Abstract
Objective: In Australia, subsidized psychiatric consultation items in the Medicare Benefits Schedule (MBS) provide essential private psychiatric services. Seasonality in service utilization may affect health care planning. This study examined the seasonal patterns of overall MBS psychiatric consultations and MBS telehealth psychiatric consultations in pre- and postpandemic periods.
Methods: Medicare Item Reports for face to-face and telehealth psychiatric items from 2016 to 2023 were retrieved and compiled. The quarterly time series for total (face-to-face and telehealth) and telehealth psychiatric consultations were analyzed descriptively, using the January–March quarter as the baseline. Linear regression analyses were performed to detect significant seasonal variations by gender and age groups. A sensitivity analysis of the impact of the post–COVID-19 increase in consultations on seasonality was also conducted.
Results: A seasonal pattern was present for total consultations before and after the expansion of telehealth items in the first quarter of 2020. There were peaks in psychiatric consultations in July–September and troughs in January–March, except in patients ≥65 years old. Total consultations were significantly higher in April–June (P = .010) and July–September (P < .001) than in January–March. Seasonal variations were the largest among young patients aged 0–24 years. Seasonality was mostly unaffected by the increase in psychiatric consultations postpandemic. However, seasonality was absent for telehealth consultations.
Conclusion: The seasonality of MBS psychiatric consultations, which was more prominent in young people, may have a practical impact on psychiatric service planning. The lack of seasonal variation in telehealth consultations and its relationship to emergency presentations warrant further research.
Prim Care Companion CNS Disord 2025;27(3):24m03898
Author affiliations are listed at the end of this article.
Subsidized private practice psychiatric consultations included in the Medicare Benefits Schedule (MBS), for which patients are partially reimbursed for payment, are a vital component of Australian psychiatric services.1 According to the Australian Institute of Health and Welfare (AIHW), in 2021/2022, nearly 2.8 million Australians (11% of the population) accessed more than 13 million Medicare reimbursed mental health services, 19% of which were provided by psychiatrists; 2% of the Australian population saw a psychiatrist in 2021/2022.2
Given the role of MBS psychiatric consultations, it is important to carefully study factors that could affect usage levels and service planning. The presence of seasonal variations in psychiatric presentations is well known for various psychiatric conditions.3–7 A recent umbrella systematic review found winter peaks for depressive symptoms within the community and summer peaks for emergency department (ED) self-harm presentations and specifically manic-related hospital admissions.3 Similar spring/summer peaks were also found for total mental health presentations in the Australian data.5 Suicide is 11%–23% more frequent in spring and summer,8,9 and this seasonal increase has been known for centuries.3,10,11 ED suicide attempts are also 1.2–1.7 times higher in spring and summer compared to winter.12
There is a dearth of research on seasonality in outpatient psychiatric services in contrast to psychiatric inpatient care. A recent systematic review of 31 studies concluded that seasonality could be a risk factor for psychiatric admissions through its effects on the psychopathology of severe mental illness.13 However, few studies, with conflicting results, investigated seasonal variations of outpatient presentations in terms of psychopathology.14,15 An early Italian study did not find significant seasonal variation in outpatient consultation numbers.16
The Australian MBS psychiatric consultations may show seasonal usage variations analogous to emergency and hospital mental health services. However, to our knowledge, research on the seasonal patterns of MBS psychiatric consultations is still unavailable. The final evaluation report of the Better Access to Psychiatrists, Psychologists and General Practitioners through the MBS initiative, which examined MBS data from 2018 to 2022, did not explicitly study the seasonality of consultations.17 Similarly, the quarterly data on Medicare-subsidized mental health–specific services in reports produced by the AIHW do not analyze seasonal changes.18
The expansion of MBS telehealth items in March 2020 following the onset of the COVID-19 pandemic, including items for psychiatric consultations, has led to marked increases in telepsychiatry usage.19 In the context of the recent MBS Telehealth Post Implementation Review, which proposes removing initial telehealth consultations, the contrastingly important role of telehealth during the pandemic indicates a revealed patient preference for ongoing use.20 Therefore, the seasonality of telehealth psychiatric consultations also requires examination, because they will likely remain an integral component of MBS psychiatric services.
