Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(1):24f03831
Author affiliations are listed at the end of this article.
Have you ever wondered if people can develop posttraumatic stress disorder (PTSD) due to their bout with psychosis and its treatment? Have you been uncertain about when and how to evaluate and treat a patient with signs and symptoms of PTSD, such as nightmares and hypervigilance, in the context of psychosis? If you have, then the following case vignette and discussion should prove useful.
CASE VIGNETTE
Mr A, a 26-year-old man with a history of childhood trauma and schizophrenia (which had required 3 inpatient psychiatric admissions in the past 2 years), presented to the emergency department (ED) of a community hospital at the bidding of his grandfather (who lives with him). At the age of 10 years, Mr A was a passenger in a motor vehicle collision in which he experienced the traumatic loss of both his parents. Mr A had discontinued his antipsychotic medication several months earlier, and as a result, he had become increasingly reclusive, refused most meals, and slept little, as he felt the need to remain ever watchful. He had become afraid that the air vents in his home were being used to poison him with toxic gas. He heard voices that told him that people were trying to kill him.
In the ED, Mr A appeared guarded; he kept his eyes on the hallway throughout his assessment. With the encouragement of his grandfather, Mr A recounted that toxic gas was traveling through the air vents; this contributed to his intense desire to leave the ED. His grandfather explained that on several occasions, Mr A had been placed in restraints due to unsafe behavior triggered by his hallucinations and paranoia. The grandfather also reported that Mr A had several brief episodes at home when he awoke, yelling that someone was trying to kill him with toxic gas. He had been quick to startle even when his symptoms were under control, especially when his nightmares were frequent.
DISCUSSION
What Is PTSD?
PTSD develops after someone is exposed to actual or threatened death, serious injury, or sexual violence via direct exposure, witnessing the event in person, learning that it happened to a close family member or friend, or being repeatedly exposed to stressful reminders of past events. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision,1 PTSD is characterized by symptoms in 4 clusters: intrusions, avoidance, impaired cognition and mood, and alterations in arousal and reactivity. PTSD is one of the most highly prevalent psychiatric disorders, affecting approximately 5% of individuals in any given year and 6% of individuals during their lifetimes.2 PTSD is especially common among women, who have a prevalence twice that of men, and among highly trauma-exposed populations (eg, military veterans and first responders). It is also frequently comorbid with other psychiatric conditions, such as substance use disorders and mood disorders.2
What Is Psychosis-Related PTSD?
Broadly speaking, psychosis refers to a state, borne from a bevy of etiologies, in which there is impaired reality testing. More narrowly, the World Health Organization and the American Psychiatric Association have defined psychosis as an impairment of reality testing, which occurs because of delusions, hallucinations without insight, or hallucinations without insight and delusions.1,3 The experience of delusions and hallucinations varies dramatically among patients; fortunately, most perceptual experiences are viewed as non–life threatening. However, derealization and hallucinations, acute emotional distress, disorganized behaviors, and their treatment may each be traumatic.4,5 Psychosis-related PTSD arises when individuals meet criteria for PTSD due to psychotic symptoms and/or the experiences associated with the treatment of psychosis.
Can Psychotic Symptoms Meet Criterion A for PTSD?
In PTSD, criterion A in the DSM-5 provides the definition of a traumatic event, ie, the “exposure to actual or threatened death, serious injury, or sexual violence” with direct exposure, witnessing trauma, learning that something traumatic has happened to a close relative or friend, or indirect exposure to frightening details of the trauma, usually in the course of professional duty.1 While clarifying the nature of traumatic experiences has been controversial,6 traumatic experiences related to psychotic symptoms or their treatment can clear the threshold required to be considered as meeting criterion A for PTSD-associated trauma.1 In the setting of impaired reality testing, psychotic symptoms, such as persecutory delusions and hallucinations, are perceived as no less real than actual threats.
Can Treatments For, and Associated With, Psychosis Be Traumatic?
Individuals who have had a psychotic episode often experience a threat to their well-being during their hospitalization that may lead to the development of PTSD symptoms.7 When patients were interviewed (N=395) 10 years after their first psychotic episode, roughly two thirds (69%) of them reported that their psychiatric hospitalization was traumatic.4 The interview sought to identify an association between perceived trauma as well as distressing or coercive experiences during psychiatric hospitalization. Perceived trauma was more common in women than in men, and in homemakers more than those who were employed full time. However, forced medication was associated with less time in treatment, especially for those with schizophrenia and schizophrenia-spectrum disorders. In addition, coercive experiences were associated with less time in treatment. The investigators concluded that the perception of trauma during a psychiatric hospitalization was common, although it was not reliably related to treatment participation.
How Often Does Psychosis Develop in Those With PTSD?
