Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(3):24f03908
Author affiliations are listed at the end of this article.
Have you ever had a patient be admitted to the intensive care unit (ICU) facing issues that you were ill prepared to manage? Have you wondered whether the ICU experience is traumatic for patients and their family members? Have you been uncertain how clinicians can manage despite facing pain, delirium, and death daily? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Mr A, a 39-year-old married man, became fearful of becoming critically ill again with a pulmonary infection. He developed nightmares and agitation and avoided social gatherings.
Mr A’s father had died in his late 30s with complications of intravenous drug use. His mother, in her late 50s, was prone to worry and had a history of anxiety and depression attributed to adverse childhood experiences (eg, sexual trauma). Prior to Mr A’s hospitalization with acute respiratory distress syndrome, he was gainfully employed. He never smoked cigarettes and only drank socially. Mr A described himself as a man of faith who attends services regularly.
Mr A had asthma as a child, which resolved by his teens. Prior to his critical illness, Mr A had never sought psychiatric care, despite having a tendency toward becoming anxious and depressed during major life changes.
When Mr A developed a cough, fever, diaphoresis, and pain breathing, he was started on antibiotics for pneumonia. Unfortunately, despite receiving additional antibiotics, he struggled to breathe and required oxygen and a chest tube and was intubated after a lung collapsed. He feared that he might not survive, thinking, “This is it.”
While in the ICU, he developed delirium, with agitation, paranoia (thinking that someone cut off his penis), and visual hallucinations (seeing children running around with animal heads). He recalled having been restrained and thought his nurses were trying to kill him. The mechanical ventilation, inability to communicate effectively due to intubation, and overall sense of vulnerability and loss of control exacerbated his fear. His inability to fully comprehend the severity of his condition, along with the isolation of the ICU, contributed to a heightened sense of panic. Mr A also developed a profound sense of loneliness, which, combined with his delirium, made him fearful of his surroundings and of the health care staff, whom he believed were trying to harm him. This distress was compounded by his poor sleep, thirst, hunger, and uncertainty about his survival. Mr A was given regular reassurance by the ICU team, and low-dose quetiapine was given to help his paranoia and fear, reduce his anxiety, and promote a sense of safety while he was delirious.
Mr A was discharged from the hospital after a 2- week ICU stay that was followed by an additional week long stay on a medical unit. Despite physical therapy (PT) in the hospital and later at home, Mr A remained quite weak and easily fatigued. He struggled to complete daily tasks and felt frustrated and demoralized that his abilities no longer matched his expectations.
DISCUSSION
How Can Pain, Anxiety, Demoralization, and Delirium Be Managed?
The comprehensive management of pain, anxiety, demoralization, and delirium in the ICU aligns closely with the pain, agitation/sedation, delirium, immobility, and sleep disruption (PADIS) framework, which serves as a guide for improving patient outcomes through an integrated and multidisciplinary approach.1 Pain is influenced by psychological (eg, anxiety and depression) and demographic (eg, age, gender, educational, and financial) factors.2 However, pain management among critically ill adults is complex and requires a comprehensive understanding of each patient. Critically ill individuals often have myriad types of pain, including acute, chronic, and acute-on-chronic pain, which may arise from multiple mechanisms and be categorized as somatic, visceral, and/or neuropathic pain. Assessment of ICU patients is frequently complicated by their inability to communicate their pain effectively due to an altered mental status or mechanical ventilation; however, self-reporting of pain is typically the optimal method for gauging pain intensity. The numeric rating scale (0–10) is a highly reliable and valid self-report pain assessment tool for those who are critically ill and can communicate.1 When communication is not feasible, validated behavioral pain scales, such as the Behavioral Pain Scale and the Critical-Care Pain Observation Tool, can help in the assessment of pain through observable behaviors.3 These tools enable health care providers to identify pain even when a patient is unable to tell you what they are experiencing.
While opioids, including morphine and hydromorphone, are commonly used for pain relief, their side effects (eg, sedation and respiratory depression) can pose significant risks, especially in those who are critically ill. The benefits of these medications should be weighed carefully against their adverse effects, emphasizing the importance of using the lowest effective dose and monitoring closely for side effects. A multimodal approach to analgesia is increasingly recommended, combining opioids with nonopioid analgesics, nonsteroidal anti-inflammatory drugs, and adjunctive agents to optimize pain control while minimizing opioid use.
Nonpharmacologic strategies, including PT, use of relaxation techniques, and cognitive-behavioral strategies, can also enhance pain management. Overall, a comprehensive, individualized approach improves patient outcomes and enhances the quality of care delivered in critical care settings.