There have been clear variations in the utilization levels of MBS psychiatric services by demographic groups. According to the AIHW, more females (22 per 1,000 population) received Medicare-reimbursed psychiatric care than males (17 per 1,000 population) in 2022–2023. Additionally, individuals aged 18–24 years were more likely to receive psychiatric services (35 people per 1,000 population) compared with other age groups.18 Therefore, seasonal patterns of MBS psychiatric consultations by gender and age likely differ and should be considered in the analysis.
Improved service planning may be possible with a better understanding of the seasonal patterns of MBS psychiatric consultations. We aimed to examine the seasonal patterns of overall MBS psychiatric consultations and MBS telehealth psychiatric consultations. Additionally, we compared the seasonal patterns of MBS psychiatric consultations before and after the COVID-19 pandemic telehealth expansion.
METHODS
Data Source
This study was a time series analysis using routinely collected MBS claim records. These data were publicly available on the Services Australia website for Medicare Item Reports (http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp).
The quarterly Australia-wide item reports for the MBS psychiatry consultation items (January–March, April–June, July–September, and October–December) were retrieved (Supplementary Table 1). The study analysis period was 8 years, from January 2016 to December 2023. Reports were compiled and merged to produce separate time series for total (face-to-face and telehealth) and telehealth psychiatric consultations.
Statistical Analysis
Descriptive statistics were analyzed. The time series were plotted by gender to observe the seasonal patterns. Using the January–March quarter as the referent, we calculated percentage differences in MBS psychiatric consultations of other quarters throughout the study period.
Using Stata 18,21 we performed a linear regression analysis to examine seasonal changes for total consultations, as the seasonal pattern suggested additive seasonality to the time series trend. The outcome variable was the quarterly consultation count, and the categorical independent variable was the quarters, with the first quarter (January–March) designated as the referent, and April–June, July–September, and October–December each represented by a dummy variable. To help interpret the time trend, a covariate representing the sample mean of the time variable was included in the model. This meant that the seasonal estimates for a given quarter were around the midpoint of the time series. The regression coefficient for a quarter variable indicated the change in consultation count from the baseline (January–March, represented by the constant in the regression model) in that quarter at the midpoint of the time series. A statistically significant seasonal change was inferred when the P value was <.05.
Ethical Considerations
This study used aggregate, deidentified Medicare data approved for release to the public by the Australian federal government through Services Australia. Accordingly, ethics approval was not required.
RESULTS
Total Consultations
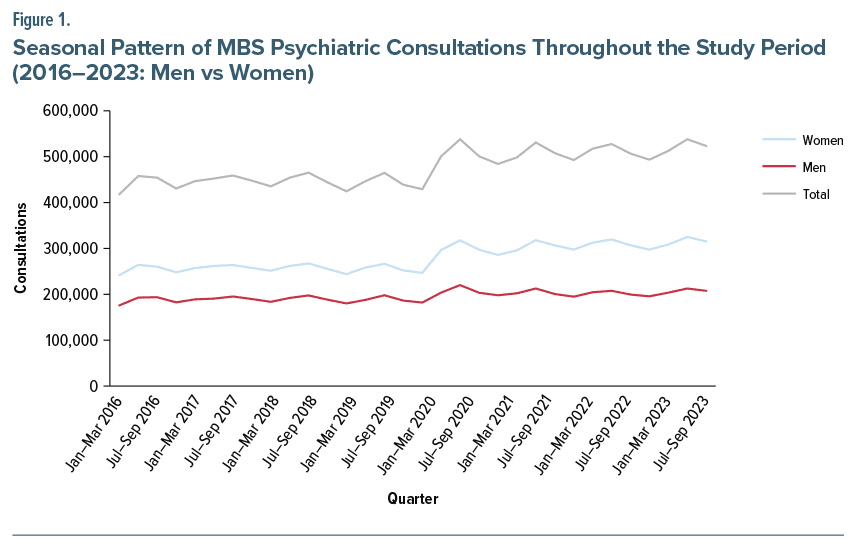
A seasonal pattern was evident throughout the study period. The consultation levels noticeably rose from the second quarter (April–June) of 2020 onward, coinciding with the onset of the COVID-19 pandemic and MBS telehealth item expansion (Figure 1).
