Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(6):25f04018
Author affiliations are listed at the end of this article.
Have you ever encountered a veteran who was worried about developing cancer or another serious medical condition? Would you be surprised to learn that a bevy of medical conditions have been presumptively linked to toxic exposures while serving in the military? Have you been uncertain about what types of resources and benefits are available to veterans for the screening, diagnosis, and treatment of disorders related to such exposures? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Mr A, a 45-year-old veteran with 22 years of service in Naval Special Warfare as a SEAL, experienced multiple toxic exposures over the course of his career. He had 9 deployments in highly kinetic combat zones in Iraq, Afghanistan, and the Philippines. His service led him to face multiple exposures that contributed to his ongoing cognitive difficulties and physical symptoms. He reported exposure to burn pits, dust storms, airborne industrial pollutants, and poor air quality, in addition to multiple blast exposures, including proximity to improvised explosive devices (IEDs), mortars, and vehicle-born IEDs, and numerous instances of head trauma from hard parachute landings.
Mr A’s symptoms intensified after his 2016 deployment, with issues such as memory problems, concentration difficulties, balance and coordination issues, chronic musculoskeletal pain, and insomnia. Recently, he also developed a nagging cough, which, although intermittent, raised concerns about the potential for long-term respiratory issues. He worried about this being related to his exposure to toxic substances, including burn pits, mustard gas during training exercises, unsanitary water, and poor air quality during deployments.
Mr A lives with his wife of 18 years and 2 children,aged 8 and 10 years. He is employed full time in a civilian defense role that involves frequent travel. Although he has a supportive family, he has avoided seeking mental health care. His wife accompanied him to the Comprehensive Brain Health and Trauma Program, expressing concern about his recent changes in mood, increasing irritability, emotional detachment, and forgetfulness.
Cancer Risks and Family History
Although Mr A is a nonsmoker and maintains a healthy exercise regimen (exercising 5 times per week), he has significant occupational exposure to potential cancer-causing agents. These include burn pits, unclean water, and exposure to chemicals. His family medical history includes significant cancer risk factors: on his maternal side, his aunt had breast cancer, and on his paternal side, there was a history of prostate cancer in his father and grandfather. While Mr A’s most recent prostate-specific antigen test was unremarkable, his combined occupational exposures and family history led to concern about his health risks. He was interested in the Massachusetts General Hospital (MGH) Early Detection and Diagnostic Center cancer screening.
DISCUSSION
What Constitutes a Toxic Exposure?
The US Department of Veterans Affairs (VA) defines a toxic exposure as “an exposure to a substance, chemical, or airborne hazard identified in the list under Section 1119(b)(2)” of Title 38 of the U.S. Code1,2; however, more broadly, this refers to contact with harmful substances that can lead to short- and long-term negative health consequences. Exposures to toxic substances among those in the military account for an underrecognized cause of chronic morbidity. Epidemiologic data from VA registries have demonstrated links between deployment-related exposures (eg, airborne particulate matter from open burn pits, organophosphate nerve agents, depleted uranium, and industrial solvents) and an increased risk of developing diseases (eg, respiratory pathologies, malignancies, neurocognitive disorders, and psychiatric disorders, including depression and posttraumatic stress disorder [PTSD]).
The most common causes of toxic exposures in US military members occur from environmental and occupational hazards that are encountered during training, deployments, and base operations. Burn pits, which were used extensively in operations in Iraq and Afghanistan, generated complex mixtures of dioxins, volatile organic compounds, and particulate matter, with epidemiologic studies showing associations with respiratory diseases and an increased risk of cancer.3 During aircraft maintenance and the handling of combat arms (eg, munitions including repetitive artillery, howitzers, mortars), military members have also been repeatedly exposed to jet fuels, solvents, and heavy metals, including lead and mercury, which have negative hematologic and neurocognitive consequences.4 Exposures to Agent Orange during the Vietnam War and to contaminated drinking water at Camp Lejeune (1953–1987) have also been linked to a multitude of negative downstream effects, including cancer and neurologic and metabolic disorders.5 During the 1990–1991 Gulf War and Operation Iraqi Freedom/ Operation Enduring Freedom conflicts, military members were exposed to organophosphates (both as insecticides and as nerve agents) and oil-fire smoke, which contributed to chronic multisystem illnesses characterized by fatigue, headaches, joint pain, indigestion, insomnia, dizziness, respiratory disorders, and memory problems, which have been thought to be secondary to neuroinflammation and mitochondrial dysfunction.6,7
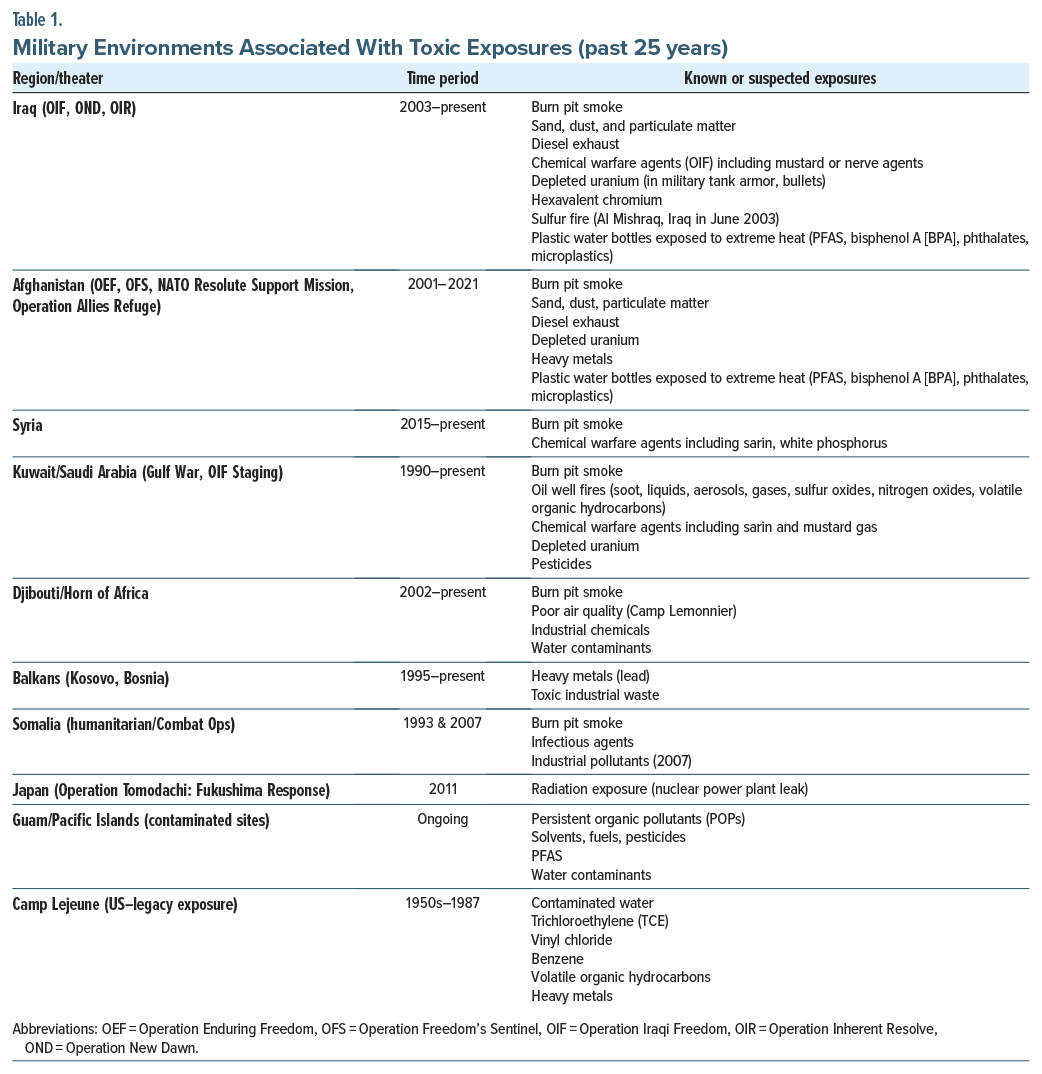
Which Military Environments in the Past 25 Years—Including Combat Zones and Domestic or Overseas Installations—Have Been Associated With Exposure to Toxic Substances?
