Abstract
Objective: To assess health care providers’ attitudes toward integrating family support into substance use disorder (SUD) treatment plans.
Methods: A cross-sectional survey design was used to evaluate perceptions, use, and challenges of family support in SUD treatment among psychiatry and internal medicine providers. A total of 104 provider participants were involved in the study.
Results: While most providers recognized the benefits of family support in enhancing SUD outcomes and decreasing relapse rates, referrals to these services were limited. Younger practitioners had lower confidence in integrating family support. Psychiatrists were found to have more favorable views relative to internal medicine providers on the efficacy of family support interventions within SUD treatment plans.
Conclusion: Perspectives on family support in SUD treatment varied across age groups and specialties, highlighting gaps in training and practice. The underutilization of family involvement underscores the need for targeted educational initiatives to enhance provider knowledge, confidence, and integration of family-based approaches that may improve patient outcomes.
Prim Care Companion CNS Disord 2026;28(1):25m04030
Author affiliations are listed at the end of this article.
Substance use disorder (SUD) impacts patients, their families, and broader society, with economic and social consequences. The COVID-19 pandemic also exacerbated substance misuse due to widespread economic and social disruptions.1 While a wide range of tools are available for treating SUD, physicians acknowledge its complex nature and the importance of incorporating integrative approaches that include both family-based support and active family member involvement in the treatment process. The goal of family member involvement in SUD treatment is to enhance the recovery process through fostering a supportive environment. Evidence from studies underscores the efficacy of family-based interventions in SUD treatment, revealing reductions in substance use and improvements in treatment adherence.2–4 Although the benefits of integrating family support into SUD treatment plans are recognized, there is a dearth of research regarding the perceptions and attitudes of clinicians toward the utility and effectiveness of family-based interventions in SUD treatment frameworks.
This study explores clinicians’ perspectives on the efficacy of family support services as a component of holistic treatment strategies for patients with SUD. We hypothesize that clinicians treating patients with SUD have knowledge gaps regarding the impact of family support on patient outcomes and its integration into treatment. Assessing their understanding will inform targeted education, resources, and training to improve implementation. Enhanced clinician knowledge and training can aid physicians in more effectively incorporating family-based treatments into SUD management strategies, enhancing both the recovery process and outcomes for patients with SUDs.
METHODS
Study Design and Instrumentation
A quantitative, cross-sectional survey was utilized to explore health care provider perspectives on family support in SUD management at a major urban academic center. Questions focused on the impact of family support on patient outcomes, treatment adherence, and relapse rates, in addition to provider confidence and perceived challenges to integration of these services into SUD care.
Participants, Inclusion and Exclusion Criteria, and Recruitment
Health care providers in psychiatry and internal medicine departments at a major urban academic center were the study’s target population. Inclusion criteria included professional designation as MD, DO, or nurse practitioner; English proficiency; and age ≥18 years. The exclusion criterion was nonconsent, indicated by discontinuation of the survey. Email listservs were utilized to send an email invitation to a Qualtrics survey.
Data Collection and Analysis
Data were collected anonymously utilizing the Qualtrics platform. Descriptive statistics for demographic and attitude items were calculated for the whole sample, and attitude items were compared between demographic groups and provider specialties using a 2-sided χ2 test or a Fisher exact test as appropriate. Analyses were performed using the R programming language, and α = .05 was used as the significance level.
Family Support Referral
At our institution, family support referrals are facilitated through the Department of Psychiatry, specifically via the Support, Advocacy, and Family Education (SAFE) program. SAFE offers families an initial consultation with an addiction psychiatrist, peer and group support, and access to educational resources. Additional referrals may also be made through hospital social work services, which could connect families with additional community-based counseling. SAFE participation is voluntary and free of charge, while external referrals may vary in payment structure.