Chronic PTSD with psychotic features was first described in a combat population in 1981.8 A literature review in 2003 assessed the prevalence of comorbid psychosis in veterans with combat-related PTSD.9 It was determined that comorbid psychosis affected 20%–40% of veterans with PTSD. However, the authors9 discussed the possibility that the prevalence of psychosis was inflated due to poor differentiation of PTSD symptoms from positive and negative symptoms of schizophrenia. Other investigators who reviewed data from the National Comorbidity Study found that having a diagnosis of PTSD increased the likelihood (from 2.45 to 4.22 times) that patients would endorse any of the 8 psychosis screening items.10 These studies highlighted the higher prevalence of psychosis among individuals with PTSD; however, clinicians often have difficulty differentiating symptoms of PTSD and schizophrenia.
What Is the Prevalence and Relationship of PTSD in Those With a Psychotic Disorder?
A systematic review of 38 studies found a widely divergent prevalence rate (0%–55%) of PTSD in patients with schizophrenia; 30 of those studies reported a prevalence greater than 10%.11 Such variability in prevalence rates likely not only reflects the challenge in differentiating PTSD symptoms from positive and negative symptoms of psychotic disorders9,12 but also highlights a lack of a universal and validated screening tools for PTSD in those with psychotic disorders.
What Is the Prevalence of Psychosis Related PTSD?
A 2021 review article13 analyzed research articles that reported prevalence rates and associated factors of psychosis-related PTSD. The authors13 found a prevalence rate of 14%–47% for individuals with psychosis who met criteria for PTSD. Although these prevalence rates refer to patients who experienced a psychosis-related trauma, the investigators noted that there was a lack of distinction between trauma that was related to the treatment for psychosis and trauma related to psychotic symptoms.
Are Vulnerable Populations More Susceptible to Developing PTSD Related to Psychosis?
Some vulnerable populations (eg, those experiencing racial disparities in psychiatric care) may be more susceptible to the development of PTSD related to psychosis. For example, a retrospective cohort study of 12,977 unique encounters of adults receiving emergency psychiatric services at a large academic medical center showed that Black patients were more likely to be physically (adjusted odds ratio [AOR] = 1.35; 95% CI, 1.07–1.72) and chemically (AOR = 1.33; 95% CI, 1.15–1.55) restrained than White patients after adjusting for measured confounders.14 Given that coercive interventions may increase one’s risk for developing PTSD, further work is needed to elucidate when disparities affect the provision of equitable and accessible psychiatric care.14
Moreover, racial and sexual minorities are at a higher risk of developing both psychosis and PTSD during their lifetimes.15–18 Adverse childhood experiences (ACEs) are also associated with a higher likelihood of developing PTSD and psychosis.19,20 In addition, childhood trauma increases the likelihood (by 27 times) of developing psychosis-related PTSD after a first psychotic episode.21 Given that racial and sexual minorities experience ACEs at higher rates than those in the general population,22,23 ACEs may place racial and sexual minorities at a higher risk for developing PTSD and psychosis. The Adverse Childhood Experiences Questionnaire24 is a widely used scale that assesses physical, emotional, and sexual abuse and household dysfunction (eg, alcohol or drug misuse, having a parent who engaged in violent or criminal behavior in the household, and mental illness in the family).
Does the Assessment of PTSD Differ in the Face of Psychosis?
A systematic review on the assessment of trauma and related symptoms revealed that most patients who have received mental health services are never asked about exposure to trauma, and inquiries about trauma were even less likely to occur in those who experienced psychosis.25 Clinicians often fear that asking about trauma may exacerbate the risk, worsen distress, or increase psychotic symptoms; although studies have shown that patients often anticipate these questions despite the risk for transient distress, not having the opportunity to discuss trauma and its connections to psychosis creates negative consequences for patients. As for the content of the evaluation, providers should recognize that exploration of traditionally recognized traumas and broad questions regarding “abuse” histories often do not allow for comprehensive responses that reveal a history of psychosis-related trauma. An examination of interviews about life history revealed that more disclosures occurred when self-report measures were used. Several studies explored the utility of existing diagnostic screening tools; the Trauma and Life Experiences (TALE) checklist was notable for its inclusion of psychosis specific elements, although larger sample sizes are necessary to determine its validity.26,27 The TALE checklist included questions related to feeling threatened by psychotic experiences (including hallucinations, paranoid delusions, and contact with mental health care services, such as in hospital settings). The checklist also included questions that may identify traumatic experiences related to psychotic experiences, such as may occur with contact with the legal system. Further research is needed to examine the risk factors associated with the development of psychosis related PTSD. A meta-analysis on the traumatic nature of first-episode psychosis showed that while psychotic symptoms, hospitalization and treatment, uncharacteristic behaviors, paranoia and fear of others, and police involvement were traumatic, there were limited data to determine if sociodemographic factors, clinical or treatment factors, prior trauma, coping styles, or associated substance use were associated with the development of psychosis related PTSD.28
What Does the Treatment of PTSD and Psychosis-Related PTSD Involve?