Agitation and sedation are closely linked to anxiety, which may coexist with, or result from, delirium, dyspnea, pain, and fear among critically ill individuals.1 Sher and colleagues have emphasized the need to address dyspnea-associated anxiety, as it can exacerbate agitation, complicate ventilator weaning and extubation, and increase the need for sedation agents.4 Thoughtful pharmacologic management involves the cautious and judicious use of agents; benzodiazepines may be more useful for anticipatory vent weaning rather than for dyspnea itself. While commonly used for anxiety, benzodiazepines are known to be deliriogenic and can worsen delirium, disrupt sleep, and negatively impact recovery.1,4 For those with dyspnea, nonpharmacologic interventions (including positioning, pursed lips breathing, and relaxation techniques) should be prioritized, as they have shown efficacy in managing dyspnea and anxiety without the associated risks of sedation or worsening delirium.4 Opioids may also decrease dyspnea; if the patient has comorbid anxiety, the use of antihistaminic agents (eg, hydroxyzine), α-2 agonists, and anticonvulsants (eg, pregabalin, gabapentin, and valproic acid) should be considered. In cases in which there is comorbid delirium, dexmedetomidine, quetiapine, or anticonvulsants may be useful.4 Propofol, an anesthetic with sedative properties, is often used by ICU teams to manage agitation and anxiety; however, it comes with the risk for hypotension and respiratory depression.1 Nonpharmacologic interventions, such as breathing techniques and psychological support, may also be beneficial. Uncontrolled anxiety increases the risk of developing a postintensive care syndrome (PICS), which can lead to long-term psychological, cognitive, and physical impairments, including posttraumatic stress disorder (PTSD).5 Early management of anxiety reduces these risks and improves post-ICU outcomes. The use of ICU diaries by staff and family can also be valuable in helping patients process their experiences and reduce their anxiety during recovery.6,7
Unfortunately, demoralization and comorbid PTSD can severely impact the mental health and recovery of critically ill individuals.8 Demoralization, with profound hopelessness and helplessness in the ICU setting, exacerbates PTSD symptoms and often leads to struggles about finding meaning during recovery, which complicates psychological healing. Addressing these issues promotes resilience, enhances coping mechanisms, and restores patients’ sense of agency.
Delirium, particularly in ICU settings, is a core concern within the PADIS framework. Rosen and colleagues have highlighted the key diagnostic criteria for delirium phenotypes: hypoactive, hyperactive, and mixed.9 Hypoactive delirium, which often goes unrecognized, presents with decreased responsiveness, while hyperactive delirium is marked by agitation and restlessness. Mixed types of delirium typically show a waxing and waning course with alternations between these states.
Although treatment is typically predicated upon etiology, antipsychotics are commonly used to manage hyperactive delirium; however, careful consideration must be given to potential side effects, including QTc prolongation, especially when they are combined with other agents that may prolong the QTc interval. Regular monitoring of cardiac function is important. In addition, dexmedetomidine, an α-2 adrenergic agonist, has shown promise in the management of delirium by reducing the need for deep sedation and shortening delirium’s duration. Its anxiolytic properties make it particularly beneficial in the ICU, especially for those whose agitation interferes with ventilator weaning and extubation.
Families also play a critical role in recognizing and managing delirium, as the impact of a loved one experiencing delirium can exacerbate their own distress and influence health care decisions. Therefore, a holistic approach that considers both the patient and their family’s needs is essential for effective delirium management. By actively involving families in the care process, health care providers can enhance support systems, foster communication, and improve overall patient outcomes.
How Can Nonpsychiatric Physicians and Psychiatrists Collaborate in the ICU?
Critically ill patients and their families face complex problems in ICUs that have affective, behavioral, cognitive, and motor manifestations. Failure to attend to these signs and symptoms runs the risk of jeopardizing the safety of both patients and health care providers, eg, when agitation and confusion obscure rational behavior. Fortunately, over recent decades, increased attention has been paid to so-called psychiatric and neuropsychiatric complications of serious illness to enhance timely and effective care.
