Abstract
Background: Absconding, defined as a patient leaving a hospital or medical facility without permission or.authorization, is a significant concern in psychiatric care, with rates varying across studies. Previous research has identified several factors—such as age, sex, diagnosis, and the treatment environment—that may contribute to the risk of absconding. This study aimed to identify the risk factors associated with absconding incidents and compare them with a matched control group.
Methods: A retrospective observational study was conducted at a psychiatric center in Jaipur, India, from January .2020 to December 2023. The study included 573 patients who .absconded, matched with 573 controls. Data were collected through chart reviews, focusing on .sociodemographic characteristics, clinical profiles, and mental status examination findings.
Results: The absconding rate was 11.54% (573 of 4,962 admissions). Most absconding patients were young males, with a mean stay of 4.07 days before absconding. Significant differences were found in affect (irritable or euphoric), perceptual abnormalities, and judgment. Absconding incidents were most frequent between 2:00 PM and 8:00 PM, and 10% of patients had a history of previous absconding. The duration of hospitalization was significantly shorter for absconders compared to controls.
Conclusion: The study found that absconding patients were primarily young males with irritable or euphoric affect, impaired judgment, and shorter hospital stays. These findings highlight the importance of early risk identification, increased supervision during high-risk periods, and tailored interventions addressing clinical and organizational factors associated with absconding.
Prim Care Companion CNS Disord 2025;27(3):24m03893
Author affiliations are listed at the end of this article.
Absconding is defined as a patient leaving a hospital or medical facility without permission or authorization for a specified duration,1 which can include leaving during escorted leave or being absent beyond the permitted timeframe.2 Studies reveal that the rates of absconding from mental institutions may fluctuate significantly, with estimations between 2.5% and 34% of total psychiatric admissions.3 In a study conducted in Australia, Muir-Cochrane et al4 reported that the absconding rate was notably higher than that in previous studies, suggesting that specific patient and event characteristics may influence these rates. Similarly, a review of absconding incidents in forensic psychiatric settings highlighted that the mean rate of absconding is approximately 12.6%, with significant variation across different facilities and populations.5
In India, recent studies have indicated that approximately 10% of psychiatric patients have a history of absconding, with certain demographic and clinical characteristics associated with this behavior.6 For instance, younger males, particularly those diagnosed with schizophrenia or bipolar disorder, are more likely to abscond.7,8 The age of absconders typically ranges from the late teens to early thirties, with a notable concentration of incidents occurring within the first few weeks of hospitalization.4,9 The motivations for absconding are complex and can be influenced by factors such as dissatisfaction with treatment, feelings of confinement, and the stigma associated with mental illness.1,10 Additionally, the presence of co-occurring substance use disorders has been linked to higher rates of absconding, as these patients may experience heightened impulsivity and a desire to seek substances outside the hospital.7
The inpatient environment itself can contribute to feelings of disempowerment and dissatisfaction among patients, which may lead to absconding. Factors such as lack of autonomy, restrictive policies, and inadequate therapeutic engagement can exacerbate feelings of frustration and hopelessness.11,12 For instance, the use of locked doors in psychiatric wards has been criticized for creating an atmosphere of confinement, which may provoke patients to abscond as a form of resistance.13 Conversely, environments that promote patient autonomy and provide structured activities have been shown to reduce the likelihood of absconding.3,14
Moreover, the social context surrounding patients also plays a critical role in their decision to abscond. Many patients report feelings of isolation and a longing for familial connections, which can motivate them to leave the hospital.9 Qualitative studies highlight that boredom and a lack of meaningful engagement in therapeutic activities contribute significantly to the desire to abscond.10,15 Therefore, enhancing the therapeutic milieu by incorporating family involvement and structured ward activities may mitigate the risk of absconding.
The evasion of mental facilities poses significant concerns for patients and caregivers. It impacts not only the treatment and safety of these individuals but also their caregivers and the community. Absconding can lead to adverse outcomes such as self-harm, suicide, and violence toward others.16,17 A national clinical survey in England revealed that a significant proportion of suicides among psychiatric inpatients occurred after absconding, highlighting the critical need for effective risk assessment and management strategies.16 Furthermore, the potential for harm extends beyond the individual, as absconding patients may pose risks to public safety, particularly in forensic settings where patients may have a history of violent behavior.2
Among the limited studies conducted in India, to our knowledge, only Verma et al6 have explored the characteristics of patients who absconded during their inpatient care at a psychiatric hospital, comparing them with matched controls. Additional research is required to examine the patterns of this phenomenon and the characteristics of individuals who evade treatment. Thus, this study employed a retrospective observational design to investigate incidents of patients absconding from a psychiatric center in India. The primary objective was to identify the risk factors associated with psychiatric inpatients and to compare these findings with those of matched control groups.