Over the past 25 years, US service members have been exposed to a wide range of toxic substances during combat operations, peace-keeping missions, humanitarian deployments, and even at stateside bases such as Camp Lejeune (Table 1). Across regions like Iraq, Afghanistan, Syria, and the Horn of Africa, troops encountered complex toxic environments (eg, burn pit smoke, chemical warfare agents, airborne, particulate matter, heavy metals, diesel exhaust, and industrial pollutants).8–10 These cumulative exposures—often layered in austere environments lacking protective infrastructure—continue to shape long-term health outcomes for veterans and warrant proactive screening, clinical attention, and policy response.
Who Has Been at Highest Risk for Exposure to Toxic Substances?
Military service members are often at an increased risk of toxic substance exposure due to their specific roles, duties, and deployment locations. These exposures can create serious long-term health consequences. The VA recognizes the consequences of toxic exposures and offers resources and compensation for veterans who have been adversely affected.11 Several groups (eg, those exposed to burn pits, nuclear waste, nuclear radiation, chemical agents, firefighting foam, explosive ordnance, aviation facilities, construction materials) have been at greatest risk from exposure to toxins.
Burn Pit Exposure: Personnel Deployed to Iraq, Afghanistan, and the Gulf
Roughly 3.5 million service members stationed at bases in Iraq, Afghanistan, and other parts of Southwest Asia were frequently exposed to open-air burn pits that were used to dispose of waste materials (eg, plastics, electronics, and medical waste).12,13 Inhalation of the resulting toxic smoke has been linked to respiratory diseases, cancers, and other chronic conditions.
Nuclear Radiation: Atomic Veterans and Nuclear Workers
Personnel involved in nuclear weapons testing or cleanup operations or who were stationed at nuclear facilities were exposed to ionizing radiation. This group includes those present during atmospheric tests in the Pacific and Nevada, as well as workers at sites like Los Alamos and Oak Ridge. Radiation exposure has been linked to various cancers (eg, leukemia and multiple myeloma). Veterans who served in the post-WWII occupation of Hiroshima or Nagasaki or who were imprisoned in Japan, worked with or near nuclear weapons testing, or served at a gaseous diffusion plant or in other capacities may be at risk of illnesses believed to be caused by radiation.14–17 Radiation exposure has been associated with acute radiation syndrome, fatigue, renal disease, headaches, and numerous cancers. The VA designates multiple malignancies (eg, brain, bone, breast, lung, and leukemia) as presumptive conditions for veterans involved in radiation-risk activities during service.16
Chemical Agents: World War II, Vietnam, Gulf War Veterans, Project 112/Project Shipboard Hazard and Defense (SHAD), and Camp LeJeune
Veterans who served in Vietnam or near the Korean Demilitarized Zone during the Vietnam era may have been exposed to Agent Orange, a herbicide linked to cancers, diabetes, and birth defects.5,18 In addition, Gulf War veterans faced exposure to chemical warfare agents and other hazardous substances.19 Veterans who served at the German bombing of Bari, Italy in World War II or worked in certain other jobs may have come in contact with mustard gas.20 Veterans who were part of warfare testing for Project 112 or Project Shipboard Hazard and Defense (SHAD) from 1962 to 1974 may be at risk of illnesses believed to be caused by chemical testing.21,22 However, a 2007 Institute of Medicine report found no clear evidence of specific long-term health problems associated with SHAD participation.21 While some differences were noted (eg, slightly higher risk of death due to cardiac disease), these findings lacked a clear biological basis and were not statistically significant when compared to nonparticipant veterans.22 Veterans at Camp Lejeune or MCAS New River (between August 1953 and December 1987) may be at risk for certain illnesses believed to be caused by contaminants found in the drinking water during that time.23,24 The VA recognizes several presumptive conditions linked to this exposure including hematologic disorders (eg, leukemia, aplastic anemia, myelodysplastic syndromes), numerous cancers (eg, bladder, kidney, liver, non-Hodgkin’s lymphoma, multiple myeloma), and Parkinson disease.24
Firefighting Foam (AFFF): Firefighters and Aircraft Handlers
Military personnel involved in firefighting or aircraft maintenance may have been exposed to aqueous film-forming foam (AFFF), which contains per- and polyfluoroalkyl substances (PFAS). PFAS are a component of firefighting foams used at airports and military installations to extinguish petroleum-based fires.25 PFAS are persistent environmental pollutants associated with myriad health risks, including cancers and hormonal disruptions.
Explosive Ordnance Disposal Technicians
Explosive ordnance disposal personnel who handle explosives and munitions are at risk of exposure to toxic substances such as nitrobenzene. Studies have indicated that bomb disposal veterans under the age of 70 years are 5 times more likely to develop bladder cancer compared to those in the general population.26
Aviation Crews: Helicopter Pilots and Aircrew
Aircrew members, particularly those who operate helicopters, like the Sea King and Chinook, have reported exposure to toxic exhaust fumes. Such exposures have been linked to increased incidences of cancers, including lung and blood cancers. Zach Stubbings, a former RAF flight sergeant and Prince William’s flying instructor, died of cancer following years of toxic exhaust fume exposure from Sea King helicopters,27 and Kai Macnaughton, a squadron leader, died from angiosarcoma, a rare blood cancer, after flying extensively in Puma and Chinook helicopters.28
Construction and Maintenance Personnel: Asbestos and Lead Exposure
Service members who have been involved in construction projects, shipbuilding, or maintenance may have encountered asbestos and lead-based materials. Exposure to these substances is associated with respiratory diseases and neurological disorders. Prolonged exposure to asbestos can cause lung scarring, non-malignant conditions involving thickening of the lung’s lining (which can impair lung function), and malignant mesothelioma. Lead-based materials were used commonly in paints and piping in military settings. Exposure to lead can result in significant neurological and cognitive impairments.
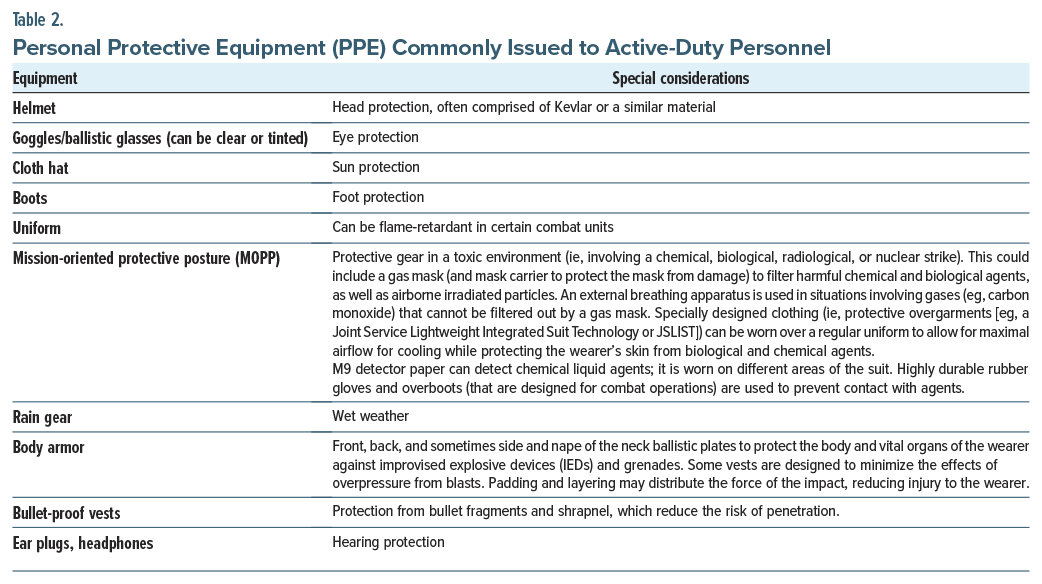
What Types of Personal Protective Equipment (PPE) Have Been Made Available to Active-Duty Personnel in Hazard-Prone Areas?