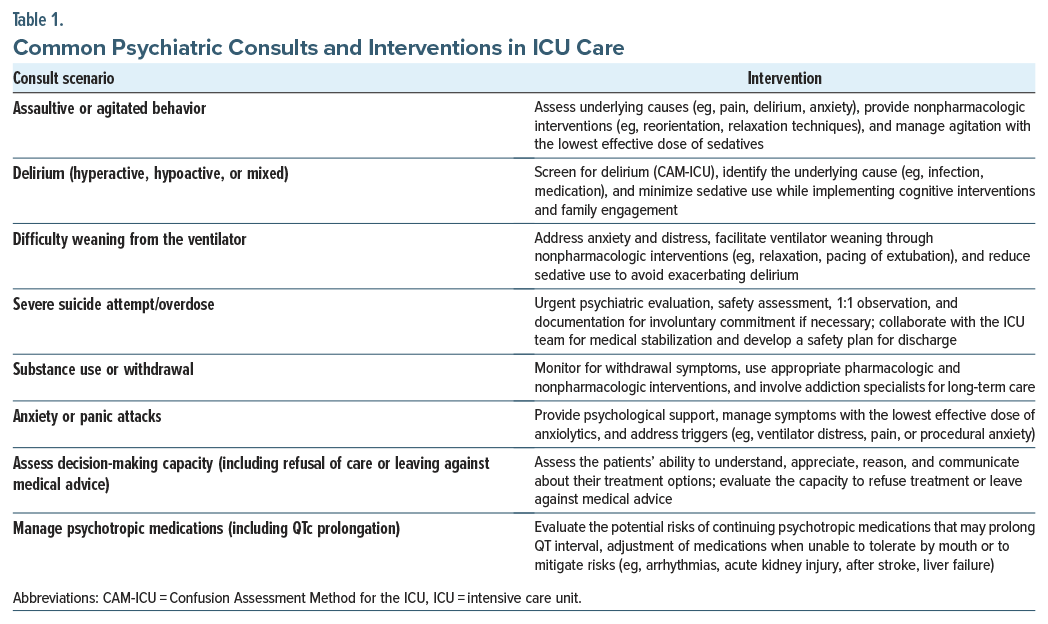
In many hospitals, psychiatric consultations are requested to manage myriad problems, eg, psychiatric presentations of medical conditions, psychiatric complications of medical conditions or their treatment, psychological reactions to medical conditions or their treatments, and medical presentations of psychiatric conditions (Table 1). However, psychiatric assessment in ICUs is often complicated by undue sedation, pain, and impaired cognition and communication ability (eg, associated with delirium, intubation, or use of restraints). Therefore, critical care psychiatrists often become adept at interpreting nonverbal communication, using letter boards, and reading lips, as well as gathering information from family members at the patient’s bedside.
The art of psychiatric consultation relies upon being an excellent and caring physician, while adhering to the medical model, paying close attention to the interface of medical and psychiatric conditions, but not to the exclusion of psychological distress, fear, and demoralization. While aspirational, this scenario may not fully reflect the realities of ICU psychiatric consultations, where time constraints, workload, and limited communication with other staff often mean that consultations are performed by the on-call psychiatrist with little opportunity for in-depth engagement. Therefore, critical care psychiatrists think physiologically and existentially, and they keep abreast of advances in a wide swath of medical and surgical subspecialties. In addition, they attend to challenges imposed by the ICU environment (eg, lights, buzzers, alarms, sleeplessness, and discomfort). Despite, these obstacles, they identify styles of interpersonal interactions that may be problematic and exacerbated by serious illness. Moreover, psychiatrists who work in ICUs tend to employ a flexible approach to patients and problems and often start with attention to “creature comforts” that are few and far between in ICUs.
Rather than creating barriers between patients, providers, and consultants (eg, by asking for more information about the patients and their problems than would be required by other consultants), critical care psychiatrists seek to be helpful and efficient. They speak directly with the referring clinician, review the current and pertinent past records, review the current and past medications (and create a timeline of beneficial and adverse effects), gather collateral data, interview and examine the patient, and formulate a diagnosis and management plan before writing a practical and helpful note and conferring with the requesting physician. Given the often-increased need for liaison skills in ICU settings, where patient care shifts from minute to minute and teams may not always be as communicative with the psychiatric consult team in changing or implementing recommendations, psychiatrists work to facilitate smoother communication and ensure that interventions are appropriately integrated into the care plan. Then, periodic follow-up visits are carried out to ensure that interventions do not “fall between the cracks.” Typically, interventions involve biological (eg, use of pharmacologic agents, awareness of drug-drug interactions), psychological, social, and existential approaches. Moreover, some institutions employ psychiatric consultants who function as integral members of ICU teams. Such relationships enhance patient outcomes, limit post-ICU emotional trauma, and mitigate staff stress.
Issues that arise in ICUs are usually acute and rarely benefit from delaying consultations by several days (eg, until after a weekend). ICU teams are expected to have consultations (eg, for the management of agitation) performed in a timely fashion; impaired communication is not a sufficient reason for intervening slowly.
At times, a definitive understanding of a problem cannot be established with a single visit (eg, determination of the underlying reasons for a suicide attempt), and follow-up visits are required. Psychiatric consultants may also facilitate communication with family, obtain important collateral information, and determine whether and with whom follow-up should be arranged and how primary care providers can be of ongoing help to their patients.