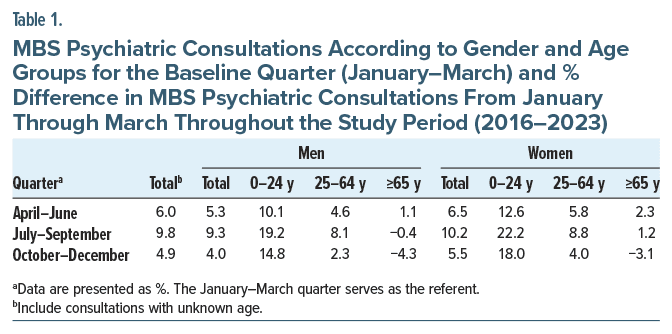
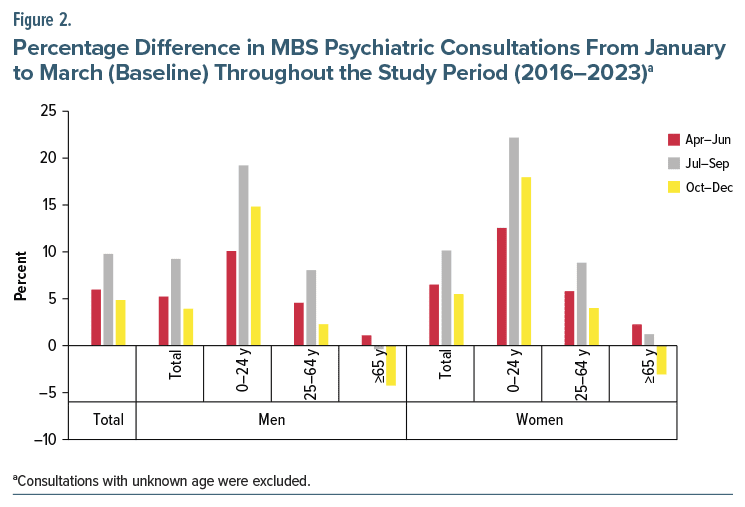
Using the first quarter (January–March) as the baseline for all years studied, differences in quarterly total consultations throughout the study period were calculated for overall total consultations and both genders by age groups. For younger age groups, some MBS items were available in age bands 0–4 years, 5–14 years, and 15–24 years, but others only had data for a single 0- to 24-year age band. Therefore, for total consultations, the combined 0- to 24-year age range was used (Table 1). Total consultations were the highest in the third quarter (July–September) except in 2016 and lowest in the first quarter (January–March) in every year analyzed (Supplementary Figure 1).
This seasonal pattern was true across both genders and most age groups except in the elderly (≥65 years old, Figure 2). The magnitudes of seasonal changes were greater in females than in males. The biggest differences were seen in the third quarter (July–September) in the youngest age group (0–24 years) for both women (+22.2% > in January–March) and men (+19.2% > January–March). The elderly group showed a different pattern, with the second quarter (April–June) having the most consultations (men: +1.1% and women: +2.3%) and the fourth quarter (October–December) having the lowest numbers of consultations (men: −4.3% and women: −3.1%).
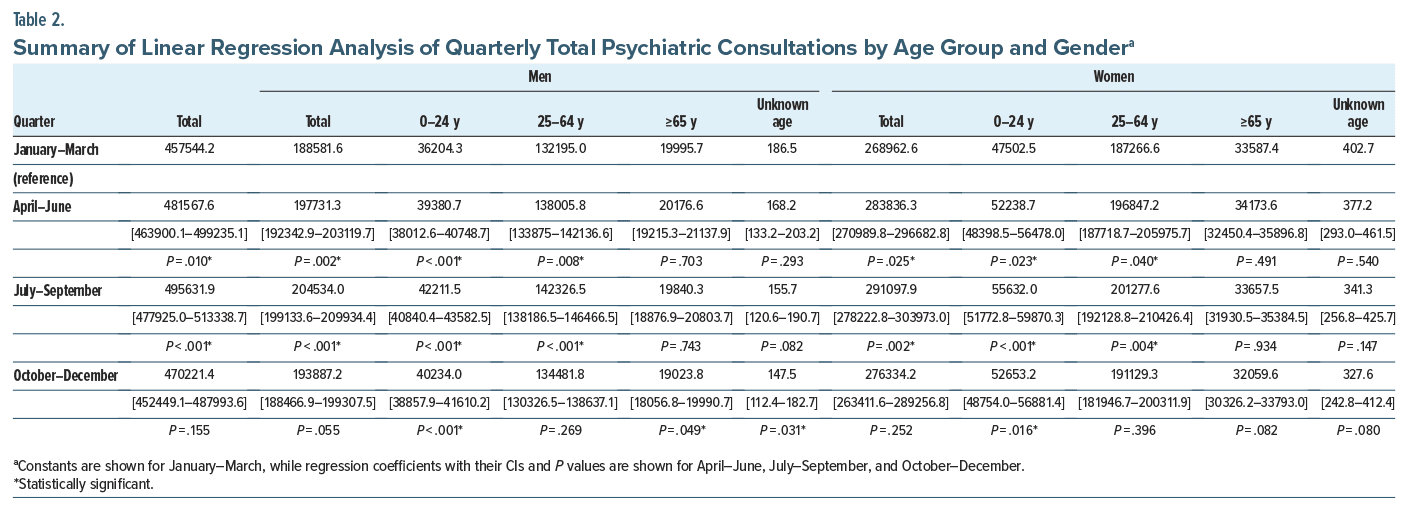
In regression analysis, seasonal changes were statistically significant for April–June and July–September (compared to the January–March baseline) except for the old (≥65) age groups. The differences between October–December and January–March were mostly insignificant except for the young (0–24) age groups (Table 2). There was an overall seasonal pattern of increasing consultations from January–March to April–June, peaking in July–September, and declining again in October–December.
Given the shift in the consultation counts in April–June 2020 after the pandemic onset, a sensitivity analysis of the potential impact of the post–COVID 19 consultation increase on seasonality was conducted. The difference between average quarterly consultations pre- and post–COVID-19 (from January–March 2016 to January–March 2020 and from April–June 2020 to October–December 2023, respectively) was calculated. A 14.8% increase in average quarterly consultations (from 445,136 to 511,090) was observed. Hence, a weighted post–COVID-19 time series adjusted for the post–COVID-19 increase (85% of the actual post–COVID-19 quarterly consultations) was constructed. This hypothetical time series and 2 other weighted post–COVID-19 time series at 80% and 90% of the actual quarterly consultations were tested in linear regression models. The sensitivity analysis results for overall total consultations, total consultations for men, and total consultations for women indicated that seasonality remained significant after the adjustments for post–COVID-19 quarterly consultation counts (Supplementary Table 2). The exceptions were the differences between October–December and January–March for total consultations and men’s consultations at 80% adjusted post–COVID-19 consultation counts.
