Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(3):25f03944
Author affiliations are listed at the end of this article.
Have you ever wondered what you should teach, where you should teach, and how you should teach medical students about psychiatry given limited time? Have you been unsure about how you might apply adult learning theory to your teaching and the learning of your trainees? Have you puzzled over how you could evaluate your teaching and the learning of your students? If so, the following vignette and discussion should prove useful.
CASE VIGNETTE 1
Ms A, a third-year medical student with an interest in psychiatry, was embarking upon her first psychiatry clerkship. Nevertheless, she was anxious about interacting with patients who have psychiatric disorders, as her prior clinical experiences had been in internal medicine and surgery. On the first day of her rotation, she was assigned to the consultation-liaison (C-L) psychiatry service. Her attending psychiatrist took her to the intensive care unit to conduct a suicide risk assessment on a 38-year-old man (with a history of depression) who was admitted following an intentional drug overdose. Although she appreciated the importance of evaluating suicide risk, establishing rapport with the patient, performing a mental status examination (MSE), understanding the patient’s clinical status, and conducting a focused physical examination, Ms A felt challenged by not knowing what to ask or how to begin the interview. She had hoped that her attending would have discussed a strategy for the interview (eg, clarification of his suicidal intent and plan, emotional and cognitive status, whether to use direct questions) before they had entered the patient’s room.
CASE VIGNETTE 2
Mr B, a fourth-year medical student, was rotating on an advanced psychiatry elective in preparation for pursuing a career in oncology. Although he had already completed a core psychiatric clerkship, his primary focus during this rotation was on understanding how to conduct a psychiatric assessment in those with a comorbid medical condition (eg, cancer). While working in an outpatient psychosocial oncology clinic, Mr B accompanied an attending psychiatrist for an assessment of a 52-year-old woman with chronic schizophrenia who had been diagnosed with breast cancer several months earlier. During the interview, the patient expressed concerns about being able to manage her psychiatric condition alongside her oncologic treatments and fears about her prognosis. Mr B felt overwhelmed by attempting to complete a psychiatric assessment, provide treatment recommendations, and offer support during their limited encounter.
DISCUSSION
Why Is It Important to Teach Medical Students About Psychiatry?
Given the prevalence of mental health disorders worldwide, psychiatric education is an essential component of medical training. Mental illnesses are increasingly recognized as being significant causes of disability-adjusted life years, which affect individuals, communities, and health care systems around the globe.1 Moreover, mental health conditions commonly co-occur with and complicate the management of other medical illnesses, underscoring the importance of comprehensive training for all health care providers. Nonetheless, medical students and medical residents often report feeling less confident about treating psychiatric conditions than other medical problems, which highlights the need for having an enhanced psychiatry curriculum.2 Many psychiatry clerkships attempt to focus on interviewing skills, the importance of the doctor-patient relationship, the diagnosis and management of psychiatric (eg, anxiety, mood, psychotic, personality, substance use, and cognitive) disorders, psychopharmacology, and assessments for suicide and violence. However, training about other issues (eg, professionalism, transition to the profession, medical ethics, and forensic matters) is often addressed in preclinical courses and nonpsychiatric clerkships (eg, internal medicine, primary care, family medicine, obstetrics, and gynecology). Ideally, efforts by teachers of several disciplines should be coordinated to link educational endeavors to issues raised during clinical practice so that students can see patients with comorbid psychiatric and medical/surgical problems; read about their diagnosis, evaluation, and management; listen to didactics, seminars, and bedside rounds where these topics are discussed; and obtain practical experience by embarking on interventions and procedures. However, each discipline is faced with the daunting task of teaching students the essential elements of their field in a limited time frame, while keeping education relevant to their trainees. This makes interdisciplinary education challenging, as many curricular efforts strive to expose students to the “low-hanging fruit” of their field and by extension fail to address subtleties raised by clinical practices (eg, coping with serious medical illness by patients and their family members, grief, health literacy, and social determinants of health). Psychiatric conditions are prevalent in all medical/surgical disciplines. Moreover, they arise from a complex interplay of myriad factors, including an individual’s genes, life experiences, and societal influences. Considering these different variables allows trainees to develop a nuanced understanding of psychiatric conditions beyond symptomatology.3 This understanding is crucial to making an accurate diagnosis and effective interdisciplinary collaborations in clinical settings. Psychiatric education also reduces stigma among health care workers. Such stigmatizing attitudes toward individuals with mental illness can interfere markedly with the delivery of appropriate (and compassionate) patient care. Targeted educational interventions can reduce stigma, foster empathy, and lead to more humane interactions, which are likely to improve clinical outcomes.4
The evolving requirements of modern medical education also underscore the necessity for enhanced psychiatric training. Health care is becoming increasingly oriented toward a holistic model, and psychiatric education must evolve to reflect psychosocial and biological integration to better equip trainees for the complexities of clinical practice. The clinical setting itself serves as a crucial environment in which students first encounter psychiatric illness and learn from hands-on educational experiences.5 In particular, C-L psychiatry rotations effectively expose students to psychiatric care within medical and surgical settings, which strengthens their understanding of mental health integration.6
Robust psychiatric training provides future health professionals with the skills needed to address a variety of mental health issues among diverse patient populations. A comprehensive education in psychiatry will enable providers to integrate psychosocial aspects and medical knowledge to improve health care delivery. Moreover, psychiatric training has the potential to alleviate the current shortage of mental health practitioners by stimulating interest in the field and aiding in recruitment and career development.7 Strengthening educational programs ensures that all health care practitioners are prepared, regardless of their specialty, to identify, manage, and appropriately refer patients with psychiatric conditions to specialty providers, thereby fostering a more effective health care system.
Which Topics Related to Psychiatry Should Be Taught to Every Medical Student?