In summary, collaboration between nonpsychiatric physicians and psychiatrists in the ICU requires a comprehensive evaluation, including chart reviews, team input, and patient/family interviews. Tools like the Generalized Anxiety Disorder-7,10 PTSD Checklist for DSM-5,11 Stanford Proxy for Delirium,12 and Confusion Assessment Method for the ICU13 help assess anxiety, trauma, and delirium. Engaging families for collateral information is essential when patients have cognitive impairments. Psychiatrists, whether embedded or consulted, play a key role in managing agitation, delirium, and emotional distress, while supporting families and ensuring follow-up care to address long term mental health needs. It is crucial to recognize the potential risk for PICS, which refers to new or worsening impairments in physical, cognitive, or mental health that arise after critical illness and can persist beyond acute care hospitalization. Risk factors for PICS include premorbid psychiatric conditions and significant experiences of fear, anxiety, delirium, and symptoms like hallucinations or nightmares. Impairments related to PICS include, but are not limited to, pulmonary function, critical illness polyneuropathy and myopathy, diffuse atrophy, and cognitive dysfunction (eg, memory, attention, processing speed). A multidisciplinary collaborative approach not only improves immediate recovery but also helps mitigate long-term psychological outcomes associated with PICS. However, continuity of care can be challenging, as the only communication to the PCP is typically a discharge summary, often lacking detailed information on ICU-based psychiatric events. Ensuring better communication among ICU teams, hospitalists, and primary care providers is crucial for addressing psychiatric conditions postdischarge.
What Kinds of Strategies Can Patients, Clinicians, and Family Members Apply to Cope Better?
When tragedy strikes, everybody responds differently. Some people may have well-defined and practiced strategies for dealing with such challenges, whereas others may be caught off guard and feel unprepared to deal with the numerous physical, logistical, and emotional challenges that surround a course of intensive care. Patients, families, and staff all have unique roles and challenges in this context, so it can be helpful to consider them as separate groups. However, regardless of which group they fall into, all people will generally have important needs in the following domains: biological, psychological, social, and spiritual.
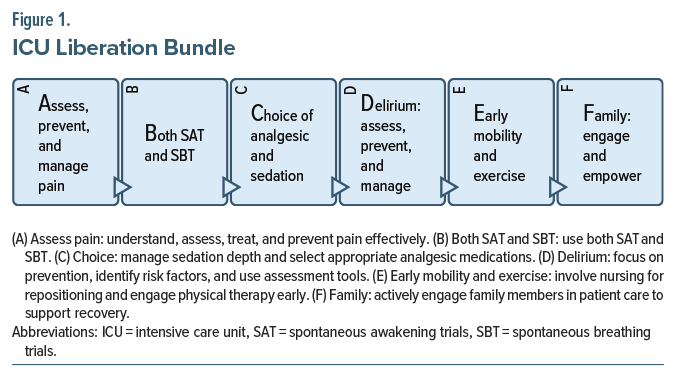
Patients encounter myriad challenges when facing a course of intensive care. Fortunately, the ABCDEF bundle is a framework that describes the most common and important needs for patients receiving intensive care, including (A) assess and manage pain; (B) both spontaneous awakening and breathing trials; (C) choice of analgesia and sedation; (D) delirium assessment, prevention, and management; (E) early mobility and exercise; and (F) family engagement and empowerment (Figure 1).14 The strength of the ABCDEF bundle is that it is an evidence-based framework that simultaneously focuses on both physical and mental aspects of recovery while implementing interventions to improve both short- and long-term outcomes. While many ICUs are already fully implementing the ABCDEF bundle in the critical care setting, other institutions may only utilize specific elements of the bundle or may implement it inconsistently.
Historically, ICU teams focused predominantly on caring for the critically ill body and deferring the care of the mind. However, the ABCDEF bundle has helped ensure a holistic approach by prioritizing lighter sedation strategies and early targeted weaning of sedation and ventilatory support. The ABCDEF bundle has also emphasized the value of early and progressive mobilization, citing its value for preventing deconditioning and delirium. These evidence-based changes in practice have helped ICUs refocus on individualized care by showing that the needs of the individual are equally as important for long-term recovery, especially as ICU survivors are faced with new and unexpected challenges resulting from their critical illness.
For patients with significant emotional reactions to their situation, Griffith and Gaby suggested an existential framework for understanding the emotional distress of medically ill patients experiencing demoralization and then tailoring supportive psychotherapy to the specific issues identified.15 Within this framework, common existential challenges that demoralized patients face include confusion, isolation, despair, helplessness, meaninglessness, fear, and resentment.15 When one of these challenges is at the core of the patient’s distress, the clinician can utilize supportive psychotherapy techniques and collaborative goal setting focused on ICU liberation to help the patient process their emotions and cultivate resilience, with the goal of facilitating recovery and critical care survivorship.