Telehealth Consultations
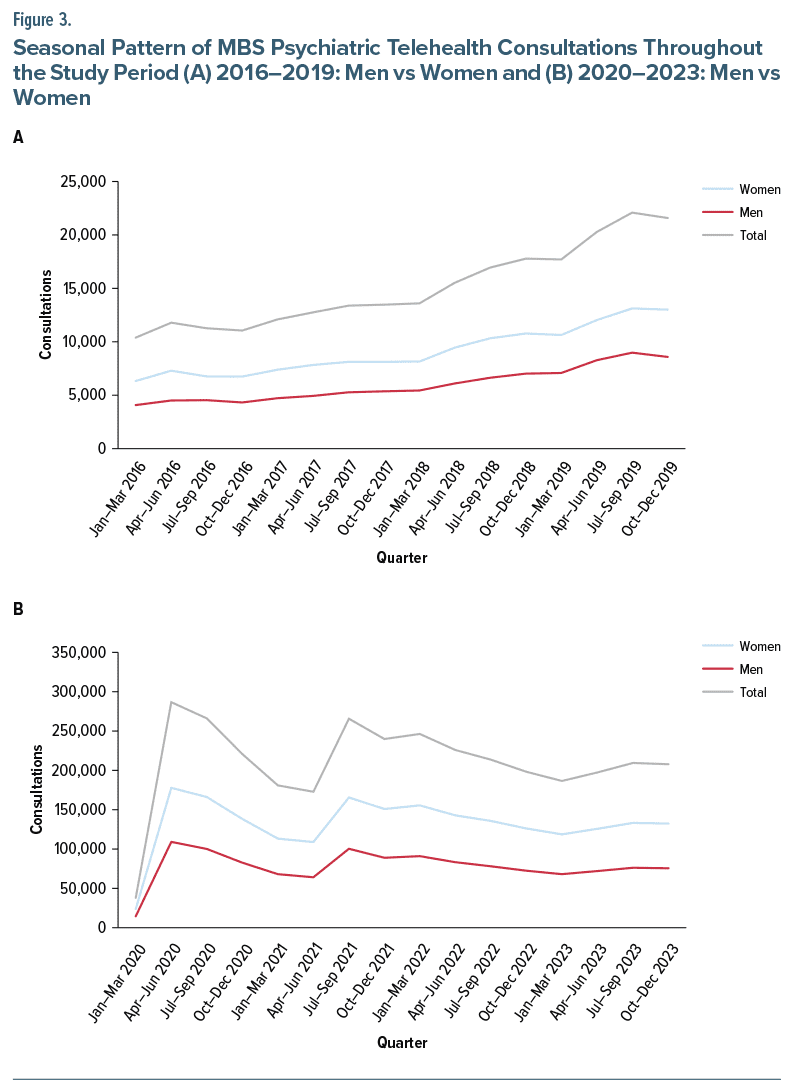
Before 2020, the telehealth consultation usage was low (Figure 3A). From 2020 onward, telehealth consultations increased greatly (Figure 3B). During both periods, no regular seasonal patterns could be observed for telehealth consultations. The seasonal plot further illustrates the lack of overall seasonality for telehealth consultations (Supplementary Figure 2). In the subsequent linear regression analysis, no statistically significant seasonal changes in telehealth consultations were found across all gender and age groups.
DISCUSSION
This study examined quarterly total MBS psychiatric consultations and MBS telehealth psychiatric consultations from January–March 2016 to October–December 2023 for seasonal patterns. We found that seasonality was present for total consultations before and after telehealth item expansion in the first quarter of 2020. There were more psychiatric consultations in the winter (in the Southern Hemisphere) and the least in the summer. This seasonal variation was not altered by the increased numbers of overall consultations following the COVID-19 pandemic. However, for telehealth psychiatric consultations alone, seasonality was absent. Therefore, given the consistent seasonal pattern of total consultations, it can be inferred that face-to-face consultations were the main contributors to the seasonal patterns seen in quarterly MBS psychiatric consultations. Seasonality of psychiatric consultations was most prominent among young patients aged 0 to 24 years.
The seasonal pattern seen in total MBS psychiatric consultations was different from that reported for ED presentations in Australia. Our results show that consultations with private practice psychiatrists peaked in July–September. However, in the analysis of ED psychiatric presentations from 2014 to 2021, Della et al5 found that the highest numbers occurred in the last quarter (October–December) and the second highest in the first quarter (January–March). One possible explanation for this difference is that there is a lag time in presentations between both primary care and referral to private psychiatric practice consultations and ED psychiatric presentations. Over three-quarters of psychiatric cases presented to EDs were urgent or semiurgent.22 Many of such presentations are related to self-harm or suicide attempts.5 Current evidence, albeit inconclusive, suggests that mood symptoms, especially depressive symptoms, tend to peak in winter,3,23 which approximates June to August in Australia and overlaps with the third quarter. It is therefore possible that patients are more likely to seek outpatient consultations in the earlier stages of their illness in winter, while more severe ED psychiatric presentations occur in the context of illness progression in summer. Additionally, cases of acute mania show a strong spring-summer seasonality24,25 and shorter lag time to presentations and are likely to be seen in EDs rather than outpatient clinics. Alternatively, the reduction of outpatient psychiatric