Autoimmune encephalitis (AIE) is an immune-mediated condition characterized by an exaggerated response to self-neuronal antigens, making it a common cause of noninfectious encephalitis.1 It can be triggered by factors such as tumors (paraneoplastic) or infections (parainfectious) and in some instances may have an unknown origin (cryptogenic).2 Clinical symptoms encompass a wide spectrum, from behavioral and psychiatric manifestations and autonomic disturbances to movement disorders and seizures, leading to diagnostic challenges and treatment delays.2,3 Variants of AIE include acute disseminated encephalitis, anti–N-methyl-d-aspartate receptor (NMDAR) encephalitis, Hashimoto encephalopathy, LGI1/CASPR2-antibody encephalitis, and limbic encephalitis.4 Diagnosis typically involves various methods, including antibody detection, neuroimaging, and electroencephalography (EEG).1 In this report, we describe a 20-year-old woman with no previous neuropsychiatric history who was diagnosed with stress-induced AIE.
Case Report
A 20-year-old unmarried woman with no personal or family history of psychiatric or neurologic illness and normal intellectual development presented to the hospital with abnormal behavior of < 1 week duration. The behavior was characterized by acute-onset violent outbursts and incoherent speech followed by mutism and urinary incontinence. She had significant stressors prior to the illness in the form of college exam failure and urological surgery. There was no history of fever, loss of consciousness, seizures, head injury, drug use, or vomiting.
On examination, she was conscious with catatonic symptoms of mutism and negativism. Muscle tone was rigid in all 4 limbs with normal deep tendon reflexes. She had bilateral flexor plantar response. There was no neck stiffness. Considering recent stressors, a provisional diagnosis of conversion disorder was given while the patient was being evaluated to rule out other organic causes. Her routine blood investigations, including hemogram, liver function tests, renal function tests, serum electrolytes, blood glucose, erythrocyte sedimentation rate, and thyroid function tests, were within normal limits. Autoimmune antibody tests including antinuclear antibody were nonreactive. She tested negative for HIV and hepatitis B surface antigen. The EEG showed abnormal bilateral diffuse moderate electrophysiologic dysfunction; the chest x-ray was normal. Ultrasonography of the abdomen was normal except for echogenic areas in the gallbladder. Magnetic resonance imaging (MRI) of the brain was normal. However, a cerebrospinal fluid (CSF) sample sent for anti-NMDAR antibody testing was positive. Considering the clinical picture and anti-NMDAR antibody positivity in the CSF, a diagnosis of anti-NMDAR encephalitis was made, and she was started on methylprednisolone pulse therapy. Due to poor response, injection rituximab was also started, to which her psychotic and catatonic symptoms responded well.
Discussion
AIE arises from an immune reaction against self-neuronal antigens, leading to antibody production.2 These antineuronal antibodies can be categorized into 3 groups: those targeting cell surface antigens (CSAab), synaptic antigens, and intraneuronal antigens (INAab), also referred to as onconeural antibodies.2 Patients with AIE linked to CSAab, such as anti-NMDAR antibodies, tend to have a more favorable prognosis. Conversely, individuals with AIE associated with INAab often exhibit limited responsiveness to immunotherapy, and their symptoms tend to be largely irreversible due to T-cell–mediated neuronal damage.2
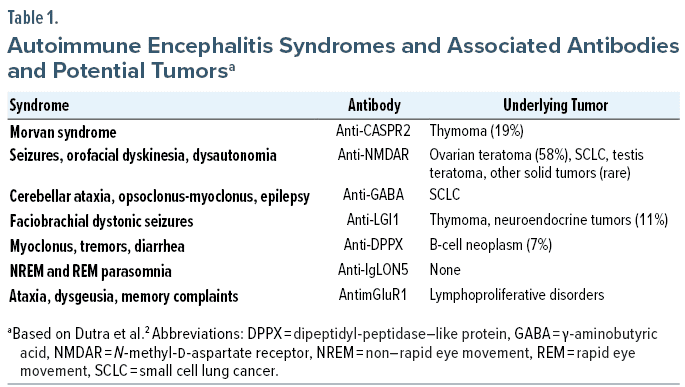
AIE can manifest with various movement disorders, including ataxia, myoclonus, orofacial dyskinesia, and dystonia.2 Seizures, including status epilepticus, are also prevalent.5 Autonomic dysfunctions, such as sinus tachycardia, bradycardia, hypersalivation, hypotension, hyperhidrosis, and constipation, frequently occur in cases of anti-NMDAR encephalitis.6 These clinical presentations often suggest a specific subtype of encephalitis and are indicative of particular antibodies. Additionally, they may be associated with underlying tumors.2 Table 1 illustrates AIE syndromes, associated antibodies, and potential tumor connections.