Lastly, the spiritual needs of patients should be addressed. In hospitals, this may often be deferred to chaplains, but if clinicians can help integrate a patient’s spiritual needs into a larger treatment plan, then they may be in the ideal position to help. While many people obtain their spiritual beliefs and practices from religion, every individual interprets and applies them differently, so it is very helpful to engage patients and/or families in discussion of any spiritual needs or conflicts. In addition, they may experience relief upon knowing that they can openly discuss difficult topics such as death, the afterlife, and existential distress with their care team.
As outlined in the ABCDEF bundle, patients’ families are an integral part of their treatment and recovery. Faced with the overwhelming distress of seeing a loved one so sick, and armed with time and strong motivation to help, families can become patients’ most ardent supporters and champions of recovery. Clinicians in the ICU setting can engage patients’ families and loved ones in an empathic way and provide tailored education about critical illness, delirium, and what to expect during the ICU recovery phase. Clinicians may also share resources with families and can model best practices for them, like demonstrating relaxation exercises or how to engage with their loved one who is still critically ill and on a ventilator. The mnemonic, SPOCCC, helps to recall essential supportive interventions for delirious patients in the ICU: support, protect, orient, calm, communicate, and comfort.16
Whereas the patient has many of their biological needs cared for, families often face huge disruptions in their life and may wind up neglecting or forgetting their own needs. It can be helpful to inquire if families are appropriately accessing food, water, sleep, and physical activity while they are working to support their loved one undergoing intensive care. Beyond that, one can also inquire about families’ psychosocial needs by asking how their life is currently affected by having a sick family member or if they have sources of support (personal or professional) that they can speak to about sensitive issues. Because patients and families often share spiritual beliefs or practices, families may be helpful in ensuring that spiritual needs are attended to by obtaining assistance from faith leaders or facilitating relevant spiritual practices.
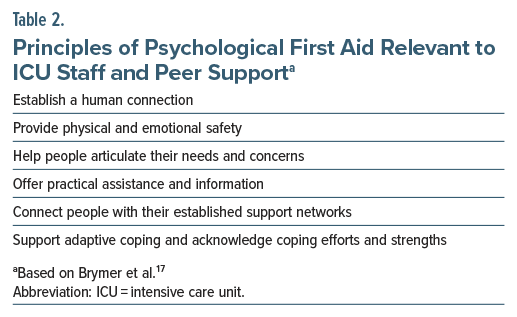
The needs of hospital staff in the ICU setting will often be quite distinct from patients and families. Staff must maintain poise and professional demeanor through all the physically and emotionally demanding work they perform. ICUs are considered a high-stress work environment given the life-threatening and rapidly changing nature of critical illness and the emotional toll that comes with witnessing critical illness and death on a regular basis. Therefore, appropriate measures must be in place to ameliorate staff distress and hopefully decrease burnout and attrition.
Fortunately, ICUs are excellent examples of teamwork that yield better outcomes and handle adversity better than teams with low cohesion. Team leaders should be prepared to manage distressed staff and know how, and to whom, to refer staff who need more assistance. However, prior to making a referral, team leaders and concerned coworkers should employ the basic principles of psychological first aid (Table 2) to encourage healthy coping strategies and cultivate resilience.17
Who Can Support Family Members Through This Devastating Experience?
While family members provide invaluable support to their loved ones in ICUs, nearly half of them experience acute stress, posttraumatic stress, worry, and depression related to their family member’s critical illness and hospitalization. Unfortunately, these symptoms often persist beyond the time of hospital discharge and negatively impact their family member’s outcomes. To enhance well-being of family members, the American College of Critical Care Medicine outlined services provided by patient navigators, care coordinators, social workers, and chaplains who can optimize family support and resilience.18
Patient navigators/case managers. Patient navigators and case managers are liaisons between patients, family members, and the health care system. These staff often have backgrounds in nursing or social work and are trained to facilitate communication between ICU teams and family members.19 In addition, patient navigators and case managers seek to remove obstacles to progress through advocacy, assistance, and education. Advocacy includes informing families of clinical trials that their family member might be eligible for or reviewing the rights of patients and family members. Assistance includes coordinating resources related to transportation services, financial assistance programs, and legal aid organizations, as well as scheduling appointments and organizing medical records. Patient navigators also provide education on conditions, studies, and medications in simple terms.20
Medical social workers. Medical social workers are professionals with skills and knowledge in family dynamics, counseling, and psychosocial risk assessments that they use to help patients and families cope with illness, mediate family conflict (that may arise in the context of the incredible stress of critical illness), and provide support as families learn about clinical updates and make decisions on behalf of their loved ones.21 Through their assessments, social workers also learn about the family’s preferred communication style, understanding of their family member’s wishes, and resources available to the family. They use this information to enhance communication among the ICU staff and the family. Social workers also help coordinate outpatient care resources at the time of discharge.