consultations in summer may arise from clinicians on vacation during this period, thereby reducing opportunities to prevent or address acute psychiatric presentations within the community setting and leading to emergency presentations. Chronic and growing workforce shortages, as highlighted in the National Mental Health Workforce Strategy 2022–2032,26 might have exacerbated such seasonal effects in service usage, negatively impacting patient care and contributing to increased burnout at work among clinicians.27,28
The finding of greater seasonal variations in psychiatric consultations seen among females may correlate with previous research showing an often higher likelihood for seasonal mood disorders in females.3 We also found that those aged below 24 years demonstrated the greatest seasonal variations in psychiatric consultations. The differences in quarterly total consultations between July–September and January–March were roughly one-fifth of the baselines for both men and women. This strong seasonal trend may also relate to the possible stress associated with being at school or university, which could relate to increased workload issues,29,30 examination stress,31 and peer interaction issues, eg, social exclusion.32 It is possible that in the summer months (associated with extended holiday breaks), these specific school- and university-related pressures may not be as prominent. Schools may be more likely to refer children with issues for mental health assessment on school recommencement, after holidays. Additionally, clinical factors might have contributed, as mood disorders, which are likely to show seasonal variations, are common diagnoses among younger patients.33,34 The more marked seasonality among younger patients than older individuals might be related to the underlying evolving seasonality of brain functions over the lifespan, which shows more seasonal fluctuations at a younger age.35 A delayed circadian phase or evening chronotype is more common at a young age36 and correlates with a high seasonality score.37
However, telehealth consultations did not manifest seasonality. As the pre–COVID-19 telehealth items were mostly limited to rural and remote areas and had low usage, we focus our discussion on the post–COVID-19 period, which is more relevant. One possibility is that COVID-19–related restrictions were the main driver of telehealth usage, especially in the early phase of the pandemic. COVID-19 significantly disrupted mental health services across the world.38 Season-related factors became less influential as COVID-19–related lockdowns meant that providers and patients might not have been away from their homes (on holidays) and hence were more likely to be available for consultations. Nonetheless, the absence of seasonal variations in telehealth consultations persisted beyond COVID-19 waves until the last quarter of 2023, when COVID 19–related movement restrictions were mostly removed. The reason for this phenomenon is unclear. One hypothesis that needs to be tested is that this might be due to the clinical characteristics of the patient subpopulation using telehealth. They could