Early and sustained treatment of PTSD and psychosis-related PTSD is pivotal in improving long-term outcomes. Delays in treatment are associated with exacerbations of both PTSD and psychotic symptoms, as well as decreased functioning and quality of life. Clinicians should also consider the traumatic aspects of treatment, as well as the treatment of comorbid psychiatric illnesses. Many patients with PTSD report having a history of multiple DSM-5 criterion A stressors, often of different types (eg, sexual assault, natural disaster, and military combat). This is of practical importance since it may affect the selection of a therapeutic modality. A systematic review analyzed studies that investigated the effectiveness, tolerability, and acceptability of trauma-focused psychotherapies.29 In addition, several studies found that trauma-focused cognitive-behavioral therapy (CBT),30–32 eye-movement desensitization and reprocessing therapy,33–36 and prolonged exposure33,37 were effective in reducing psychotic symptoms. Each of the interventions that included exposure and measured PTSD symptoms was associated with a significant decrease on PTSD symptom measures. Only 1 uncontrolled study that used trauma-informed CBT found a small but significant decrease on PTSD symptom measures,38 and no studies that used an intervention without exposure found a reduction of psychotic symptoms.38–40 The authors concluded that exposure, specifically the inclusion of trauma memory reprocessing, was necessary to address psychotic symptoms in the context of trauma.29 These results suggest that psychosocial interventions used to treat PTSD with exposure were most effective in reducing symptoms of PTSD and psychosis.
How Might the Pharmacologic Treatments for PTSD and Psychosis Interact?
Although there is no “magic bullet” for the pharmacologic treatment of PTSD, treatment is aimed at symptom management, including adequate control of psychosis and PTSD-related behaviors. Tools, such as the Brief Trauma Questionnaire,41 the PTSD Checklist for DSM-5,42 and structured clinical interviews, evaluate symptom burden. Treatment options include use of conventional antidepressants, anxiolytics, mood stabilizers, and antipsychotics. For many patients, adequate control of psychosis and PTSD-related symptoms is also critical to functional outcomes. When patients are diagnosed and treated early, this may extend to maintaining employment, family/marital/social relationships, and housing stability/food security.
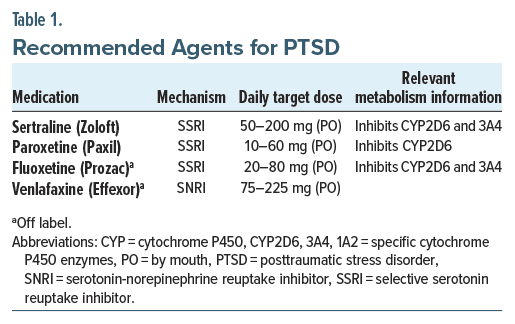