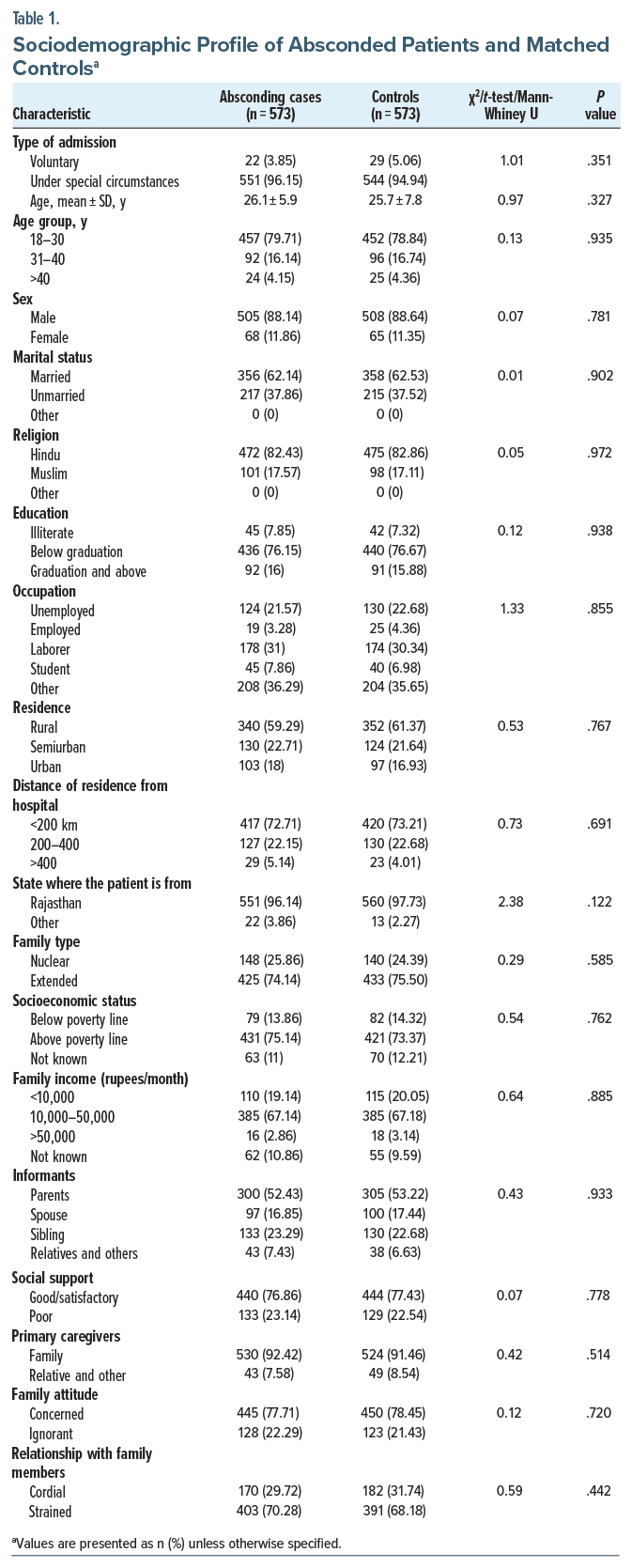
METHODS
This retrospective observational study was conducted at a psychiatric center affiliated with SMS Medical College, Jaipur, India, between January 2020 and December 2023. Ethical approval for the study was obtained from the Institutional Ethics Committee of SMS Medical College. The objective was to identify risk factors associated with absconding behavior among psychiatric inpatients by comparing 573 patients who absconded with 573 matched controls. To ensure comparability between cases and controls, a meticulous matching process was employed. For every patient who absconded, a corresponding control was selected based on specific criteria. First, controls were chosen from the same psychiatric ward to account for environmental and operational variations. Second, matching was performed within the same calendar quarter to minimize temporal biases, such as seasonal trends or staffing changes. Third, controls were matched by primary psychiatric diagnosis to ensure clinical comparability. Additionally, age and sex were considered in the matching process to account for demographic differences that could influence outcomes. Further, the χ2 or Mann-Whitney U test or unpaired t-test showed no significant difference in sociodemographic variables of absconded patients and matched controls (Table 1). This approach effectively minimized potential confounding factors related to ward environment, time of admission, diagnostic category, and demographic characteristics, thereby facilitating a more accurate assessment of the risk factors associated with absconding.
