Lithium remains a first-line treatment for bipolar disorder due to its proven ability to stabilize mood and address both manic and depressive episodes.1 However, maintaining therapeutic lithium levels is essential, as fluctuations can lead to reduced efficacy, increased side effects, or toxicity.2 Various factors—such as dietary habits, hydration status, medication interactions, and unreported supplement or steroid use—can significantly impact lithium levels.3 Notably, exogenous testosterone has been linked to the precipitation of mania in individuals with bipolar disorder.4 This case highlights the importance of assessing dietary habits, supplement use, and potential anabolic steroid use, particularly in physically active patients undergoing lithium therapy.
Case Report
A 59-year-old man with a history of bipolar I disorder presented to the emergency department multiple times each month over the course of several months for gastrointestinal complaints, primarily diarrhea and dehydration requiring intravenous fluids. Each admission lasted 1 to 2 days before he was discharged with symptomatic treatment. The patient’s medications included lithium 900 mg nightly for mood stabilization, fluoxetine 60 mg daily for depression, diazepam 10 mg for anxiety/sleep, and trazodone 50 mg as needed for sleep. His lithium levels were consistently subtherapeutic, and he continued to experience mood instability despite reported medication adherence. As a result, his lithium dose was increased to 600 mg twice daily with the aim of more consistent symptom management.
The patient was a personal trainer and bodybuilder who personally emphasized physical fitness in his daily life. He took naproxen 200 mg 4 times a day for knee arthritis pain and Tylenol 1,000 mg twice a day for the same reason so that he could maintain his weightlifting regimen. The patient consistently denied the use of testosterone or any form of hormone replacement therapy.
His psychiatric team reevaluated his ongoing mood instability symptoms and recurrent gastrointestinal complaints, considering alternative explanations for his fluctuating lithium levels. During a psychiatric visit in August 2023, the patient endorsed depressive symptoms (Patient Health Questionnaire-9 [PHQ-9]5 score: 16), including sadness, hopelessness, low energy, poor concentration, trouble falling asleep, and irritability. While he noted improvement in sadness and concentration, he also reported experiencing distractibility and racing thoughts, though without rapid or pressured speech. At a follow-up visit in November 2023, he continued to exhibit signs of depression (PHQ-9 score: 18) in addition to reporting mania symptoms, including persistent distractibility and racing thoughts.
During another psychiatric visit, the patient disclosed that he had been regularly consuming Himalayan salt mixed with up to 1.5 gallons of water daily as part of his health and fitness regimen. Given the known impact of excessive sodium and water intake on lithium excretion, this revelation provided a potential explanation for his consistently low lithium levels.6 Despite initially denying it, the patient later admitted to self-administering an off-market testosterone preparation after further discussion with the psychiatric team. Considering the known potential of testosterone to induce mania symptoms in individuals with bipolar disorder, this was identified as a likely contributing factor to his ongoing mood instability.7
Due to the risk of kidney dysfunction associated with fluctuating lithium levels, his psychiatric team decided to discontinue lithium therapy and transition him to quetiapine XR 400 mg nightly to control his bipolar symptoms. However, the patient wanted to minimize his medication use and has yet to start quetiapine or any other mood stabilizer. Despite the team’s counsel, he remained hesitant about the importance of stabilization for his bipolar I diagnosis.
Discussion
Lithium is widely recognized as an effective treatment for bipolar disorder, primarily due to its ability to stabilize mood and reduce the frequency of both manic and depressive episodes.8 It is typically prescribed at doses that achieve a therapeutic blood level between 0.8 and 1.2 mEq/L, requiring regular monitoring to prevent toxicity or inefficacy.9 However, several factors can influence lithium levels, including hydration status, dietary sodium intake, medication interactions, and renal function.10
In our case, the patient’s use of Himalayan salt likely contributed to his persistently low lithium levels. Sodium intake has a well-documented inverse relationship with lithium retention, as increased sodium consumption can enhance renal lithium excretion, leading to subtherapeutic levels.11 Conversely, dehydration can increase lithium levels by reducing renal clearance, which is particularly concerning given the patient’s recurrent episodes of diarrhea. Nonsteroidal anti-inflammatory drugs like the ones used daily by our patient, diuretics, and angiotensin-converting enzyme inhibitors are also known to elevate lithium levels by altering renal excretion.12
Fluctuating lithium levels pose significant risks, including decreased treatment efficacy, increased side effects, and long-term renal dysfunction.13 Chronic lithium use has been associated with nephrotoxicity, particularly in patients with a history of significant level variability.14 This was a key consideration in the decision to discontinue lithium therapy for this patient.