RESULTS
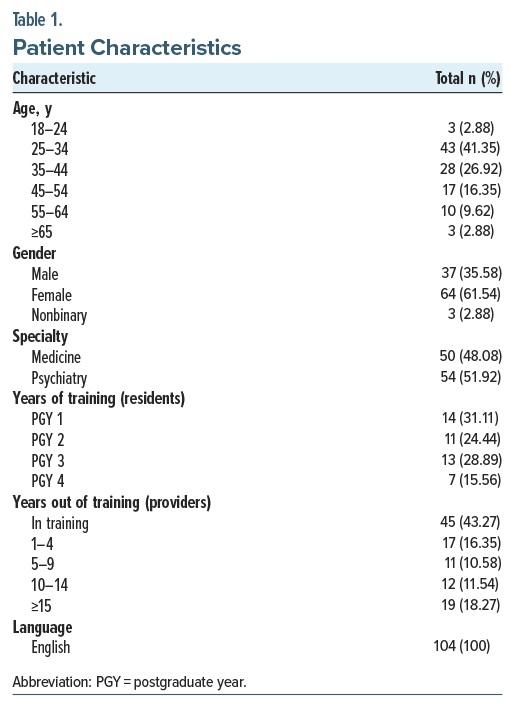
There were 104 survey participants, primarily aged 25–34 (41.35%) years and mostly female (61.54%). The respondents were close to being evenly split between medicine (48.08%) and psychiatry (51.92%) specialties. A little less than half of the respondents (43.27%) were still in training. Table 1 shows participant characteristics.
Overall Trends
Many providers reported encountering patients with SUDs on a regular basis, with 44.23% seeing them daily and 49.04% a few times per week. However, patient family interactions were less frequent, with 50% of participants engaging occasionally and 25.96% engaging frequently. Despite infrequent family interactions, respondents overwhelmingly considered family support services to be critical for SUD care (95.19%), and a majority believed that family support services improve patient outcomes (92.31%), contribute to increased treatment compliance and adherence (86.54%), and decrease relapse rates (65.38%). However, family support referrals remain rare (73.08% rarely refer). Mixed responses were received regarding the evidence of efficacy of family support services, with 72.12% agreeing that there is adequate evidence. Nonetheless, there is a strong consensus (91.35%) that family support should be included as an element of SUD treatment plans. About 63.64% of participants were neutral or disagreed that they felt confident incorporating family support into SUD plans; 76.92% recognized that introducing these services may bring new challenges to SUD treatment dynamics.
Age and Gender Comparisons
When analyzing by age, both groups endorsed the idea that family support reduces relapse rates. Older respondents showed greater trust in the evidence supporting these services, with 81.03% in agreement compared to 60.87% of younger respondents (P=.023). Regarding integration of family support into treatment, 46.55% of older respondents felt confident in their ability to incorporate these services into a treatment plan, significantly higher than the 23.91% among younger practitioners (P=.017). Gender analysis shows broad support for family involvement, with females (96.88%) expressing stronger agreement (P=.049) than males (83.78%).
Specialty Differences
Segmenting health care providers by specialty revealed significant differences between medicine and psychiatry providers. Psychiatric providers encountered SUD patients more frequently than internal medicine providers (59.26% vs 28%, P<.001) and interacted with family members of SUD patients more often (42.59% vs 8%, P<.001). They also showed greater support for family involvement, with 100% agreeing that these services improve patient outcomes, relative to 84% of internal medicine providers (P=.002). Psychiatric providers were also more likely to believe that family support improves treatment adherence (98.15% vs 74%, P<.001) and reduces relapse (87.04% vs 42%, P<.001). Additionally, psychiatric providers had greater confidence in the evidence supporting family support services (87.04% vs 56%, P<.001) and in integrating these services into treatment relative to internal medicine providers (59.26% vs 12%, P<.001).
Overall, psychiatrists had more frequent SUD patient and family interactions and more favorable views on the efficacy of family support services in SUD treatment compared to internal medicine providers, highlighting potential gaps in training and implementation.
DISCUSSION
This survey enhances our understanding of health care providers’ beliefs, attitudes, and knowledge levels regarding family support services and family member involvement during SUD treatment. While a majority of providers supported the inclusion of family support in SUD treatment plans, there was uncertainty expressed around the integration of these services, potentially indicating a gap in knowledge or experience. Additionally, older respondents had greater confidence in integration compared to their younger colleagues. Psychiatric providers also had more daily encounters with SUD patients and their families, were more likely to recognize the benefits of family support in patient outcomes, and had greater confidence in integration of family support into treatment plans compared to their internal medicine colleagues.
