Electroconvulsive therapy (ECT) is the most effective treatment for severe and treatment-resistant major depression. Although ECT has a strong safety profile, there are still risks secondary to the general anesthesia and the body’s physiological response to undergoing a seizure.1,2
During ECT, the body produces a brief 10-to 15-second parasympathetic response followed by a longer 5-to 10-minute sympathetic response characterized by hypertension, tachycardia, and arrhythmias.1 It is theorized that these increases in blood pressure and heart rate could lead to increased risk of an intracranial hemorrhage, especially in patients at an already higher risk of spontaneous bleeding.1,3
Having an intracranial bleed related to ECT is rare. In a series of 20,000 ECT procedures, there was a single case of intracerebral hemorrhage (0.005% of cases).4 In another study, ECT was not associated with an elevated risk of incident or recurrent stroke, including patients with significant vascular risk factors.5
The American Psychiatric Association published a task force report in 2001 with recommendations regarding the treatment, training, and privileging of ECT.2 This publication contains only 1 sentence on the use of ECT in patients with thrombocytopenia, which states “No special precautions appear indicated in patients with thrombocytopenic states.”2(p41)
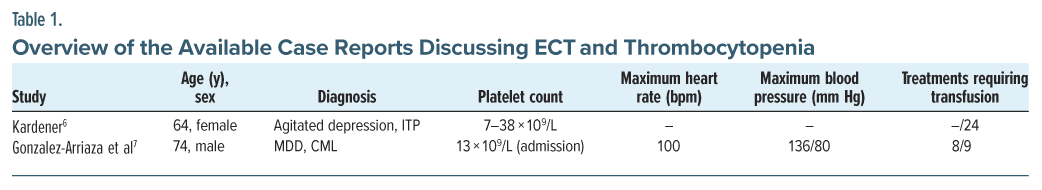
ECT has been in use for over 80 years in the United States, yet there are only 2 case reports (from 1968 to 2001) that describe use in patients with significant thrombocytopenia.2,6,7 Due to the limited number of randomized controlled trials and lack of published guidelines regarding use of ECT in patients with comorbidities, psychiatrists may face challenges weighing risks and benefits of ECT in patients with severe thrombocytopenia.8
Case Report
Ms A is a 36-year-old woman with history of major depressive disorder, panic disorder, and posttraumatic stress disorder who presented to the emergency department with worsening depression in the context of multiple psychosocial stressors. Her medical history was significant for paroxysmal nocturnal hemoglobinuria and a bone marrow transplant. A complete blood count revealed pancytopenia: hemoglobin of 4.56 g/dL (11.6–15 g/dL), absolute neutrophil count of 0.7×109/L (2.5–6.0 × 109/L), and platelet count of 31 × 109/L (150–400 × 109/L).
Ms A endorsed previous trials of multiple selective serotonin reuptake inhibitors (citalopram, fluoxetine, and sertraline), lamotrigine, methylphenidate, alprazolam, aripiprazole, doxepin, lorazepam, and mirtazapine with no significant benefit. She required numerous transfusions and a bone marrow biopsy before she was transferred to the inpatient psychiatric unit for further medication management of her depressive symptoms. Due to the severity of the patient’s presentation and her history of treatment resistance, ECT was initiated.
The anesthesia team recommended transfusing the patient to a platelet count of 50×109/L before proceeding with ECT. We researched platelet transfusion guidelines, looked at similar case studies, and had a multidisciplinary meeting with the bone marrow transplant team before establishing a preprocedural platelet goal of 20×109/L.
Ms A’s platelets ranged from 24 to 40× 109/L prior to all 6 ECT treatments. No platelet transfusions were required, and there were no complications. Toward the end of her ECT course, the patient’s depression had significantly improved.
We could only find 2 published case reports describing use of ECT in patients with significant thrombocytopenia (Table 1).6,7 Gonzalez-Arriaza et al7 decided on a preprocedural platelet goal of 20×109/L. Randomized trials of prophylactic platelet transfusion for procedures present logistic and ethical challenges, and these cutoffs were decided empirically.