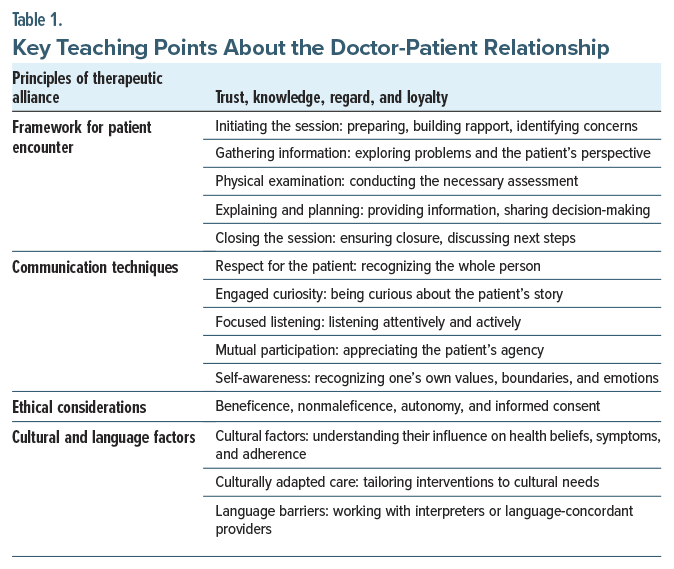
The doctor-patient relationship and communication skills.
Among interpersonal relationships, the doctor-patient relationship is one of the most intimate, requiring communication between individuals having unequal positions about issues of vital importance.8 It is built on knowledge, experience, and trust, which fosters understanding, confidence in care, commitment, and a sense of personal support.9 Effective communication enhances patient satisfaction, adherence, and outcomes,10 underscoring the importance of teaching students how to communicate effectively with patients. Having a structured framework that guides patient encounters can improve communication.10 However, building authentic connections requires both communication skills and behavioral techniques. Key components that strengthen effective doctor-patient interactions include respect, engaged curiosity, mutual participation, and self-awareness.11
In addition, the doctor-patient relationship must be rooted in 4 ethical principles: beneficence (the physician’s obligation to act for the patient’s benefit), nonmaleficence (the duty to avoid harm), autonomy (the patient’s right to make informed decisions), and informed consent.12 Given the growing diversity of patient populations, effective communication in clinical encounters requires that providers be well-equipped to navigate the influences of sociocultural identities.13 To foster meaningful interactions and enhance patient care, providers must recognize and address language barriers (eg, by utilizing professional interpreters or matching patients with language-concordant providers whenever possible).14 By prioritizing education about communication, the doctor-patient relationship and patient care can be enhanced (Table 1).
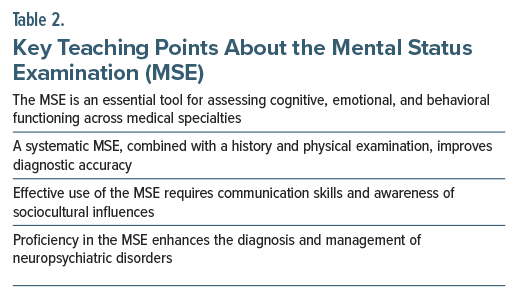
The mental status examination. The MSE is a key component of undergraduate medical education and an essential skill for all clinicians, not just those specializing in psychiatry or neurology.15 As a fundamental part of the psychiatric interview, the MSE systematically assesses cognitive, emotional, and behavioral functioning.16 Its broad applicability across various disorders and clinical settings makes it an essential examination technique for a wide range of health care providers.17
The MSE follows an organized clinical approach to evaluate a patient’s state of mind by examining multiple cognitive domains. When combined with a comprehensive neuropsychiatric history and relevant physical or neurological findings, the MSE allows the clinician to reach an accurate diagnosis.15 The core components of the MSE include appearance, behavior, motor activity, speech, mood, affect, thought process, thought content, perceptions, cognition (eg, alertness, orientation, attention, memory, and abstract reasoning), insight, and judgment.18
Medical trainees must become proficient in recognizing and accurately naming psychiatric signs and symptoms, as these are foundational steps toward clinical competency.19 However, while memorizing the definitions of psychiatric symptoms and the sequence of questions needed to elicit them is an important starting point, applying the MSE in real-world clinical evaluations can be challenging.16 The MSE is not merely a “technical skill”; rather, it is an interactive clinical interview that requires strong communication abilities.
Moreover, interpreting MSE findings requires consideration of cultural background, native language, level of education, literacy, and other social factors, as these elements can significantly influence the evaluation.20 Despite its complexity, mastering the MSE is an attainable goal through a solid understanding of its key components and consistent practice (Table 2). Clinicians who are proficient in conducting the MSE can diagnose a wide range of disorders with cognitive and neuropsychiatric manifestations, thereby improving patient outcomes.17
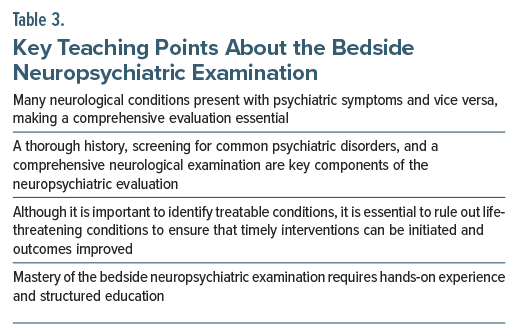
The bedside neuropsychiatric examination.
Neuropsychiatry focuses on the evaluation and management of patients with symptoms that lie at the intersection of neurology and psychiatry. Increasingly, it has become evident that many neurological conditions present with behavioral and affective symptoms, while psychiatric disorders can also have neurological anifestations.21 Given this overlap, a thorough history, screening for common psychiatric illnesses, and a comprehensive neurological examination are essential components of a neuropsychiatric evaluation. In C-L psychiatry, a neuro-medical-contextual approach has been proposed for psychiatric evaluations. This approach prioritizes the central nervous system (CNS), medical conditions that contribute to the neuropsychiatric presentation, and social and contextual factors.22 This framework underscores the critical role of the bedside neurological examination.
