Electroconvulsive therapy (ECT) is a safe, effective, and underutilized treatment for multiple psychiatric conditions.1 However, delirium is a common complication of ECT. Acute postictal delirium (<1 hour) has been reported in 18% of patients,2 with a subgroup (5.7%) experiencing disorientation up to 24 hours after treatment.3 In rare cases, delirium can be prolonged, lasting 3 days or more. We present one of the few reported cases of prolonged ECT-associated delirium, offering insights into the proposed pathophysiology.
Case Report
The patient is a 65-year-old white woman with a 9-year psychiatric history of major depressive disorder (MDD) and generalized anxiety disorder and a medical history of hypertension and early-onset Alzheimer dementia with behavioral disturbance. After developing severe MDD refractory to medication management, including adequate trials of fluoxetine, sertraline, aripiprazole, buspirone, and olanzapine, she was referred for ECT. At the time of treatment, the patient was taking sertraline 150 mg/day and olanzapine 2.5 mg nightly. While there was reported improvement in her mood after the first 3 unilateral ECT treatments, the following 3 resulted in escalating periods of acute, fluctuating mental status changes, resolving within a few hours. The fourth treatment resulted in an entire evening of fluctuating cognition, and after the fifth treatment, the patient was unable to recognize her husband for 2 days. There was no modification of ECT parameters or medications during treatment. Following an additional ECT treatment, the patient presented to the ED for escalating auditory and visual hallucinations over the previous 72 hours.
Electroencephalogram performed at this time was significant for moderate-to-severe diffuse background slowing. ECT was subsequently discontinued. During admission, the patient’s medical workup, including urinalysis, comprehensive metabolic panel, thyroid-stimulating hormone, serum anti-NMDA antibody level, and head computed tomography, was unremarkable. It was concluded that the patient’s delirium was secondary to her recent ECT, and she was treated with quetiapine 25 mg every 8 hours as needed for agitation. Her cognition and behavior improved to baseline over the next 5 days, totaling 8 days of delirium following her sixth and final ECT session.
Discussion
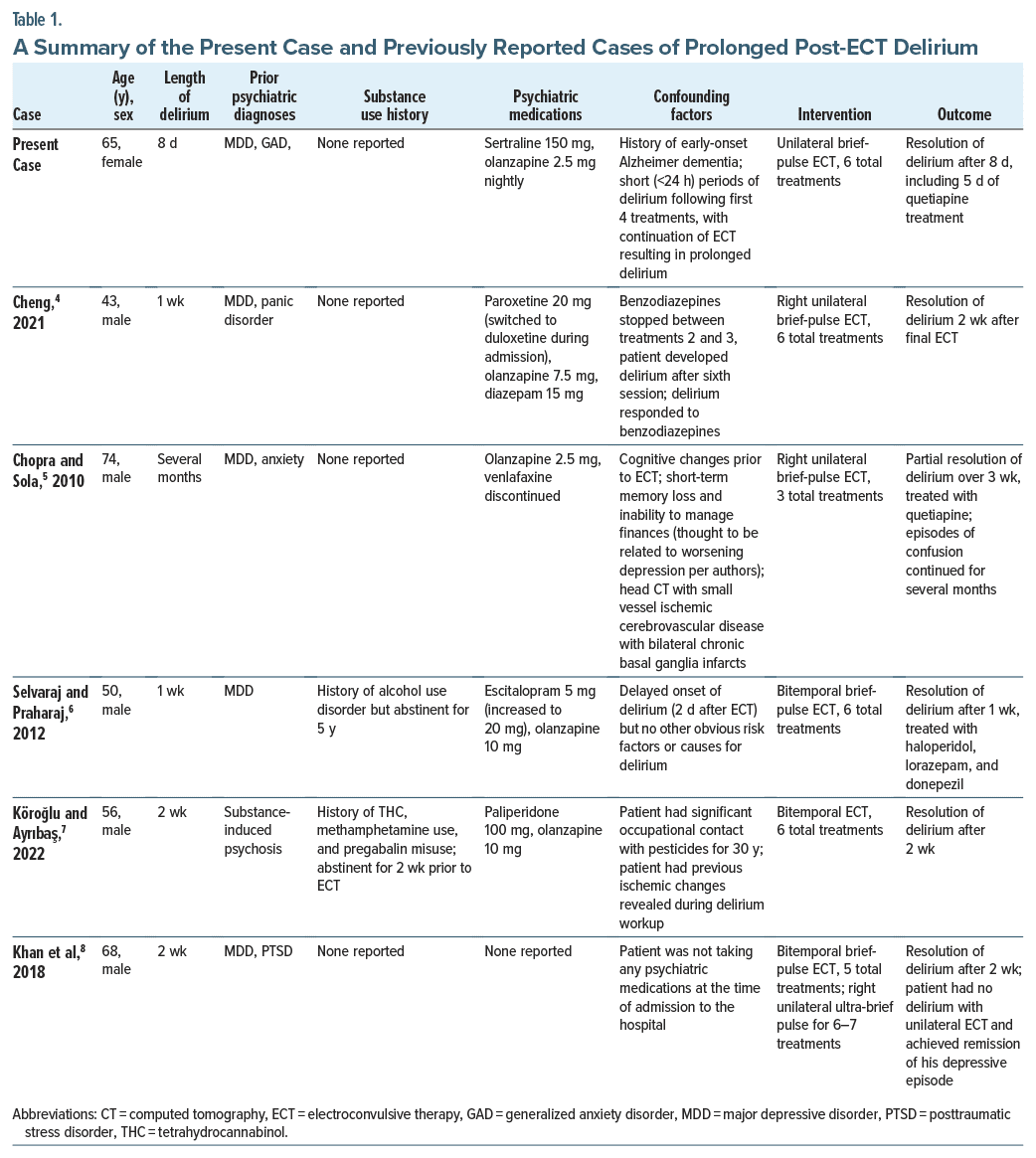
Prolonged delirium following ECT is rare. Five cases of prolonged delirium related to ECT (3+ days following ECT) have been reported (Table 1). These cases demonstrate a rare but consistent pattern wherein patients develop prolonged delirium after their third or fourth ECT treatment. In most cases, ECT was discontinued, although Khan et al8 described successful unilateral treatment following recovery from delirium induced by bilateral ECT. Unlike other reported cases, the patient presented here continued to undergo ECT and subsequently continued to have escalating periods of delirium. This exacerbation may result from kindling, where repeated electrical or chemical insults can result in behavioral changes over time. This phenomenon was first described in 1998, when researchers noted that repeated episodes of alcohol withdrawal led to a persistent hyperexcitable state that caused behavioral dysregulation.9