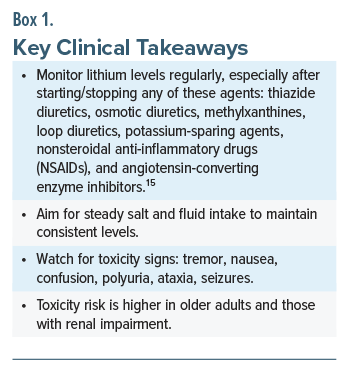
Another critical aspect of our case is the patient’s undisclosed testosterone use. Exogenous testosterone, especially in those with bipolar disorder, has been associated with the precipitation of manic symptoms.4 Given the patient’s bodybuilding background and subsequent admission of anabolic steroid use, this was likely a contributing factor to his ongoing mood instability. Box 1 provides key clinical takeaways from this case.
Conclusion
This case underscores the importance of thoroughly evaluating dietary habits, supplement use, and potential anabolic steroid use in patients with bipolar disorder who present with unstable lithium levels. Health care providers should maintain a high index of suspicion when encountering patients engaged in intense physical fitness regimens, as factors such as sodium intake, hydration status, and hormone supplementation can significantly impact treatment efficacy. A comprehensive approach that includes dietary assessment, medication reconciliation, and open discussions about supplement and steroid use is essential for optimizing mood stabilization and minimizing adverse outcomes.
Article Information
Published Online: December 11, 2025. https://doi.org/10.4088/PCC.25cr04028
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(6):25cr04028
Submitted: June 16, 2025; accepted August 26, 2025.
To Cite: McDuffee NS, Forster AA, Shah K. Unstable lithium levels in a bodybuilder with bipolar disorder: the impact of sodium intake and anabolic steroid use. Prim Care Companion CNS Disord 2025;27(6):25cr04028.
Author Affiliations: Wake Forest School of Medicine, Winston-Salem, North Carolina (McDuffee, Forster); Atrium Health Wake Forest Baptist, Winston-Salem, North Carolina (Shah).
Corresponding Author: Nicholas S. McDuffee, MA, BS, Atrium Health Wake Forest Baptist, Department of Psychiatry, Wake Forest School of Medicine, 1 Medical Center Blvd, Winston-Salem, North Carolina 27157 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was received from the patient to publish the case report, and information, including dates, has been de-identified to protect anonymity.
References (15)

- Malhi GS, Gessler D, Outhred T. The use of lithium for the treatment of bipolar disorder: recommendations from clinical practice guidelines. J Affect Disord. 2017;217:266–280. PubMed CrossRef
- Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach: part III: clinical safety. CNS Drugs. 2009;23(5):397–418. PubMed CrossRef
- McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379(9817):721–728. PubMed CrossRef
- Pope HG Jr, Katz DL. Psychiatric and medical effects of anabolic-androgenic steroid use. A controlled study of 160 athletes. Arch Gen Psychiatry. 1994;51(5):375–382. PubMed CrossRef
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. PubMed CrossRef
- Gitlin M. Lithium side effects and toxicity: prevalence and management strategies. Int J Bipolar Disord. 2016;4(1):27. PubMed CrossRef
- Elboga G, Sayiner ZA. Rare cause of manic period trigger in bipolar mood disorder: testosterone replacement. BMJ Case Rep. 2018;2018:bcr2018225108. PubMed CrossRef
- Goodwin GM, Haddad PM, Ferrier IN, et al. Evidence-based guidelines for treating bipolar disorder: revised third edition recommendations from the British Association for Psychopharmacology.J Psychopharmacol. 2016;30(6):495–553. PubMed CrossRef
- Kamal ZM, Dutta S, Rahman S, et al. Therapeutic application of lithium in bipolar disorders: a brief review. Cureus. 2022;14(9):e29332. PubMed CrossRef
- Bocchetta A, Ardau R, Fanni T, et al. Renal function during long-term lithium treatment: a cross-sectional and longitudinal study. BMC Med. 2015;13:12. PubMed CrossRef
- Shine B, McKnight RF, Leaver L, et al. Long-term effects of lithium on renal, thyroid, and parathyroid function: a retrospective analysis of laboratory data. Lancet. 2015;386(9992):461–468. PubMed CrossRef
- Rej S, Herrmann N, Shulman K. The effects of lithium on renal function in older adults-a systematic review. J Geriatr Psychiatry Neurol. 2012;25(1):51–61. PubMed CrossRef
- Machado-Vieira R, Manji HK, Zarate CA Jr. The role of lithium in the treatment of bipolar disorder: convergent evidence for neurotrophic effects as a unifying hypothesis. Bipolar Disord. 2009;11(Suppl 2):92–109. PubMed CrossRef
- Bendz H, Sjödin I, Aurell M. Renal function on and off lithium in patients treated with lithium for 15 years or more. A controlled, prospective lithium-withdrawal study. Nephrol Dial Transpl. 1996;11(3):457–460. PubMed
- LITHOBID (lithium carbonate) tablet, film coated, extended release. DailyMed, National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f7f5b69a-c2a1-4586-a189-1475d41387c0. Accessed June 18, 2025.
Enjoy this premium PDF as part of your membership benefits!