The scope of the neurological examination depends on the clinical context, the experience of the evaluator, and the setting.23 However, a thorough assessment should include key components (eg, the MSE, inspection of cranial nerves, the motor examination, assessment of reflexes, the sensory examination, and evaluation of cerebellar function and gait).21 In many cases, a focused examination is sufficient; however, determining which aspects to assess requires clinical experience. Neurological abnormalities should always be interpreted in the context of the patient’s history and other examination findings. Rating scales can complement the neuropsychiatric evaluation by providing a standardized approach to cognitive assessment. Self-report scales may also help identify symptoms that patients may not disclose spontaneously. However, these tools have limitations (and are affected by age, education, hearing, vision, and language barriers that can influence their interpretation).23
Importantly, several treatable neuropsychiatric conditions can be life-threatening if not promptly recognized, including Wernicke’s encephalopathy, neuroleptic malignant syndrome, serotonin syndrome, autoimmune encephalitis, Wilson disease, and hepatic encephalopathy among others.23 A thorough and well-executed neuropsychiatric examination is critical for timely diagnosis and intervention, ultimately improving patient outcomes. Given its significance in clinical practice, teaching medical trainees how to perform and interpret a neuropsychiatric examination is essential for high-quality patient care (Table 3).
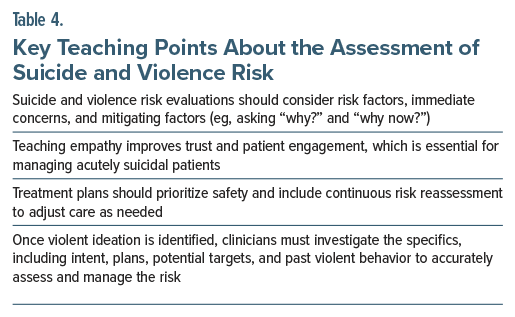
Assessment of suicide risk and the risk of violence.
Despite increasing attention to mental health in the United States, suicide rates continue to rise.24 All mental health professionals must be proficient in suicide risk assessment, and there is a growing call for broader training among other clinicians.25 Comprehensive evaluations are essential, incorporating both established risk factors (eg, mental illness, prior suicide attempts, medical conditions, family history, and access to lethal means)26 and immediate concerns like suicidal ideation, intent, and recent stressors.27 However, risk factors alone do not predict suicide, which highlights the necessity of a thorough and nuanced assessment. Moreover, factors that mitigate the risk of suicide must be assessed (eg, the role of faith to the individual, the presence and access to a supportive network, future orientation, intrapsychic and interpersonal strengths, and prior successful coping efforts). Managing acutely suicidal patients can be emotionally demanding, making it essential to equip trainees with the skills needed to navigate these challenges. Teaching empathy as a core communication skill fosters trust and improves patient engagement in treatment.27 Following assessment, treatment planning should prioritize patient safety, determine the appropriate level of care, integrate pharmacologic or psychotherapeutic interventions, and include ongoing risk reassessment.26
Clinicians must also be prepared to assess violence risk across various settings. While the relationship between psychiatric illness and violence is complex and often misunderstood,28 research indicates that serious violence is uncommon among individuals with mental disorders.26 Although the most reliable predictor of future violence is a history of violent behavior, additional risk factors include substance use, young age, male gender, and lower socioeconomic or educational status.26 Violence against health care workers is an increasing concern, underscoring the importance of structured risk assessments.29 As with suicide risk, evaluating violence risk begins with a comprehensive mental health assessment. When violent ideation is identified, clinicians must explore key details (eg, intent, plans, potential targets, and past violent behavior) (Table 4).30 Teaching these skills is essential to ensuring clinicians can accurately assess and effectively manage safety risks, ultimately improving patient care and clinician well-being.
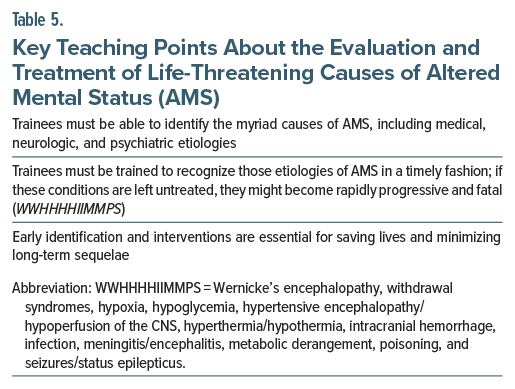
Evaluation and treatment of life-threatening causes of altered mental status. Alterations of mental status are both commonplace and problematic. Moreover, altered mental status (AMS) is a broad clinical term with myriad manifestations (signs and symptoms) and etiologies. AMS results from abnormalities in every organ system, and as such, may be categorized as medical, neurologic, or psychiatric.31 Some conditions with an AMS are rapidly progressive and life-threatening, and these require timely diagnosis and treatment to avoid catastrophe (ie, death). These can be recalled by the mnemonic WWHHHHIIMMPS, where each letter represents a different etiology for a life-threatening condition: Wernicke’s encephalopathy, withdrawal syndromes, hypoxia, hypoglycemia, hypertensive encephalopathy/ hypoperfusion of the CNS, hyperthermia/hypothermia, intracranial hemorrhage, infection, meningitis/ encephalitis, metabolic derangement, poisoning, and seizures/status epilepticus.32 Medical trainees must be equipped with the knowledge and skills to identify aberrations in the mental status, to evaluate their etiologies, to differentiate psychiatric from medical causes of AMS, and to intervene in a timely fashion. Timely detection and effective interventions are crucial in saving lives and minimizing long-term sequelae. Understanding the approach to diagnosis and treatment for these conditions ensures that trainees will consider the varied manifestations and etiologies of AMS and not overlook potentially fatal conditions (Table 5).