Pharmacologic management of PTSD focuses on the use of serotonergic agents (eg, selective serotonin reuptake inhibitors [SSRIs] such as sertraline and paroxetine and serotonin-norepinephrine reuptake inhibitors [SNRIs]) such as venlafaxine (Table 1), as described in the VA/DoD Clinical Practice Guideline for Management of Posttraumatic Stress Disorder and Acute Stress Disorder (2023),43 which was developed following a systematic review of large clinical and epidemiologic databases. However, additional research into other agents is needed, as there is insufficient evidence for or against the use of alternative SSRIs or SNRIs. However, numerous guidelines recommend the SSRI fluoxetine for the treatment of PTSD.44 When selecting an agent, clinicians should account for a patient’s presentation, their medication history, the drug’s side effect profile, and interactions; SSRIs are often the first-line agents given their wealth of safety, tolerability, and efficacy data. If regular adherence to the medication regimen is in question, fluoxetine, given its extended half-life, should be considered. When used in elderly individuals or those with an elevated body mass index, the highly anticholinergic and weight gain–inducing agent paroxetine should be avoided. Venlafaxine, although it is associated with increases in blood pressure, may be beneficial in those who exhibit predominantly neurovegetative symptoms, given its effects on norepinephrine. Patients should be counseled on the potential for increased anxiety, headache, dizziness, nausea, and sexual dysfunction when using these medications.45 Mirtazapine, a tetracyclic antidepressant, can be used clinically for PTSD-related sleep disturbances and comorbid depressive symptoms. Prazosin, an antihypertensive medication, can be used to treat PTSD-associated nightmares and depressive symptoms. However, neither mirtazapine nor prazosin are recommended in the VA/DoD guideline for PTSD,43 and a randomized control trial testing the effects of prazosin on distressing dreams and sleep quality showed no significant changes posttreatment.46
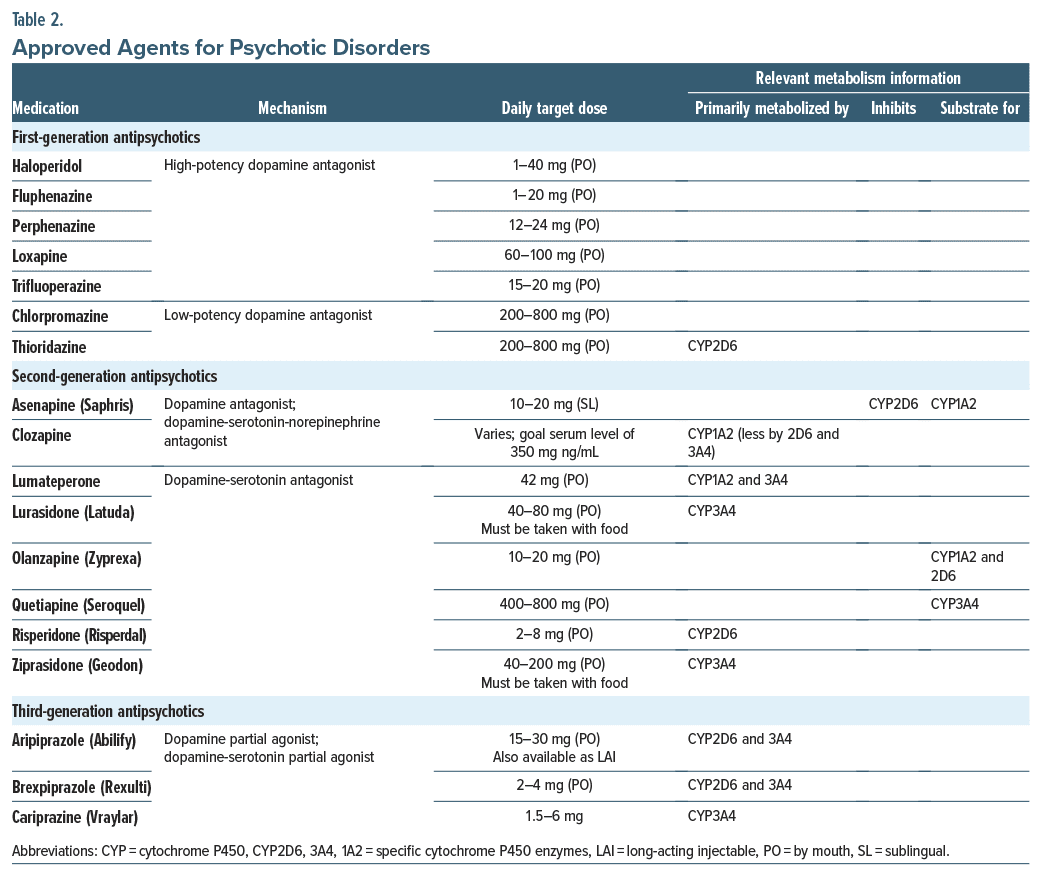
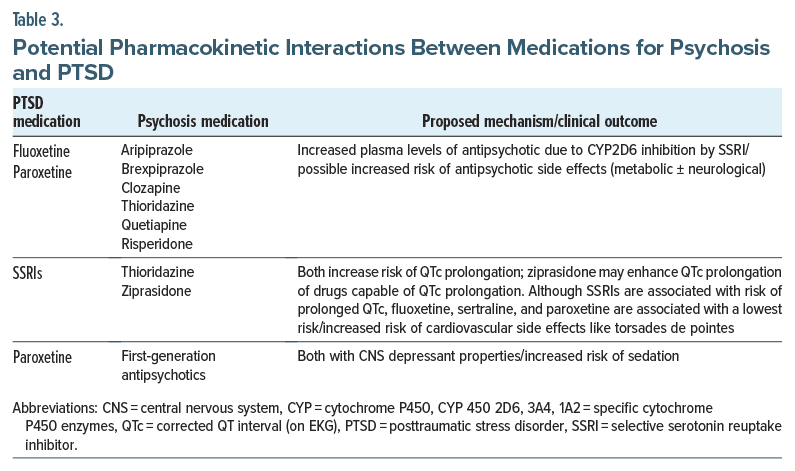
As for possible drug interactions with treatments that target psychosis, fluoxetine and paroxetine can increase the plasma levels of several antipsychotics through inhibition of cytochrome P450 2D6 (Table 2 and Table 3). In addition, the QTc-prolonging effects of SSRIs may be amplified by coadministration of antipsychotics, especially ziprasidone and thioridazine, although the SSRIs discussed here have a low likelihood of prolonging the QTc45 (Table 3). Further, when using an SSRI or SNRI for the treatment of PTSD, dosing should be appropriate (Table 1), and the trial should last at least 8–12 weeks before changing to an alternative agent or augmenting the treatment.43
When adding another agent, antipsychotics (Table 2) are commonly selected, despite having a bevy of untoward side effects (eg, metabolic and neurological) and adversely affecting physical health and quality of life, as the benefits (a reduced symptom burden) are worth the risks (eg, acute or chronic motor movement disorders, metabolic and endocrine abnormalities, autonomic changes, and an increased risk of seizures, myocardial infarction, and neuroleptic malignant syndrome).