The diagnosis of AIE relies on clinical symptoms, brain MRI findings indicating inflammation, EEG alterations, and the presence of specific antibodies, which have greatly enhanced AIE recognition due to their high specificity.4 Nevertheless, seronegative patients, who could account for up to 50% of cases, present a diagnostic challenge. Hence, it is crucial to prioritize a thorough clinical history, physical examination, and supportive diagnostic tests like MRI, inflammatory CSF parameters, and EEG in such cases.4
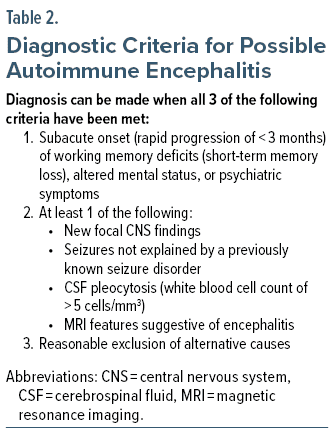
In 2016, diagnostic guidelines for AIE were established,7 and these criteria are reinforced by AIE-specific IgG antibody testing, CSF IgG index, detection of oligoclonal bands, EEG findings, and, in some cases, brain biopsy for definitive diagnosis.4 Additionally, it is worth noting that certain patients with anti-NMDAR encephalitis may exhibit a pattern of generalized rhythmic delta activity with superimposed fast activity, referred to as extreme delta brush.8 The diagnostic criteria for possible AIE is provided in Table 2.7
Considering that our patient lacked a specific infectious trigger, or an underlying cancer associated with AIE, we hypothesize that immune dysregulation induced by stress (specifically, the stress stemming from college exam failure and urological surgery in our case) may have precipitated the development of AIE. Previous reports have documented instances of stress-induced AIE.9 One conceivable mechanism connecting stress to autoimmune conditions entails the activation of the autonomic nervous system, which subsequently disturbs immune functioning and triggers an unregulated inflammatory reaction via the inflammatory reflex.9 In managing such patients, it might be beneficial to consider stress management and behavioral interventions as potential measures to reduce the risk of relapse. However, it is possible that the stress experienced by our patient was purely coincidental.
During the diagnostic evaluation of AIE, it is crucial to include screening for underlying cancer due to the common incidence of paraneoplastic AIE.2 If the initial tumor screening yields negative results but the patient exhibits antibodies typically associated with paraneoplastic cases (such as anti-NMDAR in young adult women, anti-CASPR2 [contactin-associated protein-like 2], anti-AMPAR [α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor], and anti–γ-aminobutyric acid type B), it is advisable to conduct repeat screenings after 3 to 6 months, followed by biannual screenings for the subsequent 4 years.2
Treatment options for AIE encompass corticosteroids, intravenous immunoglobulin, plasma exchange, rituximab, and cyclophosphamide.2 Timely initiation of treatment is crucial, as early immunotherapy has been shown to enhance outcomes.
Conclusion
In summary, AIE exhibits a broad spectrum of neuropsychiatric symptoms. Given the prevalence of seronegative cases, it is crucial to seek diagnostic cues in the patient’s medical history, physical examination, and supportive tests, including EEG, brain MRI, and CSF analysis. Tumor screening is essential due to the frequent association of AIE with cancer. It is important to note that not all patients may have identifiable infectious or neoplastic triggers, and the potential for stress-induced immune dysregulation should be considered. The initiation of treatment should occur promptly, without delay, to enhance overall outcomes.
Article Information
Published Online: March 26, 2024.
https://doi.org/10.4088/PCC.23cr03628
© 2024 Physicians Postgraduate Press, Inc.
Submitted: August 22, 2023; accepted November 15, 2023.
To Cite: Hanana F, Kalathil B, Uvais NA, et al. Stress-induced autoimmune encephalitis. Prim Care Companion CNS Disord. 2024;26(2):23cr03628.
Author Affiliations: Hamad Medical Corporation, Qatar (Hanana); Department of Internal Medicine, Iqraa International Hospital and Research Centre, Calicut, Kerala (Kalathil, Mohammed); Department of Psychiatry, Iqraa International Hospital and Research Centre, Calicut (Uvais).
Corresponding Author: N. A. Uvais, MD, Iqraa International Hospital and Research Centre, Calicut, Kerala, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (9)

- Gole S, Anand A. Autoimmune Encephalitis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023.
- Dutra LA, Abrantes F, Toso FF, et al. Autoimmune encephalitis: a review of diagnosis and treatment. Arq Neuropsiquiatr. 2018;76(1):41–49. PubMed CrossRef
- Soto Ontoso M, Piernas González RA, Ramírez Martínez I, et al. Clinical diagnosis of an autoimmune encephalitis presented as a manic episode with psychotic symptoms: a case report. Case Rep Psychiatry. 2022;2022:2460492. PubMed CrossRef
- Orozco E, Valencia-Sanchez C, Britton J, et al. Autoimmune encephalitis criteria in clinical practice. Neurol Clin Pract. 2023;13(3):e200151. PubMed CrossRef
- Davis R, Dalmau J. Autoimmunity, seizures, and status epilepticus. Epilepsia. 2013 Sep;54 suppl 6(0 6):46-49.
- Yan L, Zhang S, Huang X, et al. Clinical study of autonomic dysfunction in patients with anti-NMDA receptor encephalitis. Front Neurol. 2021;12:609750. PubMed CrossRef
- Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404. PubMed CrossRef
- Lee SK, Lee ST. The Laboratory diagnosis of autoimmune encephalitis. J Epilepsy Res. 2016;6(2):45–50. PubMed CrossRef
- Moideen S, Thomas R, Suresh Kumar PN, et al. Psychosis in a patient with anti-NMDA-receptor antibodies experiencing significant stress related to COVID-19. Brain Behav Immun Health. 2020;7:100125. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!