Hospital Settings
The psychiatric center consists of multiple adult psychiatry units, including 4 male wards, 4 female wards, and a specialized addiction psychiatry ward. The facility operates under an open-ward system with secure perimeters and a single controlled entry/exit point. Patients are allocated to nonaddiction units based primarily on bed availability, with no strict allocation criteria concerning age, acuity, or specific treatment needs. However, patients are generally assigned to wards based on factors such as sex and the severity of their psychiatric conditions, though no formal treatment or acuity-based criteria are strictly enforced across the nonaddiction units. All units accept patients with a wide range of psychiatric diagnoses, ensuring diversity in patient profiles. Staffing is organized into 3 shifts daily (morning, evening, and night), with each shift comprising 3–5 nurses, 2–3 ward attendants, and cleaning personnel. Routine ward activities and monitoring, including headcounts at the start and end of each shift, were conducted regularly.
Data Collection
Data were collected from the institution’s absconding registry, which maintains detailed records of incidents reported during headcounts. When a patient absconded, the corresponding case record file (CRF) was reviewed to gather relevant information. Sociodemographic details, including age, sex, marital status, socioeconomic status, and education level, were recorded. Additionally, clinical profiles were examined, covering the patient’s primary diagnosis, past psychiatric history, and current treatment. Mental status examination (MSE) findings, documented twice daily, were also reviewed to assess the patient’s mental state at different intervals. Insight levels were categorized using a 4-grade system: grade 1 for no awareness of illness, grade 2 for partial acknowledgment of symptoms attributed to external factors, grade 3 for general awareness with gaps in understanding, and grade 4 for full awareness of illness and its implications.
If a patient is reported absent during headcounts conducted at the start or end of each shift, the treatment team and hospital management are notified. A thorough search of the hospital grounds is then initiated, and the local police station is informed. If the patient is not found within the hospital and does not return by midnight, either autonomously or with assistance, the incident is officially recorded as an absconding event in the registry. A compilation of CRF numbers for patients who absconded between January 1, 2020, and December 31, 2023, was extracted from the absconding registry. The admission files for each case were reviewed to confirm the admission period and other relevant details. Data collection followed a chart review methodology, where sociodemographic information and specific details related to the absconding incident were systematically recorded. Clinical profiles were constructed based on MSEs conducted upon admission and twice daily thereafter until the patient either received treatment or absconded. MSEs were documented in the CRFs, which contained organized and comprehensive notes. The last MSE performed before absconding was analyzed to identify immediate external factors related to the incident.
Statistical Analysis
The data were initially recorded in Microsoft Excel and later imported into IBM SPSS version 23.0.0 for formal statistical analysis. Quantitative data are reported in terms of mean and SD, whereas qualitative data are summarized in frequency distribution and proportions. Independent t-tests and Mann-Whitney U tests were used to compare normally and nonnormally distributed continuous variables, respectively, while χ2 tests were used for categorical comparisons. A P value < .05 was considered significant.
RESULTS
There were a total of 4,962 admissions in adult psychiatry in the specified period. During this period, 573 patients had absconded. Thus, the absconding rate was 115.4/1,000 admissions (11.54%). The sociodemographic profile of absconded patients and controls (n=573 each) demonstrated no significant differences across most parameters. The majority of both groups were admitted under special circumstances rather than voluntarily (96.15% of cases vs 94.94% of controls, P=.351), were male (88.14% of cases vs 88.64% of controls, P=.781), and were within the age group 18–30 years (79.71% of cases vs 78.84% of controls, P =.935). Other demographic factors, including marital status, religion, education, occupation, socioeconomic status, and family type, were also comparable between groups, with no statistically significant differences (Table 1).