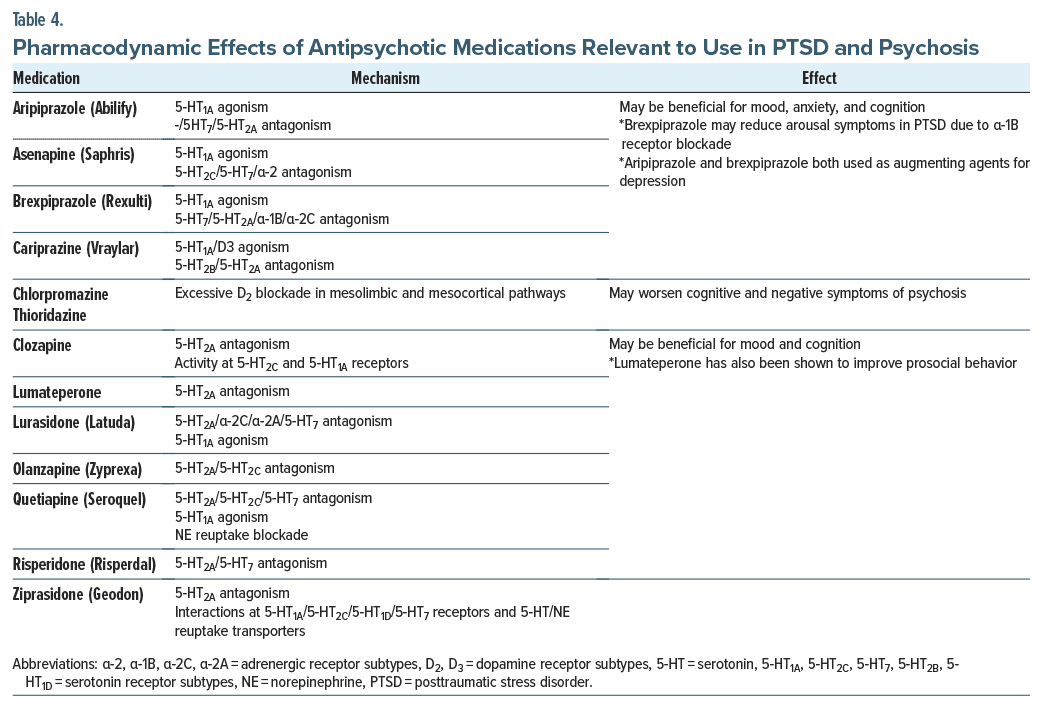
Although a variety of reasons have led to adjunctive use of antipsychotics in PTSD, the most common ones are related to PTSD-related poor sleep and intrusive thoughts, auditory hallucinations or delusions, and mood instability. All first-generation antipsychotics (FGAs) and second-generation antipsychotics (SGAs) can improve insomnia due to their sedating qualities, although SGAs (eg, quetiapine, olanzapine, and ziprasidone) are prescribed most often. None of the antipsychotics have received US Food and Drug Administration approval for the management of PTSD-associated nightmares, although clinicians frequently use risperidone or quetiapine to treat reexperiencing symptoms of PTSD. Similarly, their ability to induce sedation can be used to relieve daytime distress from intrusive thoughts or images. In addition, the newer third-generation antipsychotics are growing more popular for mood stabilization due to their unique partial-dopamine agonism, in comparison to the full dopamine blockade achieved by FGAs and SGAs.
When antipsychotics are used, they should be given once or twice a day and have smaller doses made available, as needed, for distress. Moreover, their side effect profile, drug interactions, and tolerability, as well as the patient’s preference, should be considered when selecting a medication. Examples of common drug interactions are provided in Tables 3 and 4.
What Is the Outcome of Patients With Comorbid PTSD and Psychosis?
A systematic review of outcomes of comorbid PTSD and schizophrenia found that these diagnoses were associated with worse outcomes, symptom severity, neurocognitive functioning, general psychopathology, suicidality, and quality of life than a diagnosis of schizophrenia alone47; however, several protective factors can result in less severe trauma symptoms and/or positive outcomes. A questionnaire of 85 patients with psychosis found that both resilience and adaptive coping were associated with 44% of the variance in posttraumatic growth.48 Therefore, clinicians often attempt to integrate intervention strategies to enhance protective factors that may lead to positive treatment outcomes.