be more stable patients seen at regular intervals, hence not prone to seasonal surges in consultations, whereas unwell patients would more likely present face to face. For instance, in a systematic review of the seasonality of depression, Øverland et al23 found stronger seasonality in “clinical depression” as opposed to “depressive symptoms,” implying greater seasonality with an increasing burden of disease. Patients’ preferences of the modes of consultations across clinical diagnoses and severity and their effects on seasonality also warrant further research.
This study uniquely examined the seasonality of private practice outpatient consultations in Australia over 8 years, covering both before and after the COVID 19 pandemic onset. However, there are some study limitations. The consultation data used in this study were derived from routinely collected MBS claims records. We could quantify the number of consultations but could not determine how many individuals in a specific age group or gender had a consultation in the study period. There could be a lag from when a consultation occurred to when the claim was processed and recorded. For the younger age groups, we could not differentiate children, adolescents, and young adults due to data limitations. Furthermore, clinical information, such as diagnoses and illness severity, was unavailable. Because we only examined the seasonality of psychiatric consultations using national data, potential differences in seasonality across states and territories might be missed.
Our study findings have potential implications for psychiatric service planning. Given the large seasonal variations in psychiatric consultations among young people, youth psychiatric services need to properly plan and adjust for clinical resource allocation in anticipation of seasonal variations in demand. Alternatively, low outpatient clinician availability during the holidays may also result in reduced psychiatric consultations. As telehealth consultations lack seasonality, maintaining an outpatient service with both face-to-face and telehealth options may smooth fluctuating workloads over the seasons. Improving access to specialist outpatient services, including telepsychiatry, to meet seasonal increased demands may also help reduce ED and hospital presentations. That outpatient psychiatric consultations are lowest when ED psychiatric presentations peak indicates a potential mismatch of outpatient consultations for acute community presentations, with, speculatively, a possible diversion to EDs. Future research is needed to understand better the factors associated with seasonal variation in psychiatric consultations, and the longer-term effects of telepsychiatry, in this regard.
Article Information
Published Online: May 8, 2025. https://doi.org/10.4088/PCC.24m03898
© 2025 Physicians Postgraduate Press, Inc.
Submitted: September 1, 2024; accepted January 24, 2025.
To Cite: Woon LS-C, Smith D, Della DF, et al. Seasonal variations of Australian Medicare-reimbursed psychiatric consultations between 2016 and 2023: a time series analysis. Prim Care Companion CNS Disord 2025;27(3):24m03898.