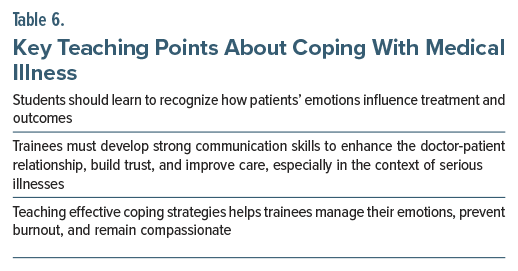
Coping with medical illness. Trainees must become adept at appreciating how their patients cope with medical illness, as coping directly impacts patient well-being and quality of care. Illness, especially when it is chronic or life-threatening, often engenders enormous emotional, psychological, and physical challenges for patients. Therefore, it is crucial to understand how people cope and how therapeutic interventions can be tailored to a patient’s coping style, as patients’ understanding and emotional responses to their illness significantly influence treatment choices, their psychological well-being, and the overall progression of their condition.33 For medical trainees, learning to communicate effectively with patients who are struggling to adapt to their illness or situation helps to foster empathy, build trust, and improve patient outcomes. In addition, physicians must realize that they experience powerful emotions when managing serious illnesses in their patients, and they would be well served to develop coping strategies to prevent burnout and maintain a compassionate approach to care. Teaching these skills early in medical training helps foster a more holistic, patient centered approach to medicine, which equips future physicians with the tools they need to manage both their patients’ and their own emotional needs (Table 6).
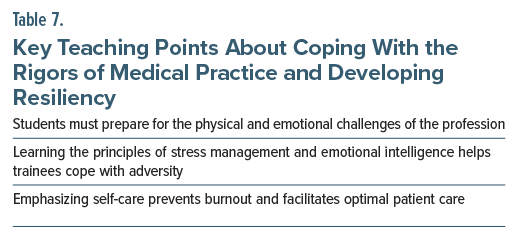
Coping with the rigors of medical practice/resiliency. Educating medical students about the rigors of medical practice and the importance of resiliency is crucial for their long-term success and well-being. Medicine is a demanding field, both physically and emotionally. It often requires spending long hours, making difficult decisions, and confronting the emotional burden of caring for patients who suffer. Managing these demands requires physical endurance, good health, appropriate knowledge and skills, and the ability to respond effectively to challenges.34 Without proper preparation, medical trainees can become overwhelmed by these challenges, which leads to burnout, compassion fatigue, or mental health struggles. Teaching resilience, through learning stress management techniques, developing emotional intelligence (eg, self-awareness), and fostering a supportive environment, empowers trainees to navigate a difficult profession while maintaining their health and compassion. Recognizing that adversity is inherent in medical practice helps future physicians develop coping strategies and a positive mindset, enabling their careers and relationships with patients to thrive. In addition, cultivating resiliency early in training encourages trainees to seek help when it is needed and to maintain a balanced approach to work and life, which ultimately benefits them and their patients (Table 7).
Who Should Teach About Psychiatry, and Where Can Lessons Be Taught?
Ever since the physician widely acknowledged as the father of modern medicine, Sir William Osler, led the medical service at the Johns Hopkins Hospital, the field of medicine has employed an apprenticeship model.35 Students have largely learned by observing more senior clinicians, who have served as role models for how to deliver clinical care. With time and experience, trainees have been granted increasing levels of autonomy and agency before they became responsible for teaching other learners. In medical education, this model has been widely known as “see one, do one, teach one.” For many years, this model has been applied in various medical fields (eg, surgery36 and psychiatry37).
Traditional psychiatry clerkships in US medical schools have been criticized for their focus on care delivered on psychiatric inpatient units, even though care in these settings represents only a small percentage of psychiatric practice venues.38 While inpatient psychiatric units offer opportunities for learning about severe psychiatric syndromes and disorders (eg, psychosis, mania, and major depressive disorder), limiting exposure during training to those who warrant inpatient psychiatric treatment can create the impression that all psychiatric illnesses are chronic and severe. After all, patients who are impaired enough to be hospitalized are more likely to suffer from severe psychiatric conditions.6
Moreover, having students evaluate and treat psychiatric outpatients is not without its challenges.6 Students who are unfamiliar with nuanced patient stories may not appreciate the extent to which the doctor-patient relationship contributes to the therapeutic process in outpatient practices. Both clinicians and patients may be reluctant to allow students into office appointments, given issues of privacy and confidentiality.39 These challenges have led psychiatric educators to search for other opportunities that can expose medical students to situations from which to learn.
C-L psychiatry rotations on medical-surgical units offer an excellent solution to this dilemma.40 Because C-L psychiatry sits on the boundary of medicine and psychiatry, it is ideally situated for medical student psychiatry clerkships. Far more medical students will matriculate into internal medicine, pediatrics, or surgical specialties than into psychiatry. At present, physicians in these nonpsychiatric specialties often feel ill-prepared to confront the psychiatric conditions that complicate the diagnosis and management of their patients.41,42 Unfortunately, many hospitals lack dedicated adult and pediatric psychiatry C-L services; thus, many graduating students find themselves working in settings without having had experience managing individuals with comorbid psychiatric and medical problems.
Teaching psychiatry on medical-surgical floors encourages horizontal and vertical models of learning.43 Horizontal models of education establish links between topics that are being taught simultaneously (eg, systems-based approaches to teaching about diagnosing an AMS, ie, neurologic, cardiologic, and respiratory etiologies). The vertical approach features domains having looser connections to each other (eg, substance use disorders and cancer-related depression); however, recurrent themes exist (eg, the importance of identifying psychosocial factors during the assessment of patients).