WHAT HAPPENED TO MR A?
Following a prolonged hospitalization, Mr A was stabilized with an antipsychotic and was discharged to the care of his outpatient team. Over the next several months, he continued to have nightmares related to the content of his prior hallucinations, and he resisted going to the ED when he injured his ankle after discharge. His mood has been low; reminders of his hospital experience are linked with feeling hopeless and shamed. His outpatient team noted that he has been vulnerable to the development of PTSD, given his experiences as well as his history of childhood trauma.
CONCLUSION
The experience of psychosis (eg, delusions and hallucinations) varies significantly among individuals; fortunately, most perceptual experiences are viewed as non–life threatening. However, derealization, acute emotional distress, disorganized behaviors, and associated treatment and hospitalization each have the potential to be traumatic. Coercive interventions (eg, restraints and involuntary administration of medications) are often associated with reduced adherence to psychiatric treatment (secondary to avoidance of trauma-related stimuli),49 less time in treatment, and loss of confidence in mental health providers. Although clinicians may not pose a threat to their psychiatric patients, some patients perceive a threat to their well-being during their hospitalization that can lead to the development of PTSD.
The first step to successful management of psychosis related PTSD is ensuring a proper assessment. Some clinicians fear that trauma-focused questioning may exacerbate the risk, worsen distress, or increase psychotic symptoms. Although studies have shown that patients often anticipate these trauma-related questions, the lack of an opportunity to discuss trauma and its connections to psychosis may lead to perceived negative consequences on the patient’s part. Providers should be aware that exploration of traditionally recognized traumas and broad questions of “abuse” histories often do not allow for comprehensive responses that would reveal psychosis related trauma.
Early and sustained treatment of PTSD or psychosis related PTSD is pivotal in improving long-term outcomes. Delays in treatment are associated with exacerbations of both PTSD and psychotic symptoms, as well as worsened functioning and quality of life. Psychosocial interventions intended to treat PTSD with exposure therapy are most effective in reducing PTSD symptoms and can also reduce symptoms of psychosis. Comorbid PTSD and schizophrenia are associated with worse outcomes in symptom severity, neurocognitive functioning, general psychopathology, suicidality, and quality of life than a diagnosis of schizophrenia alone.
Article Information
Published Online: February 6, 2025. https://doi.org/10.4088/PCC.24f03831
© 2025 Physicians Postgraduate Press, Inc.
Submitted: August 14, 2024; accepted October 14, 2024.
To Cite: Rustad JK, Waaland W, Coughlin B, et al. Psychosis-related posttraumatic stress disorder: true, true, and unrelated? Prim Care Companion CNS Disord. 2025;27(1):24f03831.
Author Affiliations: Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire (Rustad, Sippel); White River Junction VA Medical Center, White River Junction, Vermont (Rustad, Fuller); Burlington Lakeside VA Community Based Outpatient Clinic, Burlington, Vermont (Rustad, Fuller); Mental Health Counseling Program, State University of New York, New Paltz (Waaland); Dartmouth-Hitchcock Medical Center Adult Psychiatry Residency Program, Lebanon, New Hampshire (Coughlin, Neu, Wilson, Schwartz); VA Northeast Program Evaluation Center, and an Affiliate at the National Center for PTSD, Lebanon, New Hampshire (Sippel); Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts (Stern).
Corresponding Author: James K. Rustad, MD, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Dartmouth-Hitchcock Medical Center, One Medical Center Dr, Lebanon, NH 03756 ([email protected]).
Relevant Financial Relationships: Drs Rustad and Sippel and Ms Fuller are employed by the US Department of Veterans Affairs, but the opinions expressed in this presentation do not reflect those of the Department of Veterans Affairs. Dr Stern has received royalties from Elsevier for editing textbooks on psychiatry. The other authors report no conflicts of interest related to the subject of this article.
Funding/Support: None.
Clinical Points
- Frightening psychotic experiences might serve as traumatic events and precipitate the development of posttraumatic stress disorder (PTSD).
- Clinicians should be aware that exploration of traditionally recognized traumas or broad questions of “abuse” histories often do not allow for comprehensive responses that would reveal psychosis-related trauma.
- Comorbid PTSD and schizophrenia are associated with worse outcomes in symptom severity, neurocognitive functioning, general psychopathology, suicidality, and quality of life than a diagnosis of schizophrenia alone.
- Some vulnerable populations may be more susceptible to the development of PTSD related to psychosis; one mediating factor may be racial disparities in psychiatric care.
References (49)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Text rev. American Psychiatric Association; 2022.