Author Affiliations: Academic Unit of Psychiatry and Addiction Medicine, School of Medicine and Psychology, The Australian National University, Canberra, ACT, Australia (Woon, Looi); Department of Psychiatry, Faculty of Medicine, The National University of Malaysia, Kuala Lumpur, Malaysia (Woon); College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia (Smith, Della, Bastiampillai); Consortium of Australian-Academic Psychiatrists for Independent Policy Research and Analysis, Canberra, ACT, Australia (Looi, Bastiampillai).
Corresponding Author: Luke Sy-Cherng Woon, DrPsych, Academic Unit of Psychiatry and Addiction Medicine, School of Medicine and Psychology, The Australian National University, Bldg 8, Level 4, Canberra Hospital, Garran, Canberra, ACT 2605, Australia ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgments: The authors thank Services Australia, which provides public access to the Medicare Item Reports.
Additional Information: The data that support the findings of this study are openly available in Medicare Item Reports at http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp.
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Conventional (face-to-face) office-based psychiatric consultations show clear seasonal changes, especially among young patients.
- Clinical service planning and resource allocation must factor in seasonal demand surges.
- Increased access to telepsychiatry, which lacks seasonality, may help smooth fluctuations in clinical workloads.
References (38)

- Australian Institute of Health and Welfare. Australia’s mental health system. Australian Institute of Health and Welfare; 2023. Accessed April 4, 2024. https://www.aihw.gov.au/mental-health/overview/australias-mentalhealth-services
- Australian Institute of Health and Welfare. Medicare-subsidised mental health specific services. Australian Institute of Health and Welfare; 2023. Accessed April 4, 2024. https://www.aihw.gov.au/mental-health/topic-areas/medicaresubsidised-services
- Della DF, Allison S, Bidargaddi N, et al. An umbrella systematic review of seasonality in mood disorders and suicide risk: the impact on demand for primary behavioral health care and acute psychiatric services. Prim Care Companion CNS Disord. 2023;25(3):22r03395. PubMed CrossRef
- Koch HJ. Seasonality of psychiatric disease exacerbation assessed by evaluation of a consultancy service: a retrospective pilot study. Biol Rhythm Res. 2010;41(2):159–163. CrossRef
- Della DF, Smith D, Looi JC, et al. Seasonal surge for mental health demand in emergency departments. Prim Care Companion CNS Disord. 2024;26(1):23m03629. PubMed CrossRef
- Ali S, Rosychuk RJ, Dong KA, et al. Temporal trends in pediatric mental health visits: using longitudinal data to inform emergency department health care planning. Pediatr Emerg Care. 2012;28(7):620–625. PubMed CrossRef
- Heboyan V, Stevens S, McCall WV. Effects of seasonality and daylight savings time on emergency department visits for mental health disorders. Am J Emerg Med. 2019;37(8):1476–1481. PubMed CrossRef
- Rock D, Greenberg DM, Hallmayer JF. Increasing seasonality of suicide in Australia 1970–1999. Psychiatry Res. 2003;120(1):43–51. PubMed CrossRef
- Galvão PVM, Silva HRSE, Silva CMFPd. Temporal distribution of suicide mortality: a systematic review. J Affect Disord. 2018;228:132–142. PubMed
- Morselli E. Der Selbstmord: Ein Kapitel aus der Moralstatistik. Brockhaus; 1881.
- Durkheim E. Suicide: A Study in Sociology. 2nd ed. Routledge; 1951. https://doi.org/10.4324/9780203994320
- Coimbra DG, Silva ACPE, de Sousa-Rodrigues CF, et al. Do suicide attempts occur more frequently in the spring too? A systematic review and rhythmic analysis. J Affect Disord. 2016;196:125–137.
