Factitious disorder (FD), also known as Munchausen syndrome, is a psychiatric condition characterized by the deliberate fabrication or exaggeration of medical or psychological symptoms, often without an apparent external reward. Individuals affected by FD may employ various methods to simulate or induce illness, including falsification, simulation, and the deliberate induction of symptoms. While a genuine medical condition may occasionally coexist, the deceptive behaviors or self-inflicted harm linked to this disorder result in others perceiving the individual as more seriously ill or impaired than they are, often leading to unnecessary interventions.1–3 It is important to emphasize that most of the published literature on FD consists of case reports and series, which, while valuable, may present a misleading clinical picture of the disorder when separately considered.4
Factitious presentations have been documented globally, across all medical specialties and age groups. However, due to its inherently deceptive nature, FD is regarded as one of the most diagnostically challenging conditions encountered in clinical practice. A definitive diagnosis of FD is rarely made with certainty. When achieved, an extensive series of medical investigations are often followed to exclude organic causes for the patient’s symptoms.2,3
Although clinicians have recognized FD for centuries, the first comprehensive study of the disorder emerged with Asher’s seminal 1951 description of Munchausen syndrome.5 In his report, Asher applied the term Munchausen to cases of chronic factitious behavior, characterizing it as a common syndrome that most doctors have encountered, yet little has been documented.2,3
In clinical practice, most physicians are likely to encounter at least 1 patient with FD. However, the precise prevalence of FD within hospital settings remains uncertain. Estimates suggest that FD accounts for approximately 0.6%–3% of referrals from general medicine to psychiatry and between 0.02% and 0.9% of cases assessed in any medical specialty clinic. Determining the true prevalence is further complicated because health care professionals often fail to document the diagnosis, even in confirmed cases.1,2 This disorder is associated with a high economic burden for health systems; an Italian article concluded that the National Health System’s expenditures for each patient ranged between 50,000 and 1 million euros.6 Early detection of FD is therefore important, not only to reduce the unnecessary expenditure of health care resources but also to minimize potential patient harm.3
The course of FD, according to the DSM-5, typically follows a pattern of intermittent episodes, with onset most commonly occurring in early adulthood, often triggered by a prior hospitalization for a medical or psychiatric condition. In individuals who experience recurrent episodes of symptom falsification, this pattern of repeated deceptive interactions with health care professionals, including frequent hospitalizations, may persist throughout their lifetime.1
Psychodynamically oriented explanations are important for understanding and treating Munchausen syndrome. Adverse childhood experiences, such as unstable family environments and instances of physical or sexual abuse, have been proposed as significant factors contributing to the disorder’s development.7–9
Moreover, the association between FD and personality disorders, particularly borderline personality disorder, is widely cited in the professional literature and has been included in numerous review articles.7,10 However, a systematic review conducted by Yates and Feldman,2 analyzing the largest sample of patients with FD to date, revealed that comorbid psychiatric disorders were assessed in only 37% of the cases. Among these, the most prevalent comorbid disorder was depression, identified in 41.8% of patients. Other frequently diagnosed conditions included personality disorders (16.5%), substance abuse (15.3%), anxiety disorders (14.7%), functional neurological symptoms (5.3%), and eating disorders (4.1%). Notably, this finding might be influenced by the majority of case studies authored by nonpsychiatrists.2,9
Despite limited attention in the literature, the potential role of cerebral dysfunctions in FD is noteworthy. In a study involving 25 patients classified as having Munchausen syndrome, Pankratz and Lezak11 identified significant neuropsychologic alterations in approximately one-third of their sample, namely, deficits in conceptual organization, management of complex information, and judgment. The authors11 proposed that these neuropsychological impairments may contribute to the aberrant behavior of these patients. Additionally, patients with FD often display characteristics associated with cluster B personality disorders, which may correlate independently with impaired neurocognitive performance. This suggests a potential neuropsychiatric vulnerability within a subset of individuals diagnosed with Munchausen syndrome.8
To our knowledge, no cases of FD with comorbid neurodegenerative disorders have been reported. Given the complex interplay of psychological, cognitive, and potential organic factors in FD, this case report aims to elucidate the diagnostic challenges associated with differentiating FD from aggravating personality disorder or behavioral variant frontotemporal dementia (bvFTD), thereby contributing to a better understanding of this multifaceted disorder.
Case Report
A 58-year-old woman presented to our hospital for psychiatric consultation after a referral from her neurosurgery doctor due to “depressive humor and suicidal ideation.” The patient is a widow and has a 27-year-old adopted daughter. She has lived alone since her daughter recently moved out of the house. She completed the fourth grade and worked as a childhood educator until the age of 27 years. At that time, she retired due to disability, according to the patient “because of fibromyalgia.”