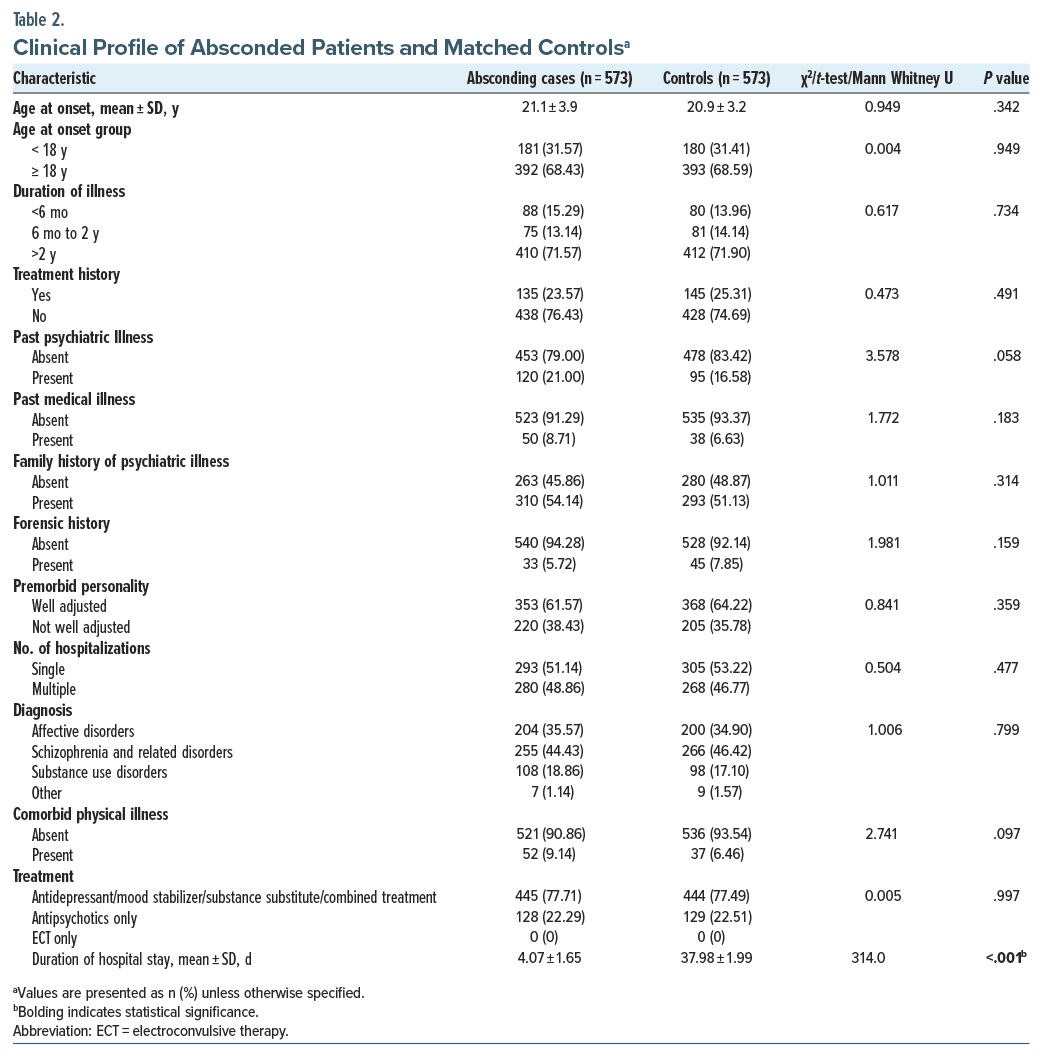
In the clinical profile, the age at onset and duration of illness showed no significant differences. However, a nonsignificant trend was noted, with a slightly higher presence of past psychiatric illness among absconded cases (21%) compared to controls (16.58%, P=.058). Notably, the duration of hospital stay was substantially shorter for absconded patients (4.07±1.65 days) than for controls (37.98±1.99 days), with a significant P value of <.001 (Table 2).
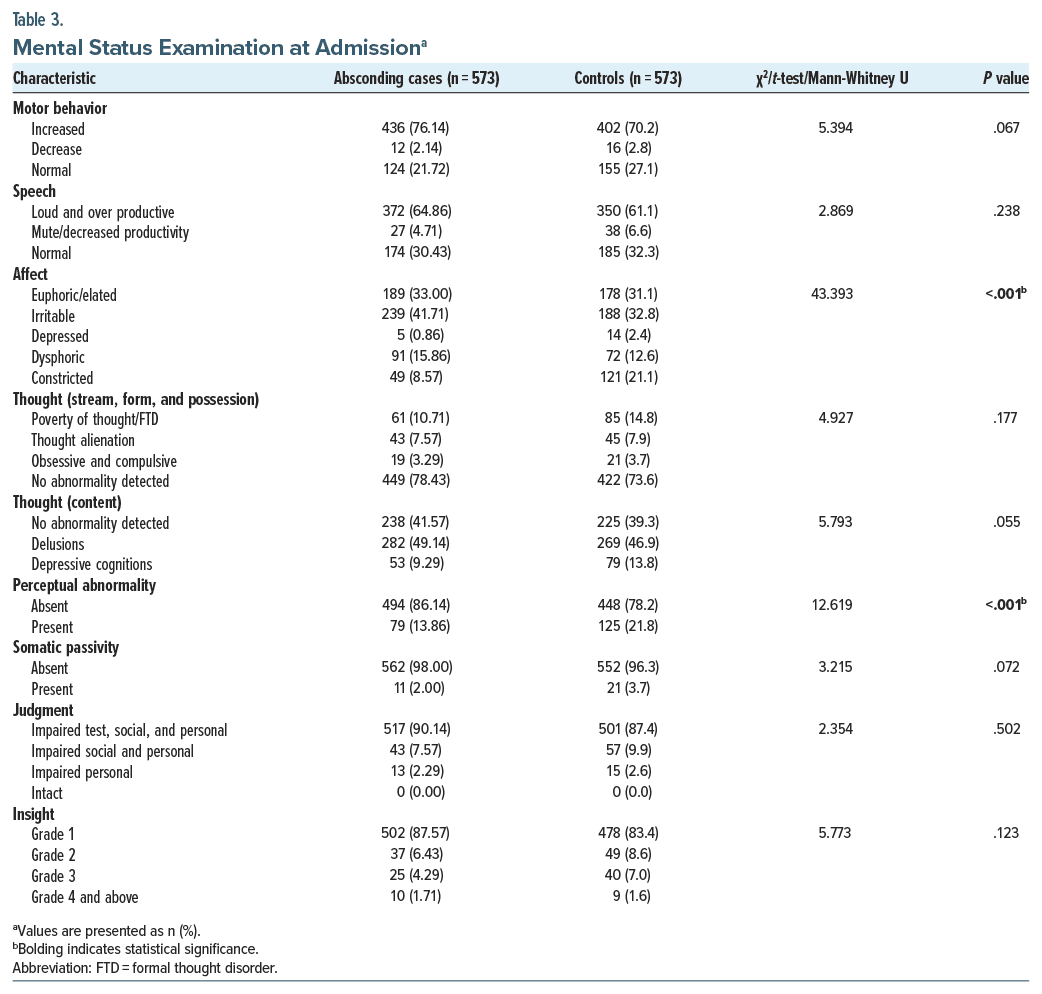
MSE at admission revealed notable differences in affect and perceptual abnormalities. Absconded patients were more likely to exhibit irritable (41.71%) or euphoric/elated (33%) affect compared to controls (32.8% irritable and 31.1% euphoric, P < .001). Furthermore, perceptual abnormalities were present in 13.86% of absconded cases vs 21.8% in controls, showing a