Clinician-educators who care for patients (eg, attendings, residents, fellows, and allied health professionals) can deliver apprentice-style teaching at the bedside.44 Such teaching at the bedside provides the opportunity to observe students’ interactions with patients (and vice versa) and to have trainees observe their teachers conducting interviews and examinations. Care at the bedside represents the optimal location for trainees to observe, learn, and practice interviewing skills and techniques, as well as strategies for patient and family education, shared decision-making, approaches to the physical examination, bedside manners, and the use of rating scales and screening tools.
Teaching rounds, held in conjunction with bedside teaching, have long been a mainstay of academic psychiatry.45 These rounds generally involve the presentation of a case by a student with a discussion that focuses on the biological, psychological, and social factors that affect patients so that a deeper understanding will be gained and evaluation and treatment options reviewed. More generally, teaching rounds facilitate learning about how to develop a case formulation and hone skills through effective communication with other clinicians. In addition, adult learning theory suggests that the process of teaching what one knows to another person requires cognitive manipulation of the material in a way that supports deeper learning.7
Dedicated teachers can deploy time-honored teaching methods (eg, observing clinical interviews, running case conferences, delivering didactic lectures, and reviewing readings [from journal articles or C-L textbooks]).44 With each of these approaches, educators can also use emerging learning tools and technology to teach (eg, with simulations, communication apps, social media, and problem-based learning).7
How Can Adult Learning Theory Be Applied to Your Teaching and the Learning of Students?
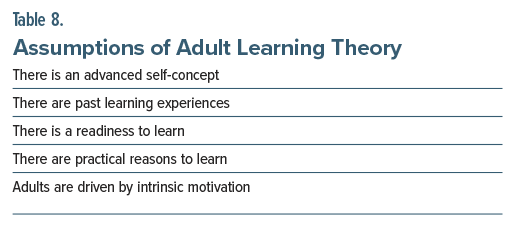
Several decades ago, Knowles46 defined adult learning theory as “the art and science of helping adults learn,” and this theory has subsequently guided psychiatric teaching strategies.7 Adult learning theory is based on several assumptions (Table 8).
Advanced self-concept. Adults are presumed to have a more mature self-concept (ie, a belief about oneself), and they prefer to take part in directing their own learning. While medical students are still consolidating their identity as physicians, educators would be well served to stress what psychiatry shares with the rest of medicine rather than to emphasize its unique characteristics.47 Psychiatric education should have at its core a medical approach that is relatable to nonpsychiatric colleagues, eg, diagnosis guides treatment, and each has an impact on prognosis. Indeed, confident use of the medical model for the diagnosis and treatment of psychopathology bridges the gap between psychiatry and the rest of medicine.
Past learning experiences. Another assumption is that adults have a bevy of learning experiences upon which to draw and thus respond well to personalized approaches to education. Although psychiatry rarely lends itself to instantaneous solutions, many psychiatric and neuropsychiatric presentations can be reversed quickly and completely, eg, catatonia (via use of intravenous lorazepam and/or electroconvulsive therapy) and delirium (via identification and correction of its neuro-medical etiologies), which offers satisfaction to learners.6 In addition, more exposure to these conditions is warranted given that they are often under-detected and misdiagnosed in medical-surgical settings by psychiatrists and nonphysicians. Medical students frequently know about diagnostic tests (eg, the hemogram, electrolyte levels, neuroimaging scans, an electroencephalogram, an electrocardiogram, neuropsychological testing, thyroid function testing, and autoimmune markers) that must be interpreted in psychiatric practices.
Readiness to learn. An additional assumption is that adults have a readiness to learn while they are appreciating the concepts that can be applied to real-world scenarios. Given the prevalence of psychiatric symptoms in the community and in medical settings, students will encounter individuals who experience thoughts of suicide, substance use and misuse, anxiety, fatigue, grief, hallucinations, delusions, changes in appetite, changes in affect, and impaired adherence. Competency in managing these disparate symptoms and conditions is essential for the practice of clinical medicine. In this sense, the psychiatry clerkship is relevant for practitioners in every discipline, and the lessons learned from evaluating patients encountered on this rotation are generalizable to the real-world practice of medicine.6
Practical reasons to learn. The next assumption is that adult learners look for, and respond best to, practical and problem-oriented methods to learn. Active participation teaches students to discern between a situation in which a psychiatrist should intervene and one in which another clinician should assume responsibility for care.48 Students must be creative and knowledgeable as they work within a multidisciplinary team to develop a differential diagnosis and treatment approach.6 It is important to consider whether a patient is anxious about an upcoming surgical procedure or paranoid about those who are treating him. Perhaps, he is both anxious and paranoid, suggesting that the student must add acute anxiety to the already apparent psychotic features that characterize the patient’s struggle and must balance the assessment of this anxiety with the recognition that paranoia might also be present. In addition, laboratory values and vital signs must be examined and scrutinized by the interdisciplinary team, including the psychiatric service, to guide appropriate interventions. Students on a psychiatric rotation (especially on the C-L service) can learn the art of creating a psychiatric treatment plan that is tailored to the patient and his or her circumstances, while considering medical concepts that are often thought to be outside of psychiatric practice.
Intrinsic motivation. The final assumption is that adults are driven by, and respond better to, intrinsic motivation rather than extrinsic motivation. When driven by intrinsic rather than extrinsic motivation, it makes sense that educational outcomes would be better. Students can see a patient and then read about what they have seen; this type of learning lends itself to self-driven exploration of causes and treatments of psychiatric symptoms and to greater autonomy and creativity among medical students.6 For example, a patient with delirium might require treatment of agitation (the target symptom) as well as investigation and treatment of the delirium’s cause (eg, creation of a differential diagnosis, ordering/interpreting diagnostic tests, and formulating and implementing timely and appropriate treatment).
Taken as a whole, these principles illustrate the importance of understanding and utilizing new teaching methods. To continue to appeal to the adult learner, teachers of psychiatry should understand and leverage adult learning theory.
How Should Information Be Offered to Students?