The nature of the personal protective equipment that is made available to active-duty personnel depends on their mission, commander, and occupation. To a large extent, the level of risk associated with an assignment or situation dictates the gear that is needed. Higher mission-oriented protective posture (MOPP), pronounced “mop,” levels correspond to an increasing level of protection; the readiness level is usually dictated by the in-theater commander.29 Unfortunately, MOPP cannot protect against exposure to high-energy, highly penetrating ionizing radiation (ie, neutrons and gamma radiation pass through all forms of PPE).30 Table 2 provides a list of PPE that are commonly issued to active-duty personnel.
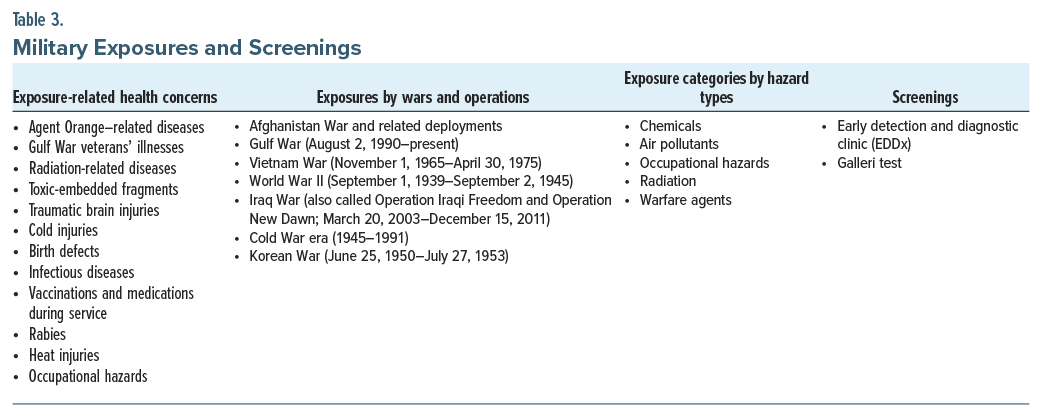
What Does Screening Related to Toxic Exposures for Active-Duty Personnel and Veterans Involve?
Health care providers in the military and in the public sector play vital roles in the screening of active-duty military and veterans related to toxic exposures. However, triaging a young person in the military with upper respiratory symptoms follows a different path than triaging a matched individual in the general population. This is because military personnel are exposed to a range of toxins rarely seen in the general population. Therefore, clinicians should ask their patients, “Are you a veteran or are you currently in the military?” The answer to this screening question will help to steer patients to the proper resources.31
According to the VA, the Sergeant First Class (SFC) Heath Robinson Honoring our Promise to Address Comprehensive Toxics (PACT) Act of 2022 was the largest health care benefit expansion in VA history.32 It ensured that active-duty personnel and veterans would be screened for toxic exposures. The PACT Act involves a 5- to 10-minute screening to identify potential exposures to toxins during one’s military service; it is repeated every 5 years.
Every veteran is eligible to enroll in the PACT Act without applying for disability benefits (if they meet the basic service and discharge requirements and any of the following descriptions are true: served in the Vietnam War or the Gulf War; served in combat zones in Iraq, Afghanistan, or elsewhere after 9/11; were deployed in support of the Global War on Terror; or were exposed to toxins or other hazards during military service at home or abroad).32 The VA reported that toxins and hazards include burn pits, sand and dust, particulate matter, oil well or sulfur fires, chemicals, radiation, warfare agents, depleted uranium, herbicides, and other occupational hazards.
When screening military personnel, it is helpful to think about toxic exposures in 3 ways. Table 3 displays these toxic exposures as belonging to 1 of 3 categories: exposures related to health concerns, exposures by wars and operations, and exposure categories by hazard types.33 Table 3 also presents screening tools that may be used for each exposure. In each of these exposure categories, a variety of infections, diseases, symptoms, defects, and injuries can occur in military personnel.
When reviewing the list of exposures encountered by active-duty service members and veterans, one finds that cancers are common sequelae. In fact, the VA estimates that more than 50,000 cases of cancer are diagnosed every year within VA health systems.34 One response to this cancer finding was John Hancock (a unit of Toronto-based Manulife) announcing (on November 13, 2024) that it was providing free access to Galleri, GRAIL’s multicancer early detection (MCED) test, to special operations veterans who were receiving care through Home Base in collaboration with MGH’s Cancer Early Detection and Diagnostic Clinic (EDDx) as part of the insurer’s mission to help people live longer, healthier, better lives.35 GRAIL Galleri is based on a prospective, case-controlled observational study that proved that the MCED demonstrated high specificity and accuracy of cancer signal origin prediction, and it detected cancer signals across a wide variety of cancers.36 This study concluded that the results supported the feasibility of the blood-based MCED test as a complement to existing single-cancer screening tests.36
In addition to the GRAIL’s MCED test, the EDDx at MGH is a clinic designed to bridge the gap between clinical care and research in early cancer detection.37 After reviewing the patient’s medical history, military career and toxin exposures, and family history of cancer, the health care provider might recommend further testing (eg, mammogram, computed tomography [CT] scan, positron-emission tomography-CT scan, colonoscopy, endoscopy, gynecologic exam with a Papanicolaou smear to detect cervical cancer, biopsy as well as other emerging technologies for early detection).37 The combination of the preventative cancer services offered at the MGH EDDx clinic and the GRAIL MCED test highlights just 2 of the many screening options that should be offered to those with military experience.
How Often Do Military Personnel and Veterans Worry About and Fear Developing Cancer Before or After Deployment to a Field of Operations Known to Have Environmental Toxins?
The term previvor, coined by Facing Our Risk of Cancer Empowered [FORCE] and later defined by the National Cancer Institute, refers to individuals at elevated risk for cancer who have not been diagnosed but live with the psychological burden of that risk due to genetic, environmental, or occupational exposures.38 This concept was underscored during the American Psychiatric Association’s 2025 Annual Meeting, when Pulitzer Prize–winning author Dr Siddhartha Mukherjee delivered the William C. Menninger Memorial Lecture at the 69th Convocation of Distinguished Fellows. Drawing on his clinical and scientific expertise, Mukherjee posed a resonant question: “Are we all previvors?”—highlighting how the anticipation of illness itself can shape mental health, identity, and medical engagement in the modern era.39
Concerns regarding the long-term health sequelae of toxic exposures sustained during military service are persistent and extensively documented. According to Dr Shereef Elnahal (Under Secretary for Health at the VA), toxic exposure risks are “connected to all generations” of warfighters.40 He emphasized that this reality “confirms what advocates have been saying for years, that the denominator of veterans exposed to harmful substances is quite large.”40
The personal experience of former President Joe Biden further illustrates the deeply human impact of these concerns. Following the death of his son, Major Beau Biden, from brain cancer on May 20, 2015, the possibility that toxic exposures encountered during military service contributed to his illness became a powerful motivating force behind the passage of the PACT Act.32,41 It established more than 23 conditions including respiratory illnesses (eg, asthma, chronic bronchitis, chronic obstructive pulmonary disease, pulmonary fibrosis, and interstitial lung disease), as well as several forms of cancer (including cancer of the brain, kidney, and gastrointestinal tract).42
Veteran engagement with PACT Act–related programs underscores the pervasive concern regarding toxic exposures within the military community. Since the launch of the VA’s PACT Act dashboard on January 1, 2023, a total of 2,220,685 claims have been processed, with an approval rate of 74.2%.43 Between August 10, 2022, and April 12, 2025, more than 6.1 million veterans completed the screening. Among them, 46.3% reported at least 1 potentially toxic exposure, and 9.8% reported multiple exposures.43 These data illuminate the scale of concern across the veteran population and strongly suggest that the health impacts of environmental exposures are both significant and widely experienced.