significant distinction (P < .001). Other domains of mental status, including motor behavior, speech, thought stream, and judgment, showed no significant differences between groups (Tables 3 and 4).
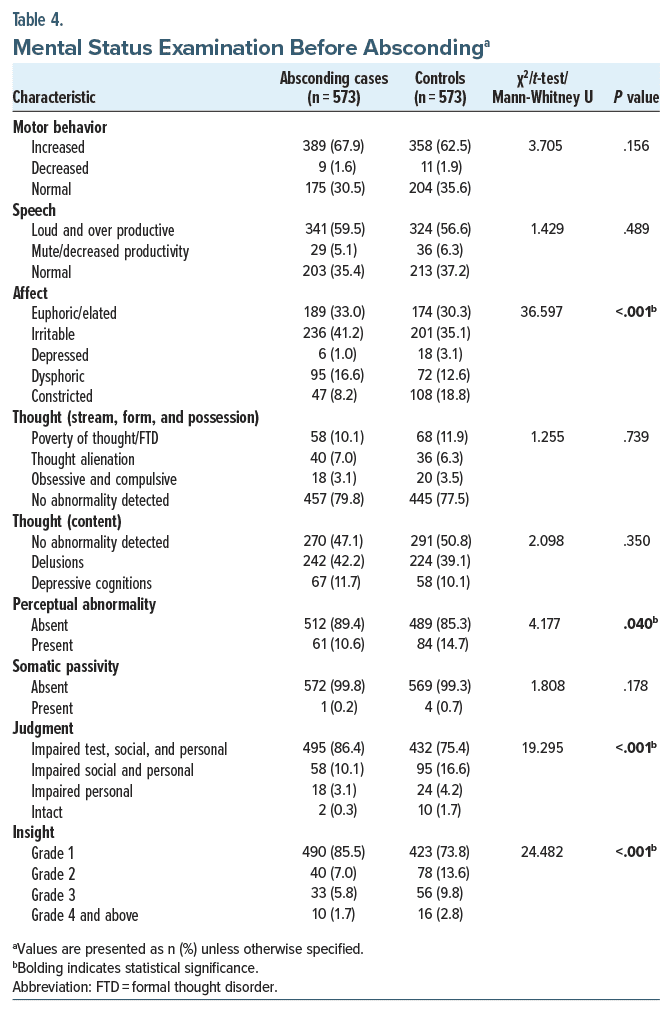
In the present study, 3.8% (n = 22) of patients absconded on the same day. Therefore, their MSE at admission was only considered for MSE before absconding. Absconding patients exhibited more euphoric/elated affect (33.0% vs 30.3%, P < .001) and impaired judgment (86.4% vs 75.4%, P < .001) before absconding. Additionally, perceptual abnormalities were less frequent in absconding cases (10.6% vs 14.7%, P = .040), while they demonstrated a higher proportion of grade 1 insight (85.5% vs 73.8%, P<.001). No significant differences were found in motor behavior, speech, thought stream abnormalities, or thought content between absconding patients and controls before absconding.