Chaplains. Chaplains provide spiritual and emotional care to patients and families of all religious faiths. Spiritual care may include prayer, rituals, and sacraments, as well as discussions of meaning, hope, and suffering. Chaplains also provide crisis intervention and grief counseling and are typically present in the hospital at all hours of the day and night. Chaplains may assist families with connections to a faith community outside of the hospital.
The role of the ICU psychiatrist extends beyond the care of surviving patients to addressing the psychological impact of patient death on both family members and health care providers. Family caregivers and surrogate decision-makers are often at risk for psychological distress, including depression, anxiety, and PTSD, particularly when involved in end-of-life care decisions. Health care providers, too, can experience significant emotional strain, and a multidisciplinary collaborative approach, including support from both embedded and consult psychiatrists, can help mitigate these effects and provide comprehensive emotional support.
How Quickly and Completely Do Patients Recover From Their Critical Illness and Posttraumatic Memories?
Critical illness is a severe stressor for patients and their families, and those who survive critical illness often experience new or worsening physical, cognitive, and psychiatric comorbidities.22 Thus, although the field remains focused on survival, it also addresses successful recovery.23
Minimizing sedation and facilitating early mobility improve survivors’ outcomes, reduce delirium, shorten the need for intensive care, and facilitate functional independence.24,25 Rehabilitation specialists (including physical, occupational, and speech-language therapists) perform important roles (including evaluation and treatment of physical [including fine motor and swallowing] and cognitive dysfunction) during critical illness and the early recovery period.
However, noncognitive psychiatric morbidity is also common in survivors of critical illness. Symptoms of PTSD, depressed mood, and general anxiety occur in one-fifth to one-third of ICU survivors.26–28 Therefore, critical illness is like other major life stressors; it is a risk factor for the onset or recurrence of emotional distress, which emphasizes that critical illnesses are often, by definition, life-threatening.29,30 In observational studies, symptoms of PTSD, anxiety, and depression often persist for more than a year after critical illness, in some cases for many years.26–35 Thus, there is an obvious need for psychiatric interventions to prevent long-term psychiatric morbidity.
What Happened to Mr A?
Mr A remained distressed and fearful of a recurrence after his ICU course and became meticulous about cleanliness and germs. He insisted on using a mask when cleaning, changed his sheets frequently, and took immunity-enhancing vitamins and minerals. He worried when he became short of breath at the gym, and he became frightened easily when he had a cough or runny nose; he was difficult to reassure. He developed flashbacks of his time in the ICU (eg, wearing the mask and hearing the ventilator). Having a cold reminded him of his critical illness. He became distant from his loved ones, felt unsupported, had low energy and motivation, and lost his appetite. He became irritable and preoccupied about whether he had done something wrong that led to his illness. At times, when frustrated by his slow physical recovery, he wished that he had died in the hospital, and he did not want to be bothered by others. In addition, Mr A developed difficulty with short-term memory, attention, and multitasking.
Mr A found it helpful to discuss his experiences with a psychiatrist who understood what he had experienced, including breathlessness, need for endotracheal intubation and mechanical ventilation, Foley catheter placement, and need for physical restraints to keep him from pulling out his lines and tubes. They realized that his Foley catheter was likely involved in his nightmarish, delirium-related experience that his penis had been removed. Mr A was reassured to hear that many patients have such frightening experiences and that his fears of getting sick again are quite understandable given what he experienced. Although he was unable to keep his prior, high-intensity job, he was able to obtain a less stressful position in the same field.
CONCLUSION
Assessment of ICU patients is frequently complicated by their inability to communicate effectively due to an altered mental status or mechanical ventilation; however, pain is a frequent companion of intensive care. While opioids, including morphine and hydromorphone, are commonly used for pain relief, their side effects (eg, sedation and respiratory depression) can pose significant risks. Hypoactive delirium often goes unrecognized, while hyperactive delirium (marked by agitation and restlessness) commonly alternates with hypoactive delirium.