However, these challenges are further exacerbated by the limited reach of the existing health care system. Although clinical professionals within the VA report that a substantial number of veterans continue to express concerns about illnesses potentially associated with environmental exposures,40 nearly half of all US veterans are not enrolled in VA managed health care.44 This significant gap poses a critical barrier to comprehensive surveillance, diagnosis, and treatment efforts, thereby impeding progress in addressing the health and policy burdens experienced by many veterans.
Toxic exposures among military members are also thought to cause adverse psychological outcomes, both directly (through toxic mechanisms) and indirectly (through chronic illness). Depression, anxiety, PTSD, and neurocognitive disorders have been linked to many of the exposures found in military members, including heavy metals, solvents, and organophosphates.45,46 Veterans of the Gulf War were exposed to multiple overlapping toxic exposures, including burn pits, industrial pollutants, dust storms, poor air quality, chemical agents, and fuels. These exposures are associated with significantly higher rates of mood disorders and cognitive complaints compared to their nonexposed peers, and they have neuroimaging findings suggestive of changes in white matter integrity and altered brain metabolism.47 Military members who were exposed to burn pits report poor sleep, irritability, and chronic fatigue, which can complicate PTSD and depression, particularly in individuals who have sustained a traumatic brain injury.8 Finally, delayed diagnosis, failure to make the diagnosis, and ineffective treatment for diseases related to toxic exposures are sources of suffering and moral injury for service members who often feel isolated, especially in veterans with multiple symptoms of unclear etiology (eg, related to multisystem illness). The fact that the impact of toxic exposures can be compounded by effects on mental health emphasizes the need for treatment of afflicted military members, while addressing biological, psychological, and social factors.
How Do Active-Duty Personnel and Veterans Cope With the Knowledge That Their Friends and Fellow Soldiers Have Developed Cancer Possibly Related to Toxic Exposures?
The emotional toll of witnessing fellow service members develop cancer or other serious illnesses, potentially linked to toxic exposures during military service, is a profound and often under-recognized source of distress for both active-duty personnel and veterans.48 Coping with this reality requires a multifaceted response that includes personal resilience, communal support, and, frequently, frustration with systemic delays in recognition and care.
A “mission mindset,” cultivated through military training, frequently functions as a psychological buffer against adversity. This mindset fosters persistence, goal-directed behavior, and emotional fortitude in the face of personal or witnessed suffering. As one Marine veteran reflected, “Quitting as a Marine was never an option. Giving up on cancer is never an option for me.”49 Central to this mindset is a present-centered orientation, wherein veterans focus on what can be controlled and accomplished in the moment, a perspective that promotes sustained engagement and adaptive coping. Embracing hardship, colloquially expressed in military culture as “embracing the suck,” often empowers service members and veterans to actively participate in their treatment and retain a sense of agency. Furthermore, the inherently team-oriented nature of military service enables peers to mobilize in support of those who are ill, reinforcing a collective sense of purpose and bolstering emotional resilience for both the individual and their broader community.
Peer networks represent a critical source of psychological support for both veterans and active-duty personnel.50 These individuals frequently turn to one another for validation, shared understanding, and emotional connection, interactions that often occur through informal relationships as well as structured veteran service organizations. For a service-oriented community, the process of transforming grief into purposeful action serves as a meaningful coping strategy. Whether through advocating for legislative reforms (eg, the PACT Act), mentoring fellow veterans, or raising public awareness about the consequences of toxic exposures, such engagement fosters a sense of agency, purpose, and communal healing.51
However, the journey toward institutional acknowledgment is frequently long and fraught with delays. A 2024 report by the Military Officers Association of America and Disabled American Veterans found that veterans wait an average of 31.4 years from the time of their initial toxic exposure until the US government formally recognizes the connection to service-related disabilities. This delay compounds psychological stress and perpetuates a sense of injustice. As Army Staff Sgt. Mark Jackson expressed, “living with symptoms is difficult, but living without validation and causation of your symptoms is maddening.”52
These experiences often contribute to moral injury, survivor’s guilt, and enduring psychological distress.53 Without timely recognition, some individuals withdraw, suppress emotions, or develop worsening mental health symptoms. Others turn to maladaptive coping strategies, including substance use. These responses underscore the need for mental health services that are attuned to the specific burdens associated with military toxic exposures. While camaraderie and collective identity offer critical emotional scaffolding, systemic reform is essential to address the underlying institutional shortcomings. According to the VA, more than 43,000 veterans are diagnosed with cancer each year, with 16% of these cases involving rare forms of the disease. Currently, 400,000 veterans are receiving cancer care at VA facilities nationwide.54 These figures highlight the urgent need for timely validation, institutional accountability, and comprehensive medical and mental health support to ensure that no veteran or service member bears this burden alone.
Why Does Exposure to Toxins Lead to Cancer and Other Medical Conditions?
Many toxins are carcinogens—substances that can cause mutations in the deoxyribonucleic acid (DNA) of cells. DNA mutations can disable critical genes that control cell growth and division, such as tumor suppressor genes or oncogenes.55 Once DNA is damaged (such as double-strand breaks) and repair mechanisms fail to fulfill their mission, cells can begin to divide uncontrollably, leading to cancer. For instance, benzene exposure damages bone marrow DNA and increases the risk of leukemia, and asbestos fibers can injure the DNA of lung cells and lead to mesothelioma.56,57 Exposure to radiation has similar effects in terms of DNA damage and repair, leading to cancer.58
Other toxins cause long-term tissue inflammation. Chronic inflammation creates an environment that is rich in reactive oxygen species and cytokines, which can damage DNA, promote cell proliferation, and suppress normal immune surveillance.59 For instance, burn pit smoke exposure can cause persistent lung inflammation, increasing the risk for lung cancer and chronic lung diseases.
Certain toxins weaken or confuse the immune system. A compromised immune system may fail to detect and destroy cells that have started to mutate and grow abnormally. For example, dioxins (known as Agent Orange) can impair immune surveillance, allowing abnormal cells to survive and form tumors.60,61
Toxins can mimic or interfere with hormonal systems as endocrine disruptors, leading to disorders like infertility, thyroid diseases, or hormonally driven cancers such as breast or prostate cancer.62–64 For example, polychlorinated biphenyls (PCBs) and certain pesticides can increase the risk of breast cancer.64
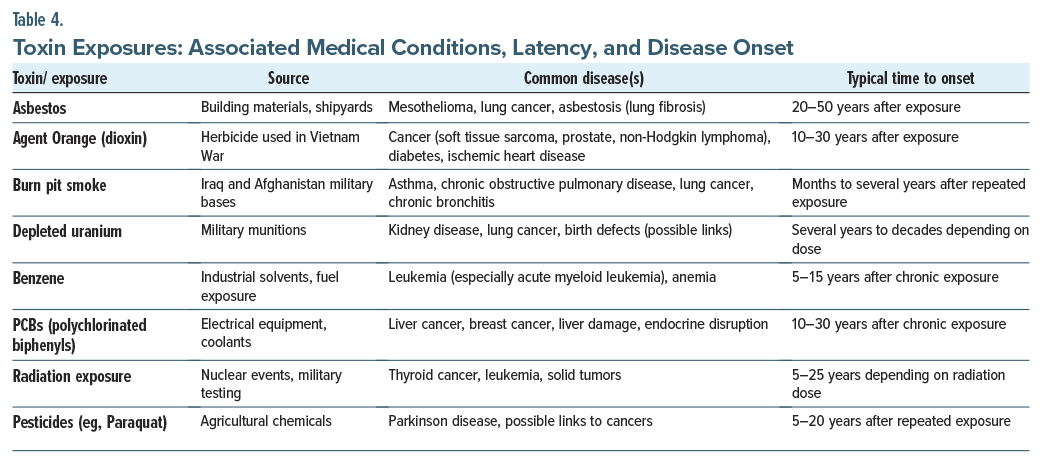
Some toxins are harmless until they are metabolized by the body into more dangerous forms that attack tissues directly. For example, aflatoxins found in moldy foods are metabolized in the liver into compounds that bind to DNA, causing liver cancer.65 In summary, toxins disrupt the normal balance and repair processes of the body. Over time, these disruptions can lead to cancer, chronic diseases, and organ failure (Table 4).