- Rizavas I, Gournellis R, Douzenis P, et al. A systematic review on the impact of seasonality on severe mental illness admissions: does seasonal variation affect coercion? Healthcare. 2023;11(15):2155. PubMed CrossRef
- Posternak MA, Zimmerman M. Lack of association between seasonality and psychopathology in psychiatric outpatients. Psychiatry Res. 2002;112(3):187–194. PubMed CrossRef
- Singh GP, Chavan BS, Arun P, et al. Seasonal pattern of psychiatry service utilization in a tertiary care hospital. Indian J Psychiatry. 2007;49(2):91–95. PubMed CrossRef
- Balestrieri M, Williams P, Micciolo R, et al. Monthly variation in the pattern of extramural psychiatric care. Soc Psychiatry. 1987;22(3):160–166. PubMed CrossRef
- Department of Health and Aged Care. Evaluation of the better access initiative – final report. Accessed November 30, 2024. https://www.health.gov.au/resources/collections/evaluation-of-the-better-access-initiative-final-report
- Australian Institute of Health and Welfare. Medicare mental health services. Australian Institute of Health and Welfare; 2023. Accessed July 15, 2024. https://www.aihw.gov.au/mental-health/topic-areas/medicare-subsidised-services
- Woon LS-C, Maguire PA, Reay RE, et al. Telepsychiatry in Australia: a scoping review. Inquiry. 2024;61:00469580241237116. PubMed
- Looi JCL, Allison S, Bastiampillai T, et al. Medicare Benefits Schedule (MBS) Review Advisory Committee post-implementation review of MBS telehealth items: abolition of initial telehealth consultations for non-general practitioner specialists. Aust Health Rev. 2024;48(1):34–36. PubMed CrossRef
- Stata Statistical Software: Release 18. StataCorp LLC.; 2023.
- Australian Institute of Health and Welfare. Mental health services provided in emergency departments. Australian Institute of Health and Welfare; 2023. Accessed April 8, 2024. https://www.aihw.gov.au/mental-health/topic-areas/emergency-departments
- Øverland S, Woicik W, Sikora L, et al. Seasonality and symptoms of depression: a systematic review of the literature. Epidemiol Psychiatr Sci. 2019;29:e31.
- Parker G, Walter SD. Seasonal variation in depressive disorders and suicidal deaths in New South Wales. Br J Psychiatry. 1982;140(6):626–632. PubMed CrossRef
- Mulder RT, Cosgriff JP, Smith AM, et al. Seasonality of mania in New Zealand. Aust N Z J Psychiatry. 1990;24(2):187–190. PubMed CrossRef
- Department of Health and Aged Care. National Mental Health Workforce Strategy 2022–2032. Accessed December 1, 2024. https://www.health.gov.au/resources/publications/national-mental-health-workforce-strategy-2022-2032?language=en
- Looi JCL, Wilkes F, Allison S, et al. The RANZCP Workforce Report: Action is needed, now. Australas Psychiatry. 2024;32(5):450–453. PubMed CrossRef
- Royal Australian and New Zealand College of Psychiatrists. Australian workforce survey report 2024. Accessed December 1, 2024. https://www.ranzcp.org/clinicalguidelines-publications/clinical-guidelines-publications-library/workforcesurvey-report-2024
- Cosma A, Stevens G, Martin G, et al. Cross-national time trends in adolescent mental well-being from 2002 to 2018 and the explanatory role of schoolwork pressure. J Adolesc Health. 2020;66(6S):S50–S58. PubMed CrossRef
- Högberg B, Strandh M, Hagquist C. Gender and secular trends in adolescent mental health over 24 years – the role of school-related stress. Soc Sci Med. 2020;250:112890.
- Beck KC, Røhr HL, Reme BA, et al. Distressing testing: a propensity score analysis of high-stakes exam failure and mental health. Child Dev. 2024;95(1):242–260. PubMed CrossRef
- Arslan PDG. School belongingness, well-being, and mental health among adolescents: exploring the role of loneliness. Aust J Psychol. 2021;73(1):70–80. CrossRef
- Polanczyk GV, Salum GA, Sugaya LS, et al. Annual Research Review: a meta analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–365. PubMed CrossRef
- Dalsgaard S, Thorsteinsson E, Trabjerg BB, et al. Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry. 2020;77(2):155–164. PubMed CrossRef
- Zhang R, Volkow ND. Seasonality of brain function: role in psychiatric disorders. Transl Psychiatry. 2023/02/22 2023;13(1):65. CrossRef
- Roenneberg T, Merrow M. Entrainment of the human circadian clock. Cold Spring Harb Symp Quant Biol. 2007;72:293–299. PubMed CrossRef
- Höller Y, Gudjónsdottir BE, Valgeirsdóttir SK, et al. The effect of age and chronotype on seasonality, sleep problems, and mood. Psychiatry Res. 2021;297:113722.
- Brunier A, Drysdale C. COVID-19 Disrupting Mental Health Services in Most Countries, WHO Survey. World Health Organization; 2020.
Enjoy this premium PDF as part of your membership benefits!