Regarding her family psychiatric history, her mother was diagnosed with Parkinson disease and Alzheimer disease. Her father had a history of suicide by hanging. She also had a maternal uncle with a diagnosis of unspecified dementia before the age of 65 years.
She has a long medical history that includes neutropenia likely secondary to autoimmune disease in evaluation, Sjögren syndrome, fibromyalgia, hypertension, mild mitral regurgitation, dyslipidemia, degenerative spine pathology currently waiting for spondylolisthesis, bilateral shoulder tendinitis submitted to surgery, left hip trochanteritis, mild osteoarthritis of the right knee submitted to surgery, surgery for decompression of the right carpal tunnel, cholecystectomy, partial gastrectomy for severe obesity, and esthetic brachioplasty.
Additionally, her medical records showed multiple uncertain diagnoses due to incompatibility of the symptomatology and the diagnostic tests, namely, major neurocognitive disorder, Parkinson disease, asthma, and rheumatoid arthritis. The patient was being followed in over 50 different medical consultations of multiple medical specialties and was submitted to a large number of medical tests and interventions over the years.
Regarding her neuropsychiatric history, she has been followed in neurology consultation since 2018 for complaints of tremor and frequent forgetfulness. Nonetheless, she had been diagnosed with FTD 2 years before presentation to our hospital.
She was also followed up in psychiatry consultation at a different hospital for several years, with the diagnostic hypothesis of dysthymia and cluster B personality disorder. The medical records show that the former attending psychiatrist already admitted that the patient was likely seeking primary gains—the role of the patient.
The patient was currently taking 17 different medications prescribed by multiple doctors, many of whom she was no longer seeing. Of note, she was taking fluoxetine 40 mg once/d, memantine 20 mg once/d, rivastigmine 9.5 mg once/d, rasagiline 1 mg once/d, and rotigotine 2 mg once/d.
According to her daughter, the patient has always been very quarrelsome, demonstrated low tolerance to frustration, and often lied to take advantage of some situations. She reports a childhood and early adolescence of verbal and physical abuse by her mother who frequently threatened to kill herself. Nonetheless, 3 years ago, she noticed a progressively higher aggressiveness in her mother’s behavior and increasing difficulties in her interpersonal relations, acting rashly and inconsequentially and demonstrating diminished response to other people’s needs and feelings. According to her daughter, the patient has threatened to poison her multiple times; was physically aggressive on various occasions towards her, some neighbors, and unknown people in the street; and has called the police numerous times, reporting physical abuse and theft that was not verified.
Two months before the first psychiatric appointment at our hospital, the patient was hospitalized due to symptomatology compatible with a stroke. Nonetheless, she was discharged without documented muscular strength reduction or other deficits, and a magnetic resonance imaging (MRI) scan of the brain (performed 1 week after the onset of symptoms) showed no findings of acute vascular events. The diagnosis of stroke was not included in the discharge diagnosis. After discharge from the hospital, she kept simulating limb paralysis and received her daughter’s help, who moved back to her mother’s house and later documented by camera the simulation of paralytic symptoms.
Relevant diagnostic tests performed over the years include the following:
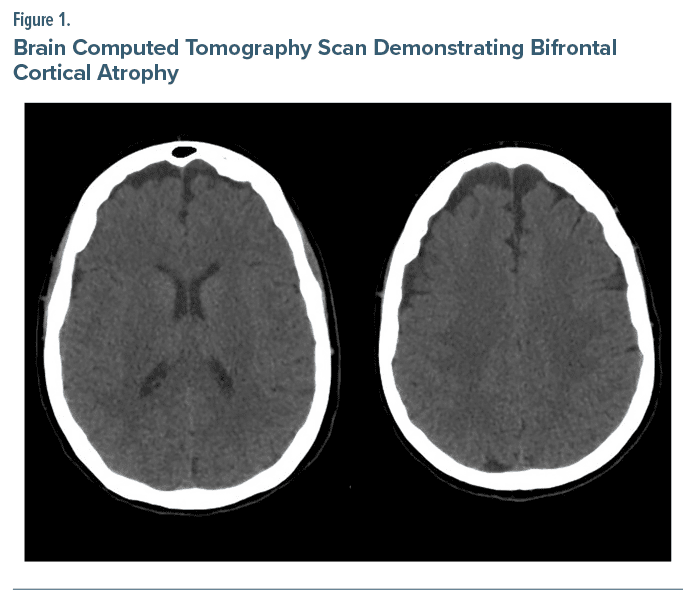
- Brain MRI showing bifrontal cortical atrophy and very mild chronic microangiopathic leukoencephalopathy.
- Neuropsychological evaluation with significant alterations in cognitive-operational functioning predominantly affecting prefrontal areas (executive functions).
- Lumbar puncture without significant protein tau or beta amyloid values.
- Brain computed tomography showing bifrontal cortical atrophy (Fig. 1).