- Goldstein RB, Smith SM, Chou SP, et al. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National Epidemiologic Survey on alcohol and related conditions-III. Soc Psychiatry Psychiatr Epidemiol. 2016;51(8):1137–1148. PubMed CrossRef
- World Health Organization. Mental Disorders. World Health Organization; 2022. Accessed December 8, 2024. https://www.who.int/news-room/fact-sheets/detail/mental-disorders
- Paksarian D, Mojtabai R, Kotov R, et al. Perceived trauma during hospitalization and treatment participation among individuals with psychotic disorders. Psychiatric Serv. 2014;65(2):266–269. PubMed CrossRef
- Berry K, Ford S, Jellicoe-Jones L, et al. PTSD symptoms associated with the experiences of psychosis and hospitalisation: a review of the literature. Clin Psychol Rev. 2013;33(4):526–538. PubMed CrossRef
- Marx BP, Hall-Clark B, Friedman MJ, et al. The PTSD Criterion A debate: a brief history, current status, and recommendations for moving forward. J Trauma Stress. 2024;37(1):5–15.
- Abdelghaffar W, Ouali U, Jomli R, et al. Posttraumatic stress disorder in first episode psychosis: prevalence and related factors. Clin Schizophr Relat Psychoses. 2018;12(3):105–112B.
- Hogben GL, Cornfield RB. Treatment of traumatic war neurosis with phenelzine. Arch Gen Psychiatry. 1981;38(4):440–445. PubMed CrossRef
- Seedat S, Stein MB, Oosthuizen PP, et al. Linking posttraumatic stress disorder and psychosis: a look at epidemiology, phenomenology, and treatment. J Nerv Ment Dis. 2003;191(10):675–681. PubMed CrossRef
- Shevlin M, Armour C, Murphy J, et al. Evidence for a psychotic posttraumatic stress disorder subtype based on the National Comorbidity Survey. Soc Psychiatry Psychiatr Epidemiol. 2011;46(11):1069–1078. PubMed CrossRef
- Dallel S, Fakra E, Cancel A. Prevalence of posttraumatic stress disorder in schizophrenia spectrum disorders: a systematic review. Neuropsychiatry. 2018;8(3):1027–1037.
- OConghaile A, DeLisi LE. Distinguishing schizophrenia from posttraumatic stress disorder with psychosis. Curr Opin Psychiatry. 2015;28(3):249–255. PubMed CrossRef
- Buswell G, Haime Z, Lloyd-Evans B, et al. A systematic review of PTSD to the experience of psychosis: prevalence and associated factors. BMC Psychiatry. 2021;21(1):9.
- Smith CM, Turner NA, Thielman NM, et al. Association of Black race with physical and chemical restraint use among patients undergoing emergency psychiatric evaluation. Psychiatr Serv. 2022;73(7):730–736. PubMed
- Marchi M, Travascio A, Uberti D, et al. Post-traumatic stress disorder among LGBTQ PEOPLE: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. 2023;32:e44.
- Spoont M, McClendon J. Racial and ethnic disparities in PTSD. PTSD Res Q. 2020;31(4):1–12.
- Schwartz RC, Blankenship DM. Racial disparities in psychotic disorder diagnosis: a review of empirical literature. World J Psychiatry. 2014;4(4):133–140. PubMed CrossRef
- Gevonden MJ, Selten JP, Myin-Germeys I, et al. Sexual minority status and psychotic symptoms: findings from The Netherlands Mental Health Survey and Incidence Studies (NEMESIS). Psychol Med. 2014;44(2):421–433. PubMed CrossRef
- Tabb LP, Rich JA, Waite D, et al. Examining associations between adverse childhood experiences and posttraumatic stress disorder symptoms among young survivors of urban violence. J Urban Health. 2022;99(4):669–679.
- Grindey A, Bradshaw T. Do different adverse childhood experiences lead to specific symptoms of psychosis in adulthood? A systematic review of the current literature. Int J Ment Health Nurs. 2022;31(4):868–887.
- Bendall S, Alvarez-Jimenez M, Hulbert CA, et al. Childhood trauma increases the risk of post-traumatic stress disorder in response to first-episode psychosis. Aust N Z J Psychiatry. 2012;46(1):35–39. PubMed CrossRef
- McCabe SE, Hughes TL, West BT, et al. Sexual orientation, adverse childhood experiences, and comorbid DSM-5 substance use and mental health disorders. J Clin Psychiatry. 2020;81(6):20m13291. PubMed
- Zhang X, Monnat SM. Racial/ethnic differences in clusters of adverse childhood experiences and associations with adolescent mental health. SSM Popul Health. 2022;17:100997. PubMed
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults – the adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258. PubMed CrossRef
- Campodonico C, Varese F, Berry K. Trauma and psychosis: a qualitative study exploring the perspectives of people with psychosis on the influence of traumatic experiences on psychotic symptoms and quality of life. BMC Psychiatry. 2022;22(1):213.