Discussion
Patients with platelet counts >50×109/L usually do not experience abnormal bleeding even with surgery. Patients with counts between 20×109/L and 50 ×109/L may experience excessive bleeding with minor trauma, but spontaneous hemorrhage is unusual. When the platelet count is less than 20 ×109/L, spontaneous bleeding may occur, and the risk for severe bleeding is high if the platelet count is less than 10×109/L.9 The clinical practice guideline from the American Association of Blood Banks recommends prophylactic transfusions for the following:
- 10 ×109/L or less to reduce the risk for spontaneous bleeding
- 20 ×109/L for patients having elective central venous catheter placement
- 50×109/L prior to elective diagnostic lumbar puncture or major elective nonneuraxial surgery
However, clinical judgment, and not a specific platelet count threshold, is paramount in deciding whether to transfuse platelets.10 Platelet transfusion is not a benign treatment and carries multiple risks including febrile reactions, allergic reactions, and infections.11 Excessive platelet transfusions also incur a high cost and can worsen the critically low supply of blood and platelet products.12 If our patient had a preprocedural platelet goal of 50×109/L, as initially recommended by anesthesia, she would have required multiple transfusions throughout her course of ECT.
This case highlights that ECT can be used safely in patients with severe thrombocytopenia. Although rare, there is a need for more research into understanding the mechanism behind intracranial hemorrhage during ECT and potential ways to reduce complications. We recommend a platelet goal of 20×109/L prior to each ECT treatment; however, additional studies are needed to determine cutoff limits for platelet transfusions prior to ECT to avoid excessive platelet transfusions, while still protecting patients from spontaneous intracranial hemorrhages.
Article Information
Published Online: July 15, 2025. https://doi.org/10.4088/PCC.25cr03922
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(4):25cr03922
Submitted: January 17, 2025; accepted April 10, 2025.
To Cite: Nearine J, Ong-Martin S, Ramos R, et al. Safety of electroconvulsive therapy in severe thrombocytopenia. Prim Care Companion CNS Disord 2025;27(4):25cr03922.
Author Affiliations: Department of Psychiatry and Behavioral Medicine, Atrium Health Wake Forest Baptist, Winston Salem, North Carolina (all authors).
Corresponding Author: Sahil Munjal, MD, Department of Psychiatry and Behavioral Medicine, Atrium Health Wake Forest Baptist, 1 Medical Center Blvd, Winston Salem, NC 27157 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (12)

- Salik I, Marwaha R. Electroconvulsive therapy. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed March 20, 2025. http://www.ncbi.nlm.gov/books/NBK538266/.
- Task Force on Electroconvulsive Therapy; Weiner RD. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging: A Task Force Report of the American Psychiatric Association. 2nd ed. American Psychiatric Association; 2001.
- Shioda K, Saito N, Nisijima K, et al. Second case report of successful electroconvulsive therapy for a patient with schizophrenia and severe hemophilia A. Neuropsychiatr Dis Treat. 2014;865.
- Matthew JR, Constan E. Complications following ECT over a three-year period in a state institution. Am J Psychiatry. 1964;120:1119–1120. PubMed CrossRef
- Rozing MP, Jørgensen MB, Osler M. Electroconvulsive therapy and later stroke in patients with affective disorders. Br J Psychiatry. 2019;214(3):168–170. PubMed CrossRef
- Kardener SH. EST in a patient with idiopathic thrombocytopenic purpura. Dis Nerv Syst. 1968;29(7):465–466. PubMed
- Gonzalez-Arriaza HL, Mueller PS, Rummans TA. Successful electroconvulsive therapy in an elderly man with severe thrombocytopenia: case report and literature review. J ECT. 2001;17(3):198–200. PubMed CrossRef
- Rabheru K. The use of electroconvulsive therapy in special patient populations. Can J Psychiatry. 2001;46(8):710–719. PubMed CrossRef
- Shuman M. Hemorrhagic disorders: abnormalities of platelet and vascular function. In: Goldman L, Bennet JC, eds. Cecil Textbook of Medicine. 21st ed. WB Saunders, Co; 2000:996–1004.
- Kaufman RM, Djulbegovic B, Gernsheimer T, et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2015;162(3):205–213. PubMed CrossRef
- Kaufman RM, Assmann SF, Triulzi DJ, et al. Transfusion-related adverse events in the Platelet Dose study. Transfus Paris. 2015;55(1):144–153. PubMed CrossRef
- Red Cross Declares First-ever Blood Crisis amid Omicron Surge [Internet]. American Red Cross; 2022. Accessed March 20, 2025. https://www.redcross.org/about-us/news-and-events/press-release/2022/blood-donors-needed-now-as-omicron-intensifies.html.
Enjoy this premium PDF as part of your membership benefits!