- Frontal Assessment Battery12 10/18 with severely impaired inhibitory control and lexical fluency and moderately impaired motor series.
In consultation at our hospital, she appeared to simulate dysarthria (inconsistent and incongruent articulation changes). Her speech was centered on the interpersonal conflict with her daughter, who became independent and moved in with her boyfriend about 1 month before the episode leading to the suspected stroke. At our observation, the patient displayed overvalued ideas with persecutory content directed at her daughter’s boyfriend and a reduced affective range of emotions. Psychotic symptoms were excluded. She had no insight regarding her neuropsychiatric symptomatology. We introduced quetiapine prolonged release titrated up to 150 mg with the intention of further titration for impulse control and plan to keep monitoring the clinical evolution of the patient.
Discussion
The patient presented here fits the diagnosis of severe cluster B personality disorder with dependent characteristics and FD/Munchausen syndrome, with significant consumption of health resources over several years due to multiple complaints incompatible or incongruent with clinical observations and diagnostic tests. We suspect primary and secondary gains for her factitious symptomatology. However, there seems to be a more recent exacerbation of her usual functioning, namely, behavioral disinhibition, and loss of sympathy and empathy, suggestive of the diagnosis of FTD, which was supported by imaging and neuropsychological assessment.
bvFTD is characterized by early personality changes, behavioral disinhibition, apathy, loss of empathy or interpersonal warmth, and deficits in executive function. Initially, these symptoms may be subtle, but behavioral abnormalities become increasingly problematic. Diagnosis of bvFTD is challenging due to the limited accuracy of neuroimaging in the early stages and the absence of molecular biomarkers, relying predominantly on clinical assessment. Establishing the differential diagnosis can be challenging considering that bvFTD shows significant symptomatic overlap with nondegenerative primary psychiatric disorders. Nonetheless, the later age at onset and difficulties in psychiatric diagnosis criteria fulfillment should direct us to the hypothesis of bvFTD instead of a primary psychiatric disorder.
This case illustrates the difficulty faced by clinicians in recognizing FTD in a patient presenting with long term psychiatric symptoms. Additionally, we emphasize the lower bvFTD diagnosis accuracy in patients with FD with decades of evolution, due to lower reliability of clinical assessment. Finally, if a patient is presenting outside mental health departments with multiple incongruent and inexplicable symptoms, we recommend talking to a psychiatrist. It is important to collect information from the patient’s family and close relatives to check for veracity and congruency of the symptomatology to avoid unnecessary interventions, diagnoses, and therapeutics.
Article Information
Published Online: May 15, 2025. https://doi.org/10.4088/PCC.24cr03901
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(3):24cr03901
Submitted: December 8, 2025; accepted January 29, 2025.
To Cite: Fernandes AM, Albuquerque SF, André R, et al. Is it Munchausen or is it dementia? Prim Care Companion CNS Disord 2025;27(3):24cr03901.
Author Affiliations: Psychiatry and Mental Health Service, Unidade Local de Saúde de Santa Maria, Lisbon, Portugal (all authors).
Corresponding Author: Ana Monteiro Fernandes, MD, Psychiatry and Mental Health Service, Unidade Local de Saúde de Santa Maria, Av Prof. Egas Moniz, Lisbon, Portugal 1649-035 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect patient anonymity.
References (12)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th ed., text rev.). American Psychiatric Association; 2022.
- Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20–28. PubMed CrossRef
- Feldman MD, Eisendrath SJ. The Spectrum of Factitious Disorders. American Psychiatric Association; 1996.
- Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160(6):1163–1168. PubMed CrossRef
- Asher R. Munchausen’s syndrome. Lancet. 1951;257(6650):339–341. PubMed CrossRef
- Onofrj M, Digiovanni A, Ajdinaj P, et al. The factitious/malingering continuum and its burden on public health costs: a review and experience in an Italian neurology setting. Neurol Sci. 2021;42(10):4073–4083. PubMed CrossRef
- Taylor S, Hyler SE. Update on factitious disorders. Int J Psychiatry Med. 1993;23(1):81–94. PubMed CrossRef
- Diefenbacher A, Heim G. Neuropsychiatric aspects in Munchausen’s syndrome. Gen Hosp Psychiatry. 1997;19(4):281–285. PubMed CrossRef
- Goldstein AB. Identification and classification of factitious disorders: an analysis of cases reported during a ten year period. Int J Psychiatry Med. 1998;28(2):221–241. PubMed CrossRef
- Steel RM. Factitious disorder (Munchausen’s syndrome). J R Coll Physicians Edinb. 2009;39(4):343–347. PubMed CrossRef
- Pankratz L, Lezak MD. Cerebral dysfunction in the Munchausen syndrome. Hillside J Clin Psychiatry. 1987;9(2):195–206. PubMed
- Dubois B, Slachevsky A, Litvan I, et al. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000 Dec 12;55(11):1621–1626. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!