- Airey ND, Taylor CDJ, Vikram A, et al. Trauma measures for use with psychosis populations: a systematic review of psychometric properties using COSMIN. Psychiatry Res. 2023;323:115163. PubMed
- Carr S, Hardy A, Fornells-Ambrojo M. The Trauma and Life Events (TALE) checklist: development of a tool for improving routine screening in people with psychosis. Eur J Psychotraumatol. 2018;9(1):1512265. PubMed CrossRef
- Rodrigues R, Anderson KK. The traumatic experience of first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2017;189:27–36. PubMed CrossRef
- Reid J, Cole C, Malik N, et al. The effectiveness and tolerability of trauma-focused psychotherapies for psychotic symptoms: a systematic review of trauma-focused psychotherapies. Int J Methods Psychiatr Res. 2024;33(1):e2005. PubMed
- Keen N, Hunter E, Peters E. Integrated trauma-focused cognitive behavioural therapy for post-traumatic stress and psychotic symptoms: a case-series study using imaginal reprocessing strategies. Front Psychiatry. 2017;8:92.
- Callcott P, Standart S, Turkington D. Trauma within psychosis: using a CBT model for PTSD in psychosis. Behav Cogn Psychother. 2004;32(2):239–244.
- Ward-Brown J, Keane D, Bhutani G, et al. TF-CBT and EMDR for young people with trauma and first episode psychosis (using a phasic treatment approach): two early intervention service case studies. Cogn Behav Therapist. 2018;11:e17. PubMed
- de Bont P, van den Berg D, van der Vleugel B, et al. Prolonged exposure and EMDR for PTSD v. a PTSD waiting-list condition: effects on symptoms of psychosis, depression and social functioning in patients with chronic psychotic disorders. Psychol Med. 2016;46(11):2411–2421. PubMed CrossRef
- Slotema C, van den Berg D, Driessen A, et al. Feasibility of EMDR for posttraumatic stress disorder in patients with personality disorders: a pilot study. Eur J Psychotraumatol. 2019;10(1):1614822. PubMed CrossRef
- van den Berg D, van der Gaag M. Treating trauma in psychosis with EMDR: a pilot study. J Behav Ther Exp Psychiatry. 2012;43(1):664–671. PubMed CrossRef
- Yasar A, Kiraz S, Usta D, et al. Eye movement desensitization and reprocessing (EMDR) therapy on a patient with schizophrenia and clinical effects: a case study. Turkish J Psychiatr. 2017;29(2):138–142.
- de Bont P, van Minnen A, de Jongh A. Treating PTSD in patients with psychosis: a within-group controlled feasibility study examining the efficacy and safety of evidence-based PE and EMDR protocols. Behav Ther. 2013;44(4):717–730. PubMed CrossRef
- Trappler B, Newville H. Trauma healing via cognitive behavior therapy in chronically hospitalized patients. Psychiatr Q. 2007;78(4):317–325. PubMed CrossRef
- Mueser KT, Gottlieb JD, Xie H, et al. Evaluation of cognitive restructuring for post traumatic stress disorder in people with severe mental illness. Br J Psychiatr. 2015;206(6):501–508. PubMed CrossRef
- Steel C, Hardy A, Smith B, et al. Cognitive–behaviour therapy for post-traumatic stress in schizophrenia. A randomized controlled trial. Psychol Med. 2017;47(1):43–51. PubMed CrossRef
- Schnurr P, Vielhauer M, Weathers F, et al. The Brief Trauma Questionnaire (BTQ) [Measurement Instrument]. National Center for PTSD; 1999. Accessed August 11, 2024. http://www.ptsd.va.gov.
- Weathers FW, Litz BT, Keane TM, et al. The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD; 2013. Accessed August 11, 2024. www.ptsd.va.gov
- VA/DoD Clinical Practice Guideline for Management of Posttraumatic Stress Disorder and Acute Stress Disorder. US Gov Pr Office; 2023. Accessed August 8, 2024. www.healthquality.va.gov/guidelines/MH/ptsd
- Martin A, Naunton M, Kosari S, et al. Treatment guidelines for PTSD: a systematic review. J Clin Med. 2021;10(18):4175.
- Stahl SM. Prescriber’s Guide: Stahl’s Essential Psychopharmacology. 8th ed. Cambridge University Press; 2024. CrossRef
- Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507–517. PubMed
- Seow LSE, Ong C, Mahesh MV, et al. A systematic review on comorbid post traumatic stress disorder in schizophrenia. Schizophr Res. 2016;176(2–3):441–451. PubMed CrossRef
- Campodonico C, Berry K, Haddock G, et al. Protective factors associated with post-traumatic outcomes in individuals with experiences of psychosis. Front Psychiatry. 2021;12:735870. PubMed
- Mueser KT, Rosenberg SD. Treating the trauma of first episode psychosis: a PTSD perspective. J Ment Health. 2003;12(2):103–108. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!