How Soon After Being Exposed to a Toxin Might an Illness or Condition Be Detected?
Some illnesses, like asthma from burn pit smoke, can appear within months of a toxic exposure. Most cancers that are linked to toxins take years (to decades) to develop because they require accumulated genetic damage.59 Dose and duration matter because high doses might cause a more rapid onset, whereas low, chronic exposures often result in later-onset disease.66 Age at exposure matters because exposures at a younger age may lead to earlier or more aggressive diseases (see Table 4).67,68
Which Interventions Can Mitigate the Psychological Sequelae of Toxin Exposure?
Military members who have been exposed to toxic substances have multiple physical and psychological consequences, which increase the disease burden (eg, cognitive impairment, anxiety, depression, and PTSD) and complicate treatment efforts.69 To mitigate these complications, pre-and postexposure interventions should address the needs of the military member dealing with the sequelae of toxic exposures as well as policy-level interventions.
For the service member, integrated physical and mental health care improves outcomes. By providing integrated care, where psychological care is seamlessly integrated with medical care, much of the stigma surrounding mental health care will be diminished.70
Interventions often involve cognitive-behavioral therapy (which is efficacious for addressing depression and PTSD), use of post–environmental exposure psychopharmacologic therapy (eg, selective serotonin reuptake inhibitors), psychoeducation and resilience training (which can reduce catastrophizing and enhance coping strategies), and peer support (that can reduce isolation).71
In addition, systematic screening for psychological symptoms in individuals with possible toxin exposures is critical. Early detection programs, such as the Department of Veterans Affairs’ Airborne Hazards and Open Burn Pit Registry, facilitate identification of at-risk individuals and enable timely referral to mental health services. On a larger level, ensuring that military policies support the documentation of possible exposures, provide medical surveillance for possible illness, and facilitate presumptive service connection for mental health conditions related to toxic exposures can further reduce stigma and decrease barriers to care.
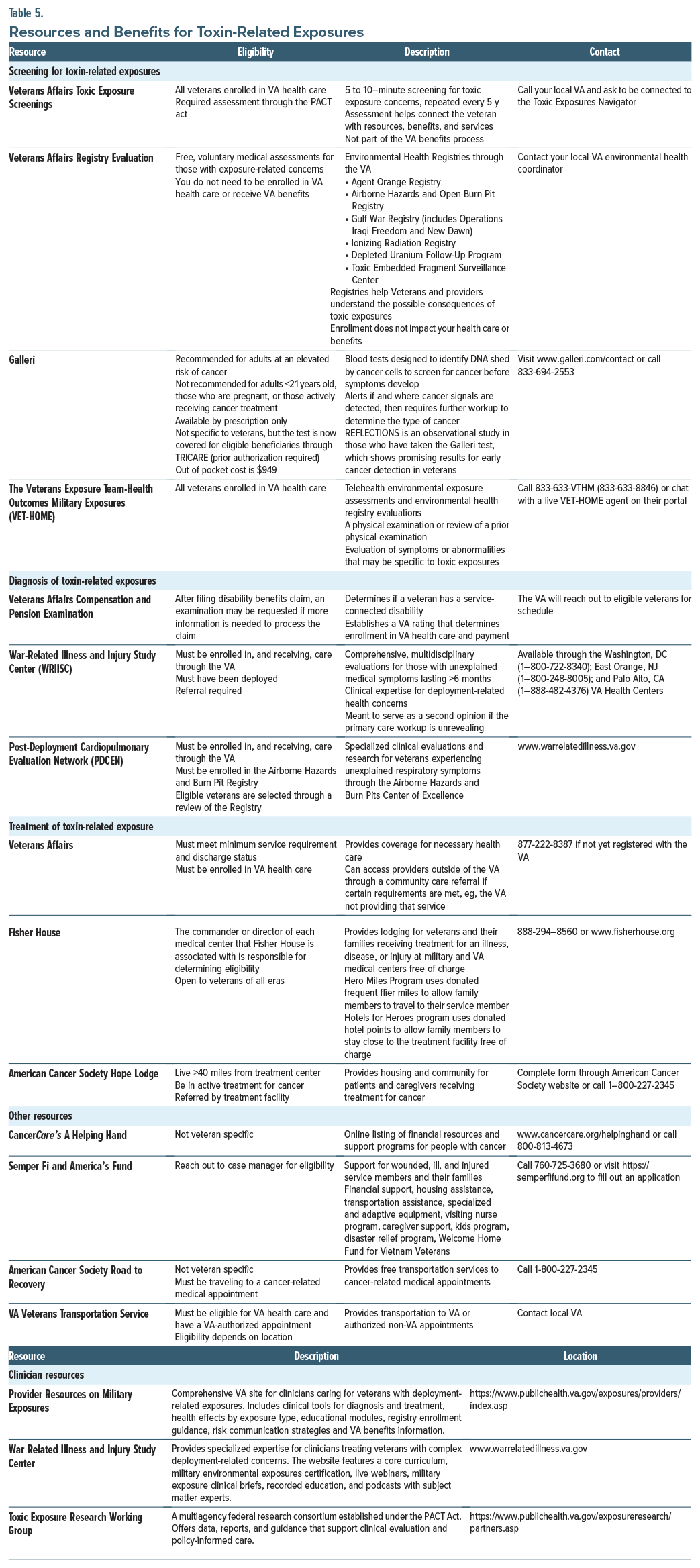
What Types of Resources and Benefits Are Available to Veterans for the Screening, Diagnosis, and Treatment of Disorders Related to Toxic Exposures?
As detailed previously, the PACT Act expanded VA access and benefits for veterans with toxic exposures. A variety of resources for veterans and clinicians are available for the screening, diagnosis, and treatment of disorders related to toxic exposures (Table 5).32,34,72–78
Veterans may be eligible for benefits and compensation for military-associated toxic exposure sequelae (eg, service-connected conditions or injuries that were caused or worsened by active military service). Veterans may apply for disability compensation by filing a claim through the VA.32 Surviving family members of veterans who died from a service-connected disability may also qualify for benefits (eg, monthly VA Dependency and Indemnity Compensation payments, accrued benefits payment, or survivor pensions).32
Can an Active-Duty Service Member or Veteran Claim Be Filed Before Disability Has Been Declared?
VA disability compensation requires that a diagnosed medical condition be linked to military service. An active-duty service member or veteran generally cannot file a VA disability claim based solely on exposure (eg, burn pits, radiation, or other toxic agents) without documented evidence of a resulting illness or injury.32 The VA requires 3 elements to approve a claim: a current diagnosed condition; evidence of an in-service event or exposure; and a medical connection between the 2. While service members may report and document toxic exposures during active duty (via registries such as the Airborne Hazards and Open Burn Pit Registry), a claim for compensation must wait until a diagnosable, service-connected disability develops. However, early documentation of exposures is encouraged, as it can strengthen future claims if symptoms arise.
Where Can Veterans and Their Health Care Providers Learn More About the Aftermath of Toxic Exposures and Their Options for Restitution?
To learn more about the aftermath of toxic exposures, veterans can request a Military Environmental Exposure clinical appointment with their primary care provider at the VA, or directly call their local VA Environmental Health Coordinator using the following directory: https://www.publichealth.va.gov/exposures/coordinators.asp.79 For restitution/service connection, veterans can file a claim through the Veteran’s Benefits Association (https://benefits.va.gov/benefits/).80
What Happened to Mr A?