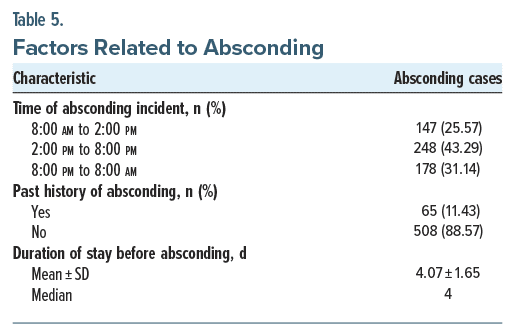
Absconding incidents were most frequent between 2:00 PM and 8:00 PM (43.29%), with fewer cases overnight. Only 11.43% of patients had a history of previous absconding, and the mean duration of stay before absconding was 4.07 ± 1.65 days (Table 5).
DISCUSSION
This study sought to analyze the sociodemographic characteristics of psychiatric inpatients who absconded and to compare them with a matched control group. Over the course of 5 years, we identified 573 absconding patients and matched them to 573 controls in terms of admission period, ward type, and psychiatric diagnosis. This matching protocol allowed us to account for several key environmental and clinical factors, including supervision levels, security measures, and management protocols that could influence absconding behavior. The rate of absconding in our study was found to be 115.4 incidents per 1,000 admissions, which is comparable to the broader range reported in previous studies, where absconding rates have varied from 1.85% to 17.2%.6,7,18
Numerous studies indicate that most absconding patients in our research were hospitalized under exceptional conditions (involuntary admission), aligning with the results of Gowda et al7 and Khammarnia et al.18 These studies have suggested that involuntary admission often correlates with a higher risk of absconding, possibly due to the sense of coercion or perceived loss of autonomy. However, our study did not find a statistically significant difference in the type of admission between absconding and control patients (P = .351). The findings echo the mixed results seen in the literature. For example, Bowers et al19 did not find a higher rate of absconding among involuntary patients, suggesting that the higher reporting of absconding incidents among involuntary patients could be due to more rigorous monitoring or institutional reporting protocols.
Additionally, our study revealed that the majority of absconding patients were young, with 79.71% aged between 18 and 30 years. This is consistent with the observations made by Khammarnia et al,18 Muir Cochrane et al,4 and John et al,20 who noted that younger patients tend to be more likely to abscond. Nevertheless, we did not identify significant age differences between absconding patients and controls (P = .935), suggesting that while younger age is a common characteristic of absconders, it may not fully account for the risk of absconding. Regarding sex, our study found that a significant majority of both absconding patients (88.14%) and controls (88.64%) were male, which is consistent with the findings of Khammarnia et al18 and Gowda et al,7 who also reported a predominance of male patients among those who absconded. Although our study did not find a significant gender difference (P = .781), this may reflect a broader trend within psychiatric care, where males are often more inclined to engage in risky or rebellious behaviors.