The advent of novel educational technologies and methodologies has helped to shift medical education away from a strict apprenticeship model.7 Under this “see one, do one, teach one” model, senior physicians were responsible for the education of their junior colleagues.37 To ensure that information is learned well and efficiently, newer pedagogical practices are often designed in a way that aligns with the principles of adult learning theory. Practices such as a “flipped classroom” or “layered learning” can allow the educational experience to be better tailored to the needs of the learner.
A flipped classroom (Table 9) is a pedagogical practice that has gained popularity in medical education and involves using classroom time for application of knowledge and critical thinking rather than a passive didactic lecture.49,50 Under the flipped classroom model, trainees “flip” activities that may typically be done at home with those that might be done in class in a more traditional model of education. Thus, pre-class activities may consist of more passive learning through assignments (eg, watching videos, listening to podcasts, or reading books or journal articles), while class time is used to reinforce knowledge through interactive discussions, exercises, or case studies.50
Layered learning, also known as a layered curriculum (Table 9), has not been used as broadly in medical education but also aligns well with the principles of adult learning theory. Layered learning refers to a practice wherein trainees can engage with educational material at different levels of complexity. In doing so, students can choose educational materials that better align with their abilities and preferred learning styles. Educational materials are typically tiered by increasing complexity from tasks that involve basic knowledge acquisition, to knowledge application, and finally complex tasks and critical thinking.51
With the flipped classroom or layered learning approaches, newer educational tools that have been previously identified52 lend themselves well to use within these more novel frameworks (Table 9). For instance, online video media (eg, YouTube videos), online curriculum, or podcasts could supplement textbook or reading material as the prework in a flipped classroom or for the basic knowledge acquisition of layered learning. Simulations or case studies could be used for the in-class portion of a flipped classroom or for knowledge application or critical thinking of layered learning.
How Can Learning by Students Be Assessed?
In selecting educational modalities that ensure that information is learned well and efficiently, it is critical to assess what students have learned through these methods. The measurement of progress through assessment is essential in ensuring that the ways in which the trainees are taught are meeting the needs of the trainees.53,54
When assessing trainees, the methods we utilize should be comprehensive and able to assess essential knowledge and skills ideally conveyed through our educational modalities. The specific target of the assessment should be considered as well, as some assessment methods may be better designed to assess certain components of learning (eg, declarative knowledge, procedural knowledge, competence, or performance).53 Table 10 notes several assessment methods that could be useful.
How Did Ms A and Mr B Rate Their Educational Experience, and How Did It Alter Their Practice?
Ms A and Mr B both thoroughly enjoyed their experience on their psychiatry rotations and rated them very highly. However, they each noted that they would have preferred to have had a flipped classroom approach (ie, reading about what they were about to encounter and discussing it with their attending before seeing a patient with a given condition), which would have provided self-directed learning and made them feel better prepared to apply theoretical knowledge to a clinical setting. Instead, they used a “common sense” approach and engaged directly with the patients. They each asked their attending whether they could be prepared before their next clinical encounter. They realized that they learned better when they read, listened to a presentation, discussed the fine points, and received feedback in real time during an interview (to shape the interview as it occurred rather than only after it had been completed). With such layered learning, they believed they could build knowledge progressively, making the challenging experiences more manageable. They learned to approach patient care more systematically (covering biological, psychological, social, cultural, and existential factors), thereby ensuring that they would assess both basic and complex aspects of each patient’s condition. Preparation through role-played exercises facilitated skills (eg, interviewing and conducting a safety assessment) in a safe, controlled environment. Moreover, such an approach built confidence and empathy, while also teaching them how to ask sensitive questions and build rapport with patients. By conducting observed clinical interviews and receiving direct feedback from the attending psychiatrists later in their rotation, they were able to hone their clinical skills and gain confidence in providing psychiatric care. In addition, they engaged in multiple-choice examinations to assess and test their knowledge and growth.
CONCLUSION
Given the prevalence and sequelae of mental health disorders worldwide, psychiatric education is essential to medical training and to the enhancement of the doctor-patient relationship (which is one of the most intimate relationships between individuals). Since effective communication enhances patient satisfaction, adherence, and outcomes, it is important to teach students how to communicate effectively with patients. At the core of the psychiatric interview is the MSE, which systematically assesses cognitive, emotional, and behavioral functioning. Its applicability across disorders and clinical settings makes it an essential examination technique for a wide range of health care providers. Moreover, the use of a neuro-medical approach prioritizes the involvement of the CNS in myriad conditions, especially those that present with an AMS (and that can be life-threatening and treatable, eg, Wernicke’s encephalopathy, neuroleptic malignant syndrome, serotonin syndrome, and autoimmune encephalitis). Trainees must also become adept at appreciating how their patients cope with medical illness, as coping directly impacts patient well-being and quality of care. In addition, every mental health professional must be proficient in assessing the risk of suicide and violence. Because C-L psychiatry sits on the boundary of medicine and psychiatry, it offers an ideal clerkship for medical students. Bedside teaching can be enhanced by use of flipped classrooms and layered learning that can rely on the principles of adult learning theory and allow the educational experience to be tailored to the needs of the learner and relatable to nonpsychiatric colleagues.
Article Information
Published Online: June 17, 2025. https://doi.org/10.4088/PCC.25f03944
© 2025 Physicians Postgraduate Press, Inc.
Submitted: February 19, 2025; accepted April 22, 2025.
To Cite: Lee JH, Rustad JK, Herrera Santos LJ, et al. Time-limited teaching of psychiatry to medical students: flipping the classroom and offering layered learning.
Prim Care Companion CNS Disord 2025;27(3):25f03944.