Mr A was seen at the MGH Early Detection and Diagnosis Center for cancer screening due to concerns about his occupational exposures during military service. During the assessment, he reported exposures to burn pits, chemicals from industrial solvents, PFAS (firefighting foam), radar/radiation from large antennas, and mustard gas during training exercises. These exposures, along with a family history of cancer, including prostate cancer in his father and grandfather and breast cancer in his maternal aunt, raised his concern about long-term health risks.
We discussed the potential increased risk for developing cancers (such as genitourinary, dermatologic, gastrointestinal, and hematologic cancers) and the option of genetic testing to better assess cancer risk, considering his family history. Although family history increases the likelihood of carrying germline mutations, it is not definitive. Testing affected family members, particularly his father, mother, or maternal aunt, would provide clearer insight. Mr A was made aware of the psychological and financial implications of genetic testing, including the possible anxiety it could cause and the impact on insurance. Given his current health concerns, he consented to undergo both genetic testing, including BRCA1/2, and the Galleri MCED test. Mr A was found to harbor a BRCA2 germline mutation, with significant health implications for himself and his family. At this time, the Galleri MCED test results were still pending.
Fortunately, all treatment at Home Base is provided at no cost; it is supported by a Grateful Nation through philanthropic donations, private foundations, and federal partnerships rather than being paid through a single funding stream.
CONCLUSION
Exposure to substances (eg, depleted uranium), chemicals (eg, organophosphate nerve agents, industrial solvents), or airborne hazards (eg, airborne particulate matter from open burn pits) can lead to short- and long-term negative health consequences; however, those in the military account for an underrecognized cause of chronic morbidity and an increased risk of developing diseases (eg, respiratory pathologies, malignancies, neurocognitive disorders, and psychiatric disorders, including depression and PTSD). In addition, during aircraft maintenance and the handling of combat arms (eg, munitions including repetitive artillery, howitzers, mortars), military members have also been repeatedly exposed to jet fuels, AFFF (which are used to extinguish petroleum-based fires), and heavy metals (eg, lead, mercury), which have negative hematologic and neurocognitive consequences.
Every veteran is eligible to enroll in the PACT Act without applying for disability benefits (if they meet the basic service and discharge requirements and any of the following are true: served in the Vietnam War or the Gulf War; served in combat zones in Iraq, Afghanistan, or elsewhere after 9/11; were deployed in support of the Global War on Terror; or were exposed to toxins or other hazards during military service at home or abroad). Pre-and postexposure interventions, as well as policy-level interventions, should address the needs of military members dealing with the sequelae of toxic exposures.
The emotional toll of witnessing fellow service members develop cancer or other serious illnesses, potentially linked to toxic exposures during military service, is a profound and often under-recognized source of distress for both active-duty personnel and veterans. Without timely recognition, some individuals withdraw, suppress emotions, or develop worsening mental health symptoms.
Article Information
Published Online: November 25, 2025. https://doi.org/10.4088/PCC.25f04018
© 2025 Physicians Postgraduate Press, Inc.
Submitted: June 5, 2025; accepted August 5, 2025.
To Cite: Matta SE, Bonvie JL, Rustad JK, et al. Screening for and managing the sequelae of toxic exposures in veterans. Prim Care Companion CNS Disord 2025;27(6):25f04018.
Author Affiliations: Department of Psychiatry, Harvard Medical School, Boston, Massachusetts (Matta, Stern); Massachusetts General Hospital, Boston, Massachusetts (Matta, Bonvie, Joy, Rainone, Stern); Department of Psychology, Harvard Medical School, Boston, Massachusetts (Bonvie); Geisel School of Medicine at Dartmouth, Hanover, New Hampshire (Rustad); Larner College of Medicine at University of Vermont, Burlington, Vermont (Rustad); Burlington Lakeside VA Community Based Outpatient Clinic, Burlington, Vermont (Rustad); White River Junction VA Medical Center, Hartford, Vermont (Rustad); Home Base National Center of Excellence, Charlestown, Massachusetts (Joy, Rainone); Uniformed Services University of the Health Sciences, Bethesda, Maryland (La Croix); Long Beach VA Medical Center, Long Beach, California (Quang); Chao Family Comprehensive Cancer Center at University of California Irvine School of Medicine, Orange, California (Quang); 52nd President of the American College of Legal Medicine, Chicago, Illinois (Quang). Matta, Bonvie, Rustad Joy, Rainone, La Croix, and Quang are co-first authors; Stern is senior author.
Corresponding Author: Theodore A. Stern, MD, Massachusetts General Hospital, 55 Fruit St, WRN 606, Boston, MA 02114 ([email protected]).
Relevant Financial Relationships: Dr Rustad is employed by the United States Department of Veterans Affairs, but the opinions expressed in this article do not reflect those of the Department of Veterans Affairs. Dr La Croix is an active-duty Naval officer and is employed by the United States Department of Defense, but the opinions expressed in this article are her own and do not reflect those of the Uniformed Services University, the United States Navy, or the Department of Defense. Dr Quang is employed by the United States Department of Veterans Affairs, but the opinions expressed in this article are his own and do not reflect those of the Department of Veterans Affairs. Dr Stern has received royalties from Elsevier for editing textbooks on psychiatry. Drs Matta and Bonvie and Mss Joy and Rainone report no relevant financial relationships.
Funding/Support: None.
Acknowledgement: Dr Rustad would like to express his gratitude to Joshua Gerasimof, US Army retired, LICSW, White River Junction VAMC, White River Junction, Vermont; Matthew Bouchard, US Army retired, LICSW, South Burlington Vet Center, Burlington, Vermont; and Phillip Trefethen, US Army retired, BA, Environmental Health Coordinator, White River Junction VAMC, White River Junction, Vermont. They report no financial relationships relevant to the subject of this article.
Clinical Points
- Veterans of the Gulf War and post-9/11 conflicts were exposed to multiple overlapping toxic exposures, including burn pits, industrial pollutants, dust storms, poor air quality, chemical agents, and fuels that are associated with significantly higher rates of mood disorders and cognitive complaints and have neuroimaging findings suggestive of changes in white matter integrity and altered brain metabolism.
- Health care providers play vital roles in the screening of active-duty military and veterans because military personnel are exposed to a range of toxins; therefore, clinicians should ask their patients, “Are you a veteran or are you currently in the military?” as the answer to this screening question will help to steer the patient to the proper resources.
- Passage of the PACT Act in 2022 ensures that active-duty personnel and veterans will be screened for toxic exposures and involves a 5-to 10-minute screening to identify potential exposures to toxins during one’s military service, and it is repeated every 5 years.
- GRAIL’s multicancer early detection test is available to special operations veterans receiving care through Home Base in collaboration with Massachusetts General Hospital’s Cancer Early Detection and Diagnostic Clinic to help people live longer, healthier, better lives.
References (80)

- United States House of Representatives. 38 U.S.C. § 1119: Presumptions of toxic exposure. 2022. Accessed April 28, 2025. https://uscode.house.gov/view.xhtml?req=(title:38%20section:1119%20edition:prelim)
- Toxic Exposure Research Clearinghouse. Public Health. U.S. Department of Veterans Affairs. Accessed August 3, 2025. https://www.publichealth.va.gov/exposureresearch/index.asp
- Chassé JS, Rossi C, Downs J, et al. Associations between self-reported burn pit exposure and functional status, 1990-2021. Mil Med. 2024;189(9–10):e2107–e2113. PubMed CrossRef
- Hurley RA, Taber KH. Occupational exposure to solvents: neuropsychiatric and imaging features. J Neuropsychiatry Clin Neurosci. 2015;27(1):1–6. PubMed CrossRef
- National Academies of Sciences. Engineering, and Medicine 2018. Veterans and Agent Orange: Update 11. The National Academies Press; 2018.
- Golomb BA. Acetylcholinesterase inhibitors and Gulf war illnesses. Proc Natl Acad Sci USA. 2008;105(11):4295–4300. PubMed CrossRef
- Research Advisory Committee on Gulf War Veterans’ Illnesses. Gulf War Illness and the Health of Gulf War Veterans: Research Update and Recommendations, 2009-2013. US Government Printing Office; 2014.