In our analysis of marital status, we found no significant differences between absconding patients and the control group (P = .902), consistent with the findings of Khammarnia et al18 and Verma et al.6 However, Gowda et al7 and Muir-Cochrane et al4 suggested that unmarried patients may be more likely to abscond due to reduced family support and social obligations. In terms of family dynamics, most absconding patients in our sample originated from extended families (74.14%), aligning with Verma et al,6 but contrasting with Gowda et al,7 who indicated a higher incidence of absconders from nuclear households. This may reflect cultural or regional variations in family support and pressures. Our findings indicate that family structure alone may not predict absconding behavior; rather, the quality of family relationships appears to be a more significant factor. Furthermore, we noted no disparities between absconding patients and controls on age of symptom start, disease duration, treatment history, mental or medical disorders, family medical histories, or forensic backgrounds, consistent with Verma et al.6
Our findings indicate that the mean age at onset for absconders was 21.1 years, which aligns with previous studies that report a predominance of younger patients among absconders.7,21 The predominant schizophrenia and associated illnesses, followed by affective disorders and drug use disorders. This aligns with previous literature that identifies psychotic illnesses as a common predictor of absconding behavior in psychiatric settings.4,16 The high incidence of schizophrenia among absconders corroborates findings from various studies that emphasize the vulnerability of these patients to absconding due to their mental health conditions.7,22
Subsequent investigation indicated that a significant percentage of absconding patients had an irritated affect both at admission and prior to their departure. This is consistent with findings from Yahyavi and Faraji,22 who suggested that patients with heightened irritability are less likely to report perceptual abnormalities, which may contribute to their absconding behavior.10 Our investigation revealed that absconding patients had less perceptual anomalies at admission than controls, indicating a possible protective factor against absconding incidents. This observation aligns with the notion that a lack of perceptual disturbances may allow patients to maintain a degree of awareness and control over their actions, thereby influencing their decision to leave the hospital.10,22
Judgment and understanding significantly differed between the 2 groups at the moment of absconding. The absconding group mostly had grade 1 insight, while the control group showed enhanced insight levels (grade 2 or above).8,23 This finding is particularly relevant, as previous studies have indicated that impaired insight is a significant risk factor for absconding.6,12 The correlation between insight levels and absconding behavior underscores the importance of mental health professionals assessing patients’ insight as part of their risk management strategies.8,22
The timing of absconding events also merits discussion. The majority of absconding incidents occurred during daytime hours, particularly between 2:00 PM and 8:00 PM. This finding is consistent with prior research that suggests patients may find it easier to leave during busy periods when staff and visitors are present, thereby reducing the likelihood of being noticed.8,10 This contrasts with other studies that reported a clustering of absconding events during early morning hours, indicating that patterns of absconding may vary significantly across different hospital settings and organizational structures.7,24
Moreover, this study identified that approximately 10% of absconding patients had a history of previous absconding incidents. This finding is lower than that of Meehan et al,25 who reported that one-third of absconders had prior absconding experiences. The discrepancy may reflect improvements in psychiatric management and environmental factors that have evolved over time, contributing to a reduction in repeat absconding behaviors.12,26
The study has several limitations. The retrospective design based on CRF reviews may have introduced reporting bias, particularly in subjective assessments of mental status and affect. Additionally, the study did not explore qualitative reasons for absconding, limiting the understanding of patient perspectives. The 4-year observation period, while substantial, may not fully capture temporal variations in absconding patterns.
CONCLUSION
Most absconding patients were young males admitted involuntarily, often with irritable or euphoric affect, impaired judgment, and grade 1 insight. Most incidents occurred between 2:00 PM and 8:00 PM, primarily within the first week of admission. Absconding patients had significantly shorter hospital stays and minimal perceptual abnormalities, and few had a prior history of absconding. These incidents highlight the need for early risk identification, improved supervision during high-risk periods, and tailored interventions to address clinical and organizational factors associated with absconding behavior. Future research should include prospective studies with longer observation periods and qualitative designs to better understand absconding behaviors and improve prevention strategies.
Article Information
Published Online: May 13, 2025. https://doi.org/10.4088/PCC.24m03893
© 2025 Physicians Postgraduate Press, Inc.
Submitted: November 19, 2024; accepted January 19, 2025.
To Cite: Kumar V, Batra L, Sharma S. Factors associated with absconding during inpatient care from a psychiatric center: a retrospective observational study. Prim Care Companion CNS Disord 2025;27(3):24m03893.
Author Affiliations: Department of Psychiatry, SMS Medical College and Attached Hospitals, Jaipur, India (Kumar, Batra, Sharma).
Corresponding Author: Vikas Kumar, MD, Department of Psychiatry, SMS Medical College and Attached Hospitals, Jaipur 302004, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Risk assessment: Early identification of patients with irritable or euphoric affect and impaired insight can help mitigate absconding risks.
- Supervision: Increased vigilance during peak hours (2:00 PM–8:00 PM) is critical.
