Psychiatry. 2000;15(7):644–649. PubMed CrossRef
- Borland E, Nägga K, Nilsson PM, et al. The Montreal Cognitive Assessment: normative data from a large Swedish population-based cohort. J Alzheimers Dis. 2017;59(3):893–901. PubMed CrossRef
- Gillving C, Ekman CJ, Hammar Å, et al. Seizure duration and electroconvulsive therapy in major depressive disorder. JAMA Netw Open. 2024;7(7):e2422738. CrossRef
- Alves LP, Freire TF, Fleck MP, et al. A naturalistic study of high-dose unilateral ECT among severely depressed inpatients: how does it work in the clinical practice? BMC Psychiatry. 2016;16(1):396. PubMed CrossRef
- Goegan SA, Hasey GM, King JP, et al. Naturalistic study on the effects of electroconvulsive therapy (ECT) on depressive symptoms. Can J Psychiatry. 2022;67(5):351–360. CrossRef
- Khalid N, Atkins M, Tredget J, et al. The effectiveness of electroconvulsive therapy in treatment-resistant depression: a naturalistic study. J ECT. 2008;24(2):141–145. PubMed CrossRef
- Milev RV, Giacobbe P, Kennedy SH, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. neurostimulation treatments. Can J Psychiatry. 2016;61(9):561–575. CrossRef
- Ten Have TR, Normand SLT, Marcus SM, et al. Intent-to-treat vs. non-intent-to-treat analyses under treatment non-adherence in mental health randomized trials. Psychiatr Ann. 2008;38(12):772–783. CrossRef
- Schulberg HC, Block MR, Madonia MJ, et al. Treating major depression in primary care practice: eight-month clinical outcomes. Arch Gen Psychiatry. 1996;53(10):913–919. PubMed CrossRef
- Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the national comorbidity survey Replication (NCS-R). JAMA. 2003;289(23):3095–3105.
- Rivas-Vazquez RA, Saffa-Biller D, Ruiz I, et al. Current issues in anxiety and depression: comorbid, mixed, and subthreshold disorders. Prof Psychol Res Pract. 2004;35(1):74–83. CrossRef
- Pollack MH. Comorbid anxiety and depression. J Clin Psychiatry. 2005;66(suppl 8):22–29.
- Brus O, Cao Y, Gustafsson E, et al. Self-assessed remission rates after electroconvulsive therapy of depressive disorders. Eur Psychiatry. 2017;45:154–160. PubMed CrossRef
- Berggren Å, Gustafson L, Höglund P, et al. A long-term follow-up of clinical response and regional cerebral blood flow changes in depressed patients treated with ECT. J Affect Disord. 2014;167:235–243. PubMed CrossRef
- Obbels J, Verwijk E, Bouckaert F, et al. ECT-related anxiety: a systematic review. J ECT. 2017;33(4):229–236. CrossRef
- Ozdemir O, Yillmaz E, Atilla E. Is electroconvulsive therapy (ECT) effective in the treatment of psychosis or anxiety disorders? report of two cases. J Mood Disord. 2014;4(3):122–125. CrossRef
- Kong XM, Xu SX, Sun Y, et al. Electroconvulsive therapy changes the regional resting state function measured by regional homogeneity (ReHo) and amplitude of low frequency fluctuations (ALFF) in elderly major depressive disorder patients: an exploratory study. Psychiatry Res. 2017;264:13–21. PubMed CrossRef
- van Diermen L, van den Ameele S, Kamperman A, et al. Prediction of electroconvulsive therapy response and remission in major depression: meta-analysis. Br J Psychiatry. 2018;212(2):71–80. PubMed CrossRef
- Kellner CH, Tobias KG, Wiegand J. Electrode placement in electroconvulsive therapy (ECT): a review of the literature. J ECT. 2010;26(3):175–180. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!