- U.S. Department of Veterans Affairs. Airborne Hazards and Open Burn Pit Registry. Accessed April 28, 2025. https://www.publichealth.va.gov/exposures/burnpits/registry.asp
- IOM (Institute of Medicine). Long-Term Health Consequences of Exposure to Burn Pits in Iraq and Afghanistan. The National Academies Press; 2011.
- VA Office of Public Health. Environmental health concerns and toxic Wounds. Accessed November 5, 2025. https://www.publichealth.va.gov/exposures/index.asp
- U.S. Department of Veterans Affairs. Exposure to hazardous chemicals and materials. 2023. Accessed November 5, 2025. https://www.va.gov/disability/eligibility/hazardous-materials-exposure/
- National Academies of Sciences. Engineering, and medicine; health and medicine division; board on population health and public health Practice. In: Butler DA, Styka AN, Savitz DA, et al, eds. Assessment of the Department of Veterans Affairs Airborne Hazards and Open Burn Pit Registry. National Academies Press (US); 2017.
- National Academies of Sciences, Engineering, and Medicine. Respiratory Health Effects of Airborne Hazards Exposures in the Southwest Asia Theater of Military Operations. The National Academies Press; 2020.
- National Research Council (US) Committee to Assess the Scientific Information for the Radiation Exposure Screening and Education Program. Assessment of the Scientific Information for the Radiation Exposure Screening and Education Program. National Academies Press (US); 2005.
- United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Sources and Effects of Ionizing Radiation: UNSCEAR 2008 Report Volume II. United Nations; 2011. Accessed May 15, 2025. https://www.unscear.org/unscear/en/publications/2008_2.html
- U.S. Department of Veterans Affairs. Exposure to Radiation During Military Service. Public Health. Accessed May 15, 2025. https://www.publichealth.va.gov/exposures/radiation/sources/index.asp
- Mettler FA, Jr., Upton AC, eds. In: Medical Effects of Ionizing Radiation, 3rd ed. Saunders Elsevier; 2008.
- U.S. Department of Veterans Affairs. Agent Orange. Accessed May 15, 2025. https://www.publichealth.va.gov/exposures/agentorange/
- Institute of Medicine (US) Committee on Health Effects Associated with Exposures During the Gulf War; Fulco CE, Liverman CT, Sox HC, eds. Gulf War and Health: Volume 1. Depleted Uranium, Sarin, Pyridostigmine Bromide, Vaccines. National Academies Press (US); 2000.
- U.S. Department of Veterans Affairs. Mustard Gas or Lewisite Exposure. Public Health. Accessed May 15, 2025. https://www.va.gov/disability/eligibility/hazardous-materials-exposure/mustard-gas-lewisite/
- Institute of Medicine (US) Committee on Veterans’ Health-Related Effects of Herbicides. Long-Term Health Effects of Participation in Project SHAD (Shipboard Hazard and Defense). National Academies Press; 2007.
- U.S. Department of Defense and VA - Project SHAD/112 Public Health Info. VA Project SHAD Page. Accessed May 15, 2025. https://www.publichealth.va.gov/exposures/shad/
- Agency for Toxic Substances and Disease Registry (ATSDR). Camp Lejeune Drinking Water Contamination. ATSDR Camp Lejeune Page. Accessed May 15, 2025. https://www.atsdr.cdc.gov/camp-lejeune/index.html
- U.S. Department of Veterans Affairs (VA). Camp Lejeune water contamination. VA Camp Lejeune Page. Accessed May 15, 2025. https://www.va.gov/disability/eligibility/hazardous-materials-exposure/camp-lejeune-water-contamination/
- PFAS Exposure and Risk of Cancer, National Cancer Institute, Division of Cancer Epidemiology & Genetics, National Institute of Health. Accessed May 15, 2025.https://dceg.cancer.gov/research/what-we-study/pfas?utm_source=chatgpt.com
- Collett G, Bashford T, Whitehead NJ, et al. Occupational incidence of bladder cancer amongst veteran ammunition technicians of the British Army. BJU Int. 2025; 135(6):928–930.
- Brown L. Prince Williams’ ex-instructor dies “after years of inhaling fumes”. The Times; 2025. Accessed May 15, 2025. https://www.thetimes.com/uk/defence/article/prince-williams-ex-instructor-dies-after-years-of-inhaling-fumes-wkpkvb9jz
- Weaver M. Mod Sued by Aircrew Over Alleged Exposure to Carcinogenic Helicopter Fumes. The Guardian; 2024. Accessed May 12, 2025. https://www.theguardian.com/uk-news/article/2024/may/29/mod-sued-over-allegedly-carcinogenic-fumes-from-military-helicopters
- MOPP Analysis. In Field Manual FM3-4/11-9, Field Manual for Nuclear, Biological, and Chemical (NBC) protection. Department of the Army, US Marine Corps; 1992. Accessed May 15, 2025. https://www.gulflink.osd.mil/khamisiyah_ii/khamisiyah_ii_refs/n15en246/Ch2.htm
- U.S. Department of Health & Human Services: Radiation Emergency. Medical Management. Mission Oriented Protective Posture (MOPP) Gear: Military PPE. Accessed May 15, 2025. https://remm.hhs.gov/MOPP.htm
- Toczylowski D, Treyball MP, Letvak S, et al. Caring for Veterans with Toxic Exposures: Veteran Exposure Assessment Screening and Evaluation (VET-EASE) Toolkit. N C Med J. 2023;84(6):373–378. PubMed CrossRef
- US Department of Veterans Affairs. The PACT Act and your VA benefits [Internet]. US Department of Veterans Affairs. . Accessed May 24, 2025. https://www.va.gov/resources/the-pact-act-and-your-va-benefits/
- US Department of Veterans Affairs. Protect Your Health [Internet]. US Department of Veterans Affairs; 2013. Accessed May 24, 2025. https://www.publichealth.va.gov/exposures/
- American Cancer Society. Us Veterans: Cancer Resources – Cancer Risk. U S Veterans Cancer Resources Cancer Risk. Accessed May 24, 2025. https://www.cancer.org/cancer/veterans.html
- Hancock J. John Hancock Provides Multi-Cancer Early Detection Tests to Special Operations Veterans in Collaboration With Home Base. John Hancock. Accessed May 15, 2025. https://www.johnhancock.com/about-us/newsroom/news/john-hancock/2024/11/john-hancock-provides-multi-cancer-early-detection-
- Klein EA, Richards D, Cohn A, et al. Clinical validation of a targeted methylation-based multi-cancer early detection test using an independent validation set. Ann Oncol. 2021;32(9):1167–1177. PubMed CrossRef
- Massachusetts General Hospital. Cancer Early Detection and Diagnostics Clinic. Massachusetts General Hospital. Accessed April 8, 2025. https://www.massgeneral.org/cancer-center/treatments-and-services/cancer-early-detection
- CURE Today. Defining ‘Previvor. Accessed May 24, 2025. https://www.curetoday.com/view/defining-previvor
- American Psychiatric Association. APA’s 69th Convocation of Distinguished Fellows to Feature Pulitzer Prize–Winning Author Siddhartha Mukherjee. Accessed May 24, 2025. https://www.psychiatry.org/psychiatrists/meetings/annual-meeting/blog/apas-69th-convocation-of-distinguished-fellows-to
- Shane L, III. Concern about military toxic exposure injuries remains high among vets. Military Times; 2023. Accessed May 24, 2025. https://www.militarytimes.com/veterans/2023/11/22/concern-about-military-toxic-exposure-injuries-remains-high-among-vets/
- Sagalyn D. Biden Addresses Possible Link Between Son’s Fatal Brain Cancer and Toxic Military Burn Pits. PBS News Hour. 2018. Accessed May 24, 2025. https://www.pbs.org/newshour/health/biden-addresses-possible-link-between-sons-fatal-brain-cancer-and-toxic-military-burn-pits