Author Affiliations: Department of Psychiatry, Harvard Medical School, Boston, Massachusetts (Lee, Herrera Santos, Stern); Department of Psychiatry, Brigham and Women’s Faulkner Hospital, Jamaica Plain, Massachusetts (Lee); Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire (Rustad, Ho); Department of Psychiatry, Larner College of Medicine, University of Vermont, Burlington, Vermont (Rustad); Burlington Lakeside VA Community Based Outpatient Clinic, Burlington, Vermont (Rustad); White River Junction VA Medical Center, White River Junction, Vermont (Rustad); Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts (Herrera Santos, Stern); Department of Psychiatry, Darthmouth-Hitchcock Medical Center, Lebanon, New Hampshire (Ho).
Lee, Rustad, Herrera Santos, and Ho are co-first authors; Stern is the senior author.
Corresponding Author: Jeong Hoo Lee, MD, Department of Psychiatry, Brigham and Women’s Faulkner Hospital, Harvard Medical School, 1153 Centre St, Jamaica Plain, MA 02130 ([email protected]).
Dr Lee is a consultation-liaison psychiatrist at Brigham and Women’s Faulkner Hospital and an instructor and associate clerkship site director for psychiatry at Harvard Medical School.
Relevant Financial Relationships: Dr Rustad is employed by the US Department of Veterans Affairs, but the opinions expressed in this presentation do not reflect those of the Department of Veterans Affairs. Dr Stern has received royalties from Elsevier for editing textbooks on psychiatry. The other authors report no financial relationships related to the subject of this article.
Funding/Support: None.
References (54)

- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–150. PubMed CrossRef
- Gillett G, Davis O, Gill A, et al. Exploring foundation doctors’ self-reported confidence in the assessment and management of mental health conditions. BJPsych Bull. 2024;48(2):139–144. PubMed CrossRef
- Aftab A, Waterman GS. Conceptual competence in psychiatry: recommendations for education and training. Acad Psychiatry. 2021;45(2):203–209. PubMed CrossRef
- Zonoobi M, Tabatabaee M, Amini H. The effects of an educational intervention on reducing stigma among medical students toward patients with psychiatric disorders. BMC Med Educ. 2024;24(1):1216. PubMed CrossRef
- Spencer J. Learning and teaching in the clinical environment. BMJ. 2003;326(7389):591–594. PubMed CrossRef
- Rustad JK, Schlozman SC, Chen J, et al. An alternative proposal for teaching medical students about psychiatry: consultation-Liaison psychiatry rotations that consult to medical and surgical services. Acad Psychiatry. 2024;48(1):81–85. PubMed CrossRef
- Ho PA, Girgis C, Rustad JK, et al. Advancing the mission of Consultation-Liaison Psychiatry through innovation in teaching. Psychosomatics. 2019;60(6):539–548. PubMed CrossRef
- Ong LM, de Haes JC, Hoos AM, et al. Doctor-patient communication: a review of the literature. Soc Sci Med 1982. 1995;40(7):903-918. CrossRef
- Chipidza FE, Wallwork RS, Stern TA. Impact of the doctor-patient relationship. Prim Care Companion CNS Disord. 2015;17(5):15f01840.
- Deveugele M. Communication training: skills and beyond. Patient Educ Couns. 2015;98(10):1287–1291. PubMed CrossRef
- Fuehrer S, Weil A, Osterberg LG, et al. Building authentic connection in the patient-physician relationship. J Prim Care Community Health. 2024;15:21501319231225996. PubMed CrossRef
- Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. 2021;30(1):17–28. PubMed CrossRef
- Trinh NH, Jahan AB, Chen JA. Moving from cultural competence to cultural humility in psychiatric education. Psychiatr Clin North Am. 2021;44(2):149–157. PubMed CrossRef
- Valle Coto MG, Iñiguez RX, Lentskevich MA, et al. Teaching foundational language equity concepts in the pre-clinical curriculum. BMC Med Educ. 2024;24(1):485. PubMed CrossRef
- Finney GR, Minagar A, Heilman KM. Assessment of mental status. Neurol Clin. 2016;34(1):1–16. PubMed CrossRef
- Lenouvel E, Chivu C, Mattson J, et al. Instructional design strategies for teaching the mental status examination and psychiatric interview: a scoping review. Acad Psychiatry. 2022;46(6):750–758. PubMed CrossRef
- Mendez M. Chapter 1 - introduction. In: Mendez M, ed. The Mental Status Examination Handbook. Elsevier; 2022:3–8. CrossRef
- Voss RM, Das JM. Mental status examination. In: StatPearls. StatPearls Publishing; 2025. Accessed February 17, 2025. http://www.ncbi.nlm.nih.gov/books/NBK546682/
- Martin A, Jacobs A, Krause R, et al. The mental status exam: an online teaching exercise using video-based depictions by simulated patients. MedEdPORTAL. 2020;16:10947. PubMed CrossRef
- Norris D, Clark MS, Shipley S. The mental status examination. Am Fam Physician. 2016;94(8):635–641. PubMed
- Trapp NT, Martyna MR, Siddiqi SH, et al. The neuropsychiatric approach to the assessment of patients in neurology. Semin Neurol. 2022;42(2):88–106. PubMed CrossRef
- Jimenez XF, Azzam PN, Gopalan P. Teaching a neuromedical-contextual approach to psychosomatic medicine. Acad Psychiatry. 2015;39(2):204–211. PubMed CrossRef
- Agrawal N, Faruqui R, Bodani M. Oxford Textbook of Neuropsychiatry. 1st ed. OUP Oxford; 2020. Accessed February 17, 2025. http://ezp-prod1.hul.harvard.edu/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=nlebk&AN=2570158&site=ehost-live&scope=site