- Therapeutic environment: Enhancing patient autonomy and engagement through structured activities can reduce absconding incidents
References (26)

- Voss I, Bartlett R. Seeking freedom: a systematic review and thematic synthesis of the literature on patients’ experience of absconding from hospital. J Psychiatr Ment Health Nurs. 2019;26(9–10):289–300. PubMed CrossRef
- Campagnolo D, Furimsky I, Chaimowitz G. Absconsion from forensic psychiatric institutions. Int J Risk Recover. 2019;2(2):36–50. CrossRef
- Muir-Cochrane E, Muller A, Oster C. Absconding: a qualitative perspective of patients leaving inpatient psychiatric care. Int J Ment Health Nurs. 2021;30(5):1127–1135. PubMed CrossRef
- Muir-Cochrane E, Mosel K, Gerace A, et al. The profile of absconding psychiatric inpatients in Australia. J Clin Nurs. 2011;20(5–6):706–713. PubMed CrossRef
- Andreasson H, Nyman M, Krona H, et al. Predictors of length of stay in forensic psychiatry: the influence of perceived risk of violence. Int J Law Psychiatry. 2014;37(6):635–642. PubMed CrossRef
- Verma DK, Khanra S, Goyal N, et al. Absconding during inpatient care from a tertiary psychiatric hospital: a comparative study. Indian J Psychol Med. 2020;42(5):456–463. PubMed CrossRef
- Gowda GS, Thamby A, Basavaraju V, et al. Prevalence and clinical and coercion characteristics of patients who abscond during inpatient care from psychiatric hospital. Indian J Psychol Med. 2019;41(2):144–149. PubMed CrossRef
- Gerace A, Oster C, Mosel K, et al. Five-year review of absconding in three acute psychiatric inpatient wards in Australia. Int J Ment Health Nurs. 2015;24(1):28–37. PubMed CrossRef
- Sheikhmoonesi F, Kabirzadeh A, Yahyavi ST, et al. A prospective study of patients absconding from a psychiatric hospital in Iran. Med Glas (Zenica). 2012;9(2):345–349. PubMed
- Kaggwa MM, Acai A, Rukundo GZ, et al. Patients’ perspectives on the experience of absconding from a psychiatric hospital: a qualitative study. BMC Psychiatry. 2021;21(1):371. PubMed CrossRef
- Whitecross F, Lee S, Bushell H, et al. Implementing a psychiatric behaviours of concern team can reduce restrictive intervention use and improve safety in inpatient psychiatry. Australas Psychiatry. 2020;28(4):401–406. PubMed CrossRef
- Muir-Cochrane E, Oster C, Grotto J, et al. The inpatient psychiatric unit as both a safe and unsafe place: implications for absconding. Int J Ment Health Nurs. 2013;22(4):304–312. PubMed CrossRef
- Lang U, Hartmann S, Schulz-Hartmann S, et al. Do locked doors in psychiatric hospitals prevent patients from absconding? Eur Psychiatry. 2010;24(4):218–224.
- Simpson AI, Penney SR, Fernane S, et al. The impact of structured decision making on absconding by forensic psychiatric patients: results from an A-B design study. BMC Psychiatry. 2015;15:103. PubMed CrossRef
- Moradpour M, Amiresmaili M, Nekoei-Moghadam M, et al. The reasons why patients abscond from public hospitals in southeastern Iran: a qualitative study. Arch Public Health. 2021;79(1):106. PubMed CrossRef
- Hunt IM, Windfuhr K, Swinson N, et al. Suicide amongst psychiatric inpatients who abscond from the ward: a national clinical survey. BMC Psychiatry. 2010;10(1):14. PubMed CrossRef
- Wilkie T, Penney SR, Fernane S, et al. Characteristics and motivations of absconders from forensic mental health services: a case-control study. BMC Psychiatry. 2014;14(1):91. PubMed CrossRef
- Khammarnia M, Kassani A, Amiresmaili M, et al. Study of patients absconding behavior in a general hospital at southern region of Iran. Int J Health Policy Manag. 2014;4(3):137–141. PubMed CrossRef
- Bowers L, Jarrett M, Clark N. Absconding: a literature review. J Psychiatr Ment Health Nurs. 1998;5:343–353. PubMed CrossRef
- John CJ, Gangadhar BN, Channabasavanna SM. Phenomenology of “escape” from a mental hospital in India. Indian J Psychiatry. 1980;22(3):247–250. PubMed
- Mosel K, Ziaian T, Gerace A, et al. An exploration of absconding behaviours from culturally and linguistically diverse psychiatric hospital patients in Australia. Int J Cult Ment Health. 2010;3(2):96–106. CrossRef
- Yahyavi ST, Faraji S. Absconding from a psychiatric hospital in a developing country, related factors, and the consequences. Med J Islam Repub Iran. 2023;37:110. PubMed CrossRef
- Rivest M. When lay knowledge is a symptom: the uses of insight in psychiatric interventions. Stud Soc Justice. 2022;16(1):245–263. CrossRef
- Nakamura R, Asami T, Yoshimi A, et al. Clinical and brain structural effects of the illness management and recovery program in middle-aged and older patients with schizophrenia. Psychiatry Clin Neurosci. 2019;73(12):731–737. PubMed CrossRef
- Meehan T, Morrison P, McDougall S. Absconding behaviour: an exploratory investigation in an acute inpatient unit. Aust N Z J Psychiatry. 1999;33(4):533–537. PubMed CrossRef
- Mosel KA, Gerace A, Muir-Cochrane E. Retrospective analysis of absconding behaviour by acute care consumers in one psychiatric hospital campus in Australia. Int J Ment Health Nurs. 2010;19(3):177–185. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!