- Prestige Veteran Medical Consulting. Updated list of military burn pit presumptive conditions. Accessed May 24, 2025. https://prestigeveteranmctx.com/updated-list-of-military-burn-pit-presumptive-conditions/
- U.S. Department of Veterans Affairs. VA PACT Act Performance Dashboard: Issue 48. 2025. Accessed May 24, 2025. https://department.va.gov/pactdata/wp-content/uploads/sites/18/2025/04/VA-PACT-Act-Dashboard-Issue-48_041825-508.pdf
- Rasmussen P, Farmer CM. The promise and challenges of VA community care: Veterans’ issues in focus. Rand Health Q. 2023;10(3):9. PubMed
- Haley RW, Spence JS, Carmack PS, et al. Abnormal brain response to cholinergic challenge in chronic encephalopathy from the 1991 Gulf War. Psychiatry Res. 2009;171(3):207–220. PubMed CrossRef
- Sullivan K, Krengel M, Proctor SP, et al. Cognitive functioning in treatment-seeking Gulf War veterans: pyridostigmine bromide use and PTSD. J Psychopath Behav Assess. 2003;25:95–103. CrossRef
- Chao LL, Abadjian L, Hlavin J, et al. Effects of low-level sarin and cyclosarin exposure and Gulf war illness on brain structure and function: a study at 4 T. Neurotoxicology. 2011;32(6):814–822. PubMed CrossRef
- Mulligan EA, Wachen JS, Naik AD, et al. Cancer as a criterion A traumatic stressor for Veterans: Prevalence and correlates. Psychol Trauma. 2014;6(suppl 1):S73–S81. PubMed CrossRef
- City of Hope. Veterans Often Turn to Military Experience to Help Battle Cancer. Cancer Treatment Centers of America. 2020. Accessed May 24, 2025. https://www.cancercenter.com/community/blog/2020/11/veterans-and-cancer
- Mercier JM, Hosseiny F, Rodrigues S, et al. Peer support activities for Veterans, serving members, and their families: results of a scoping review. Int J Environ Res Public Health. 2023;20(4):3628. PubMed CrossRef
- Booth J. Advocating for Veterans’ Mental Health Gave Me a New Purpose in Life. National Alliance on Mental Illness; 2023. Accessed May 24, 2025. https://www.nami.org/advocate/advocating-for-veterans-mental-health-gave-me-a-new-purpose-in-life/
- Chan M. Veterans Wait 30 Years on Average for the U.S. to Acknowledge Toxic Exposures, New Report Says. NBC News. 2024. Accessed May 24, 2025. https://nbcnews.com/news/us-news/veterans-wait-30-years-average-us-acknowledge-toxic-exposures-new-repo-rcna171371
- Human Resources, University of California, San Francisco. Trauma, Moral Injury, and Grief. UCSF. Accessed May 10, 2025. https://hr.ucsf.edu/wellbeing/coping-and-resiliency-program/cope-program-wellness-resources/trauma-moral-injury-and-grief
- VAntage Point Contributor. VA’s Progress on Treating Cancer Since 2016. VA News; 2022. Accessed May 24, 2025. https://news.va.gov/101361/vas-progress-on-treating-cancer-since-2016/
- Basu AK. DNA damage, mutagenesis and cancer. Int J Mol Sci. 2018;19(4):970.
- Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Benzene [Internet]. Toxic Substances Portal. U.S. Department of Health and Human Services; 2024. Accessed May 24, 2025. https://wwwn.cdc.gov/TSP/ToxProfiles/ToxProfiles.aspx?id=40&tid=14
- Santos C, Dixe MDA, Sacadura-Leite E, et al. Asbestos exposure and malignant pleural mesothelioma: a systematic review of literature. Port J Public Health. 2023; 40(3):188–202. PubMed CrossRef
- Hall EJ, Giaccia AJ. Chapter 2: Molecular mechanisms of DNA and chromosome damage and repair. In: Hall EJ, Giaccia AJ, eds. Radiobiology for the Radiologist. 8th ed. Wolters Kluwer/Lippincott Williams & Wilkins; 2018. PubMed CrossRef
- Reuter S, Gupta SC, Chaturvedi MM, et al. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med. 2010;49(11):1603–1616. PubMed CrossRef
- Baan R, Grosse Y, Straif K, et al. A review of human carcinogens-Part F: chemical agents and related occupations. Lancet Oncol. 2009;10(12):1143–1144. PubMed CrossRef
- Kerkvliet NI. Recent advances in understanding the mechanisms of TCDD immunotoxicity. Int Immunopharmacol. 2002;2(2–3):277–291. PubMed CrossRef
- Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev. 2009;30(4):293–342. PubMed CrossRef
- Brody JG, Rudel RA. Environmental pollutants and breast cancer. Environ Health Perspect. 2003;111(8):1007–1019. PubMed CrossRef
- International Agency for Research on Cancer (IARC). Polychlorinated Biphenyls and Polybrominated Biphenyls. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. IARC; 2016. 107. Accessed May 24, 2025. https://publications.iarc.fr/131
- Kensler TW, Roebuck BD, Wogan GN, et al Aflatoxin: a 50-year odyssey of mechanistic and translational toxicology. Toxicol Sci. 2011;120(suppl 1):S28–S48. PubMed CrossRef
- Groopman JD, Kensler TW, Wild CP. Protective interventions to prevent aflatoxin-induced carcinogenesis in developing countries. Annu Rev Public Health. 2008;29:187–203. PubMed CrossRef
- United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Sources and effects of ionizing radiation. Volume II, Annex B: Effects of radiation exposure on children. UNSCEAR 2013 Report to the General Assembly. United Nations; 2013. Accessed May 24, 2025. https://www.unscear.org/unscear/en/publications/2013_2.html
- Preston DL, Ron E, Tokuoka S, et al. Solid cancer incidence in atomic bomb survivors:1958-1998. Radiat Res. 2007;168(1):1–64. PubMed CrossRef
- White RF, Steele L, O’Callaghan JP, et al. Recent research on Gulf War illness and other health problems in veterans of the 1991 Gulf War: effects of toxicant exposures during deployment. Cortex. 2016;74:449–475. PubMed CrossRef
- Schnurr PP, Green BL. Understanding relationships among trauma, post-tramatic stress disorder, and health outcomes. Adv Mind Body Med. 2004;20(1):18–29. PubMed
- Pietrzak RH, Johnson DC, Goldstein MB, et al. Psychological resilience and post-deployment social support protect against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Depress Anxiety. 2009;26(8):745–751. PubMed CrossRef
- American Cancer Society. Hope Lodge [Internet]. Accessed May 24, 2025. https://www.cancer.org/support-programs-and-services/patient-lodging/hope-lodge.html
- CancerCare. Helping Hand: Resources for people with cancer [Internet]. CancerCare. Accessed May 24, 2025. https://www.cancercare.org/helpinghand/
- Fisher House Foundation. Home [Internet]. Fisher House Foundation. Accessed May 5, 2025. https://www.fisherhouse.org/
- GRAIL, Inc. Galleri®: Multi-cancer Early Detection Test [Internet]. Accessed May 24, 2025. https://www.galleri.com/
- Semper Fi & America’s Fund. Service Member & Family support Program [Internet]. The Fund. Accessed May 5, 2025. https://thefund.org/our-programs/service-member-family-support-program/
- U.S. Department of Veterans Affairs. VET-HOME Portal [Internet]. U.S. Department of Veterans Affairs. Accessed May 24, 2025. https://vethome.va.gov/
- U.S. Department of Veterans Affairs. War Related Illness and Injury Study Center. [Internet]. U.S. Department of Veterans Affairs. Accessed May 24, 2025. https://www.warrelatedillness.va.gov/
- U.S. Department of Veterans Affairs. Environmental Health Coordinators [Internet]. Accessed May 24, 2025. https://www.publichealth.va.gov/exposures/coordinators.asp
- Veterans Benefits Administration. Benefits [Internet]. Accessed May 24, 2025. https://www.benefits.va.gov/benefits/
This PDF is free for all visitors!