- Moutier CY. Innovative and timely approaches to suicide prevention in medical education. Acad Psychiatry. 2021;45(3):252–256. PubMed CrossRef
- Hung EK, Binder RL, Fordwood SR, et al. A method for evaluating competency in assessment and management of suicide risk. Acad Psychiatry. 2012;36(1):23–28. PubMed CrossRef
- Brendel RW, Wei MH, Edersheim JG. An approach to the patient in crisis: assessments of the risk of suicide and violence. Med Clin North Am. 2010;94(6):1089–1102. PubMed CrossRef
- Foster A, Alderman M, Safin D, et al. Teaching suicide risk assessment: spotlight on the therapeutic relationship. Acad Psychiatry. 2021;45(3):257–261. PubMed CrossRef
- Warburton KD, Scott CL. Violence risk assessment and treatment. CNS Spectr. 2014;19(5):366–367. PubMed CrossRef
- Hvidhjelm J, Berring LL, Whittington R, et al. Short-term risk assessment in the long term: a scoping review and meta-analysis of the Brøset Violence Checklist. J Psychiatr Ment Health Nurs. 2023;30(4):637–648. PubMed CrossRef
- Wortzel HS, Borges LM, Barnes SM, et al. Therapeutic risk management for violence: clinical risk assessment. J Psychiatr Pract. 2020;26(4):313–319. PubMed CrossRef
- Donovan AL, Vyas CM, Petriceks A, et al. Agitation and an altered mental status in the emergency department: differential diagnosis, evaluation, and treatment. Prim Care Companion CNS Disord. 2022;24(6):22f03277. PubMed CrossRef
- Caplan JP, Beckwith N, McCoy TH, et al. Delirium. In: Stern TA, Wilens TE, Fava M, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 3rd ed. Elsevier Inc; 2025:155–165. CrossRef
- Schlozman SC, Cohen J, Stern TA. Coping With Medical Illness and Psychotherapy of the Medically Ill Patients. In: Stern TA, Wilens TE, Fava M, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 3rd ed. Elsevier Inc; 2025:95–99. CrossRef
- Howe A, Smajdor A, Stöckl A. Towards an understanding of resilience and its relevance to medical training. Med Educ. 2012;46(4):349–356. PubMed CrossRef
- Dornan T. Osler, Flexner, apprenticeship and “the new medical education.” J R Soc Med. 2005;98(3):91–95. PubMed CrossRef
- Kotsis SV, Chung KC. Application of the “see one, do one, teach one” concept in surgical training. Plast Reconstr Surg. 2013;131(5):1194–1201. PubMed CrossRef
- Gorrindo T, Beresin EV. Is “see one, do one, teach one” dead? Implications for the professionalization of medical educators in the twenty-first century. Acad Psychiatry. 2015;39(6):613–614. PubMed CrossRef
- 2025 Psychiatry clerkship guide. Med Sch Insid. 2023. Accessed February 17, 2025. https://medschoolinsiders.com/medical-student/psychiatry-clerkshipguide/
- Vemuri M, Dunn LB. Ethical and clinical issues in integrated care settings: patient privacy concerns and electronic health records. Focus (Madison). 2017;15(3):301–305. PubMed CrossRef
- Meyer F, Abbasi O, Kasick D, et al. Medical student experiences on Consultation Liaison psychiatry rotations: a nationwide survey. Psychosomatics. 2018;59(1):75–80. PubMed CrossRef
- Saunders J, Gopalan P, Puri N, et al. Psychosomatic medicine for non-psychiatric residents: video education and incorporation of technology. Acad Psychiatry. 2015;39(6):649–653. PubMed CrossRef
- Morreale MK, Balon R, Coverdale J, et al. Educating other physicians in the provision of psychiatric care. Acad Psychiatry. 2023;47(1):7–9. PubMed CrossRef
- Cooper S, Dogra N, Lunn B, et al. Undergraduate psychiatry teaching – the core curriculum. In: Teaching Psychiatry to Undergraduates. The Royal College of Psychiatrists; 2011:26–37.
- Lokko HN, Gatchel JR, Becker MA, et al. The art and science of learning, teaching, and delivering feedback in psychosomatic medicine. Psychosomatics. 2016;57(1):31–40. PubMed CrossRef
- Wei MH, Querques J, Stern TA. Teaching trainees about the practice of consultation-liaison psychiatry in the general hospital. Psychiatr Clin North Am. 2011;34(3):689–707. PubMed CrossRef
- Knowles M. The Adult Learner: A Neglected Species. Gulf Publishing Company; 1973. Accessed February 17, 2025. https://eric.ed.gov/?id=ED084368
- Kontos N, Freudenreich O, Querques J, et al. The consultation psychiatrist as effective physician. Gen Hosp Psychiatry. 2003;25(1):20–23. PubMed CrossRef
- Kontos N, Freudenreich O, Querques J. Ownership, responsibility and hospital care: lessons for the consultation psychiatrist. Gen Hosp Psychiatry. 2008;30(3):257–262. PubMed CrossRef
- French H, Arias-Shah A, Gisondo C, et al. Perspectives: the flipped classroom in graduate medical education. NeoReviews. 2020;21(3):e150–e156. PubMed CrossRef
- Phillips J, Wiesbauer F. The flipped classroom in medical education: a new standard in teaching. Trends Anaesth Crit Care. 2022;42:4–8. PubMed CrossRef
- İçöz D, Çetin B, Özdemir O. Comparative analysis of layered curriculum and project-based learning approaches in an oral radiological course. J Dent Educ. 2024. Published online. doi:10.1002/jdd.13775. CrossRef
- Ho PA, Girgis C, Rustad JK, et al. Advancing medical education through innovations in teaching during the COVID-19 pandemic. Prim Care Companion CNS Disord. 2021;23(1):20nr02847. PubMed CrossRef
- Lee GB, Chiu AM. Assessment and feedback methods in competency-based medical education. Ann Allergy Asthma Immunol. 2022;128(3):256–262. PubMed CrossRef
- Tabish S. Assessment methods in medical education. Int J Health Sci. 2008;2(2):3–7.
Enjoy this premium PDF as part of your membership benefits!