Although a significant proportion of health care providers regularly encounter SUD patients, engagement with families is less frequent, potentially affecting their inclusion in treatment decisions. While family support services are widely recognized for improving adherence and outcomes and reducing relapse, referrals remain low. Providing education about available resources and conducting additional research to understand barriers to referral could help identify specific challenges.
Frequent encounters with SUD patients correlated with greater support for family involvement, improved patient outcomes, and increased confidence in integration of family support services into treatment plans. Regular interaction with SUD patients and families appears to enhance provider perceptions of the efficacy of family support services. As shown in the age gap analysis, younger providers may lack confidence in integrating family support services into SUD treatment. Simulations, case studies, and additional training could enhance their comfort, allowing for more consistent care across providers.5,6
Notable differences exist between psychiatry and internal medicine practitioners, with psychiatrists more likely to value and trust the efficacy of family support services as a component of SUD treatment plans. This difference may stem from the psychosocial focus that may be more prevalent during psychiatry residency training. Additional education on the psychosocial aspects of care could help bridge this perception gap across specialties.
There were limitations in conducting this study. The generalizability of the data is challenged by focusing on providers from a major urban academic center, limiting generalizability of these results to other settings such as rural environments. Selection bias must also be considered, as providers interested in family support may have been more likely to respond than those who are unfamiliar.
Overall, there is a consensus on the value of family support in SUD treatments, but barriers, such as lack of differing perceptions across specialties and insufficient training among young providers, impede its widespread integration. By providing greater education and resources on utilizing the psychosocial model of treating SUD patients, we can begin to take steps toward improving the management of SUD patients and better integrate family support services into their treatment plans.
Article Information
Published Online: January 6, 2026. https://doi.org/10.4088/PCC.25m04030
© 2026 Physicians Postgraduate Press, Inc.
Submitted: June 22, 2025; accepted October 15, 2025.
To Cite: Anand S, Romano N, Knight R, et al. Exploring health care provider knowledge and perceptions of family support for patients with substance use disorders. Prim Care Companion CNS Disord 2026;28(1):25m04030.
Author Affiliations: Department of Psychiatry, Weill Cornell Medical College, New York, New York (Anand, Romano, Knight, Makovkina, Avery); Department of Population Health Sciences, Weill Cornell Medical College, New York, New York (Qiu).
Corresponding Author: Sahil Anand, BA, 1300 York Ave, New York, NY 10065 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Family inclusion in substance use disorder treatment improves patient outcomes, but provider referrals remain limited; health care providers should prioritize connecting patients with available family support resources.
- Psychiatrists and more experienced providers reported greater confidence in integrating family support, while internal medicine and younger clinicians expressed lower comfort, highlighting the need for targeted training and educational resources to strengthen utilization of family-based approaches in these groups.
References (6)

- Chacon NC, Walia N, Allen A, et al. Substance use during COVID-19 pandemic: impact on the underserved communities. Discov (Craiova, Romania). 2021;9(4):e141. PubMed CrossRef
- Hartnett D, Carr A, Hamilton E, et al. The Effectiveness of functional family therapy for adolescent behavioral and substance misuse problems: a meta-analysis. Fam Process. 2017;56(3):607–619. PubMed CrossRef
- Esteban J, Suárez-Relinque C, Jiménez TI. Effects of family therapy for substance abuse: a systematic review of recent research. Fam Process. 2023;62(1):49–73. PubMed CrossRef
- Hogue A, Schumm JA, MacLean A, et al. Couple and family therapy for substance use disorders: evidence-based update 2010-2019. J Marital Fam Ther. 2022;48(1):178–203. PubMed CrossRef
- Downar J, McNaughton N, Abdelhalim T, et al. Standardized patient simulation versus didactic teaching alone for improving residents’ communication skills when discussing goals of care and resuscitation: a randomized controlled trial. Palliat Med. 2017;31(2):130–139. PubMed CrossRef
- Harrington AW, Oliveira KD, Lui FY, et al. Resident education in end-of-life communication and management: assessing comfort level to enhance competence and confidence. J Surg Educ. 2020;77(2):300–308. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!