Although treatment is typically predicated upon etiology, antipsychotics are commonly used to manage hyperactive delirium; however, careful consideration must be given to potential side effects, including QTc prolongation, especially when they are combined with other agents that prolong the QTc interval. Opioids decrease dyspnea, while antihistaminic agents (eg, hydroxyzine or quetiapine), benzodiazepines, α-2 agonists (eg, guanfacine and dexmedetomidine), and anticonvulsants (eg, pregabalin, gabapentin, and valproic acid) should be considered for anxiety relief. When comorbid delirium exists, dexmedetomidine, quetiapine, or anticonvulsants (eg, pregabalin, gabapentin, or valproic acid) should be considered. Propofol, an anesthetic, also manages agitation and anxiety; however, it comes with the risk for hypotension and respiratory depression.
The ABCDEF bundle is a framework that describes the most common and important needs for patients undergoing intensive care, involving (A) assessment and management of pain; (B) both spontaneous awakening and breathing trials; (C) choice of analgesia and sedation; (D) delirium assessment, prevention, and management; (E) early mobility and exercise; and (F) family engagement and empowerment. Although family members provide invaluable support to their loved ones in ICUs, nearly half of them experience acute stress, posttraumatic stress, worry, and depression related to their family member’s critical illness and hospitalization.
Article Information
Published Online: June 17, 2025. https://doi.org/10.4088/PCC.24f03908
© 2025 Physicians Postgraduate Press, Inc.
Submitted: December 20, 2024; accepted March 31, 2025.
To Cite: Matta SE, Bieber ED, Bui M, et al. Facing intensive care: a guide for primary care providers. Prim Care Companion CNS Disord 2025;27(3):24f03908.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts (Matta, Stern); Department of Psychiatry and Behavioral Sciences, Northwestern University Feinberg School of Medicine, Chicago, Illinois (Bieber); The Pritzker Department of Psychiatry and Behavioral Health, Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, Illinois (Bieber); Department of Psychiatry, Virginia Commonwealth University, Richmond, Virginia (Bui); Department of Psychiatry, Lewis Gale Medical Center, Salem, Virginia (Braford); Ohio Health, Columbus, Ohio (Hardin); Department of Psychiatry and Behavioral Medicine, Wake Forest University School of Medicine, Winston Salem, North Carolina (Dragonetti); Atrium Wake Forest Baptist, Winston Salem, North Carolina (Dragonetti). Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Johns Hopkins Hospital, Baltimore, Maryland (Bienvenu).
Corresponding Author: Sofia E. Matta, MD, Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School, 55 Fruit St, Boston, MA 02114 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- In many hospitals, psychiatric consultations are requested to manage myriad problems, eg, psychiatric presentations of medical conditions, psychiatric complications of medical conditions or their treatment, psychological reactions to medical conditions or their treatments, and medical presentations of psychiatric conditions. However, psychiatric assessment in intensive care units is often complicated by undue sedation, pain, and impaired cognition and communication ability (eg, associated with delirium, intubation, or use of restraints).
- Critically ill patients develop complex problems that involve affective, behavioral, cognitive, and motor manifestations. Failure to attend to these signs and symptoms runs the risk of jeopardizing the safety of both patients and health care providers.
- Critical care psychiatrists emphasize being helpful and efficient. They speak directly with the referring clinician, review the current and pertinent past records, review the current and past medications (and create a timeline of beneficial and adverse effects), gather collateral data, interview and examine the patient, and formulate a diagnosis and management plan before writing a practical and helpful note and conferring with the requesting physician.
- By actively involving families in the care process, health care providers can enhance support systems, foster communication, and improve overall patient outcomes.
References (35)

- Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–e873. PubMed CrossRef
- Grol-Prokopczyk H. Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. Pain. 2017;158(2):313–322. PubMed CrossRef
- Severgnini P, Pelosi P, Contino E, et al. Accuracy of Critical Care Pain Observation Tool and Behavioral Pain Scale to assess pain in critically ill conscious and unconscious patients: prospective, observational study. J Intensive Care. 2016;4:68. PubMed CrossRef
- Sher Y, Desai N, Sole J, et al. Dyspnea and dyspnea-associated anxiety in the ICU patient population: a narrative review for CL psychiatrists. J Acad Consult Liaison Psychiatry. 2024;65(1):54–65. PubMed CrossRef
- Sayde GE, Shapiro PA, Kronish I, et al. A shift towards targeted post-ICU treatment: multidisciplinary care for cardiac arrest survivors. J Crit Care. 2024;82:154798. PubMed CrossRef
- Sayde GE, Stefanescu A, Conrad E, et al. Implementing an intensive care unit (ICU) diary program at a large academic medical center: results from a randomized control trial evaluating psychological morbidity associated with critical illness. Gen Hosp Psychiatry. 2020;66:96–102. PubMed CrossRef
- Huang W, Gao Y, Zhou L, et al. Effects of ICU diaries on psychological disorders and sleep quality in critically ill patients and their family members: a systematic review and meta-analysis. Sleep Med. 2024;122:84–91. PubMed CrossRef
- Kilciksiz CM, Julnes PSS, Owoso A. Demoralization and co-morbid PTSD: a case report and literature review. Psychiatry Res Case Rep. 2023;2(1):100125. CrossRef
- Rosen JH, Bieber E, Matta SE, et al. Hypoactive delirium: differential diagnosis, evaluation, and treatment. Prim Care Companion CNS Disord. 2024;26(1):23f03602. PubMed CrossRef
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. PubMed CrossRef
- Weathers FW, Litz BT, Keane TM, et al The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD; 2013. Accessed May 30, 2025. https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
- Maldonado JR, Waggoner A, Zibrik DJ, et al. Validation of the Stanford Proxy Test for Delirium (S-PTD) in older adults. Int Psychogeriatr. 2018;30(11):1291–1304. PubMed
- Ely EW. Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Chest. 1999;115(4):1135–1142.