Hypothetically, this phenomenon can extend to ECT, where hyperexcitability and hypersynchrony of brain activity may make patients susceptible to delirium with repeated treatments. Kindling provides a novel means of conceptualizing prolonged ECT delirium, especially in cases in which symptoms escalate with further treatment. Each subsequent event of central nervous system excitation could have further exacerbated the patient’s hyperexcitable state. This case suggests that caution should be applied in prolonged postictal delirium and that continued ECT may further exacerbate this risk. Delirium is associated with a prolonged hospital stay, development or worsening of cognitive impairment, and increased mortality; therefore, it is critical to mitigate the risk for delirium.10
In cases of prolonged delirium following ECT, it may be necessary to space out treatments, modify medication regimens, or discontinue treatment altogether. Continued investigation into the link between ECT and prolonged delirium is essential in understanding risk factors for this complication and determining when it is appropriate to terminate an ECT course.
Article Information
Published Online: May 20, 2025. https://doi.org/10.4088/PCC.24cr03888
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(3):24cr03888
Submitted: November 7, 2024; accepted February 5, 2025.
To Cite: Hill GW, Luzum NR, Shah K, et al. Progressive prolonged delirium after electroconvulsive therapy. Prim Care Companion CNS Disord 2025;27(3):24cr03888.
Author Affiliations: Wake Forest University School of Medicine, Winston-Salem, North Carolina (Hill); Department of Psychiatry, Wake Forest University School of Medicine, Winston-Salem, North Carolina (Luzum, Shah, Munjal).
Corresponding Author: Nathan R. Luzum, MD, Department of Psychiatry, Wake Forest University School of Medicine, 1 Medical Center Blvd, Winston-Salem, NC 27103 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect patient confidentiality.
References (10)

- Espinoza RT, Kellner CH. Electroconvulsive therapy. N Engl J Med. 2022;386(7):667–672. PubMed CrossRef
- Logan CJ, Stewart JT. Treatment of post-electroconvulsive therapy delirium and agitation with donepezil. J ECT. 2007;23(1):28–29. PubMed CrossRef
- Grover S, Kumar A, Chakrabarti S, et al. The incidence of prolonged post-electroconvulsive therapy delirium: a retrospective study. Indian J Psychiatry. 2020;62(2):193–197. PubMed CrossRef
- Cheng K. Confusion and psychosis-like symptoms after ECT: benzodiazepine withdrawal or prolonged post-ECT delirium? Psychiatric Annals. 2021;51(11):536–539. CrossRef
- Chopra A, Sola CL. A case of prolonged interictal ECT-induced delirium. J Neuropsychiatry Clin Neurosci. 2010;22(2):E32–E33. PubMed CrossRef
- Selvaraj AG, Praharaj SK. Delayed onset and prolonged interictal delirium following electroconvulsive therapy. Psychogeriatrics. 2012;12(3):211–213. PubMed CrossRef
- Köroğlu E, Ayrıbaş B. Prolonged post-ECT delirium associated with substance-induced psychosis: a case report. Perspect Psychiatr Care. 2022;58(4):3103–3105. PubMed CrossRef
- Khan AR, Mahmood H, Wasiq S, et al. Prolonged post-electroconvulsive therapy delirium: an unusual presentation. Cureus. 2018;10(8):e3221. PubMed CrossRef
- Becker HC. Kindling in alcohol withdrawal. Alcohol Health Res World. 1998;22(1):25–33. PubMed
- Maldonado JR. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Crit Care Clin. 2017;33(3):461–519. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!