- Ely EW. The ABCDEF Bundle: science and philosophy of how ICU liberation serves patients and families. Crit Care Med. 2017;45(2):321–330. PubMed CrossRef
- Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109–116. PubMed CrossRef
- Boland R, Goldstein M, Haltzman S. Psychiatric Management of Behavioral Syndromes in Intensive Care Units. In: Stoudemire A, Fogel B, Greenberg D, eds. Psychiatric Care of the Medical Patient. Oxford University Press; 2000:303.
- Brymer M, Jacobs A, Layne C, et al. (National Child Traumatic Stress Network and National Center for PTSD). Psychological First Aid: Field Operations Guide. 2nd ed; 2006. https://www.nctsn.org/sites/default/files/resources/pfa_field_operations_guide.pdf. Accessed December 17, 2024
- Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103–128. PubMed CrossRef
- Alghanim F, Furqan M, Prichett L, et al. The effect of chaplain patient navigators and multidisciplinary family meetings on patient outcomes in the ICU: the Critical Care Collaboration and Communication Project. Crit Care Explor. 2021;3(11):e0574. PubMed CrossRef
- What is a patient navigator? Western Governors University. 2024. Accessed September 28, 2024. https://www.wgu.edu/career-guide/healthcare/patientnavigator-career.html
- Netzer G. Families in the Intensive Care Unit : A Guide to Understanding, Engaging, and Supporting at the Bedside. 1st ed. Springer International Publishing: Imprint: Springer; 2018.
- Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–509. PubMed CrossRef
- Elliott D, Davidson JE, Harvey MA, et al. Exploring the scope of post-intensive care syndrome therapy and care: engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med. 2014;42(12):2518–2526. PubMed CrossRef
- Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300(14):1685–1690. PubMed CrossRef
- Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373(9678):1874–1882. PubMed CrossRef
- Nikayin S, Rabiee A, Hashem MD, et al. Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2016;43:23–29. PubMed CrossRef
- Parker AM, Sricharoenchai T, Raparla S, et al. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med. 2015;43(5):1121–1129. PubMed CrossRef
- Rabiee A, Nikayin S, Hashem MD, et al. Depressive symptoms after critical illness: a systematic review and meta-analysis. Crit Care Med. 2016;44(9):1744–1753. PubMed CrossRef
- Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161(4):631–636. PubMed CrossRef
- Overstreet C, Berenz EC, Kendler KS, et al. Predictors and mental health outcomes of potentially traumatic event exposure. Psychiatry Res. 2017;247:296–304. PubMed CrossRef
- Bienvenu OJ, Colantuoni E, Mendez-Tellez PA, et al. Depressive symptoms and impaired physical function after acute lung injury: a 2-year longitudinal study. Am J Respir Crit Care Med. 2012;185(5):517–524. PubMed CrossRef
- Bienvenu OJ, Colantuoni E, Mendez-Tellez PA, et al. Cooccurrence of and remission from general anxiety, depression, and posttraumatic stress disorder symptoms after acute lung injury: a 2-year longitudinal study. Crit Care Med. 2015;43(3):642–653. PubMed CrossRef
- Bienvenu OJ, Friedman LA, Colantuoni E, et al. Psychiatric symptoms after acute respiratory distress syndrome: a 5-year longitudinal study. Intensive Care Med. 2018;44(1):38–47. PubMed CrossRef
- Bienvenu OJ, Gellar J, Althouse BM, et al. Post-traumatic stress disorder symptoms after acute lung injury: a 2-year prospective longitudinal study. Psychol Med. 2013;43(12):2657–2671. PubMed CrossRef
- Kapfhammer HP, Rothenhäusler HB, Krauseneck T, et al. Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatry. 2004;161(1):45–52. PubMed CrossRef
This PDF is free for all visitors!