Posterior reversible encephalopathy syndrome (PRES) is an acute clinical condition, often manifesting as a spectrum of findings including headache, encephalopathy, visual disturbances, and seizures. The disorder is believed to result from failure of cerebral autoregulation and endothelial dysfunction, resulting in vasogenic cerebral edema.1 As the name implies, the condition mostly involves the occipital and parietal regions. While infratentorial involvement can occur,2 PRES resulting in acute obstructive hydrocephalus is an exceedingly rare finding. Here, we present a case of PRES due to substance-induced hypertensive crisis resulting in obstructive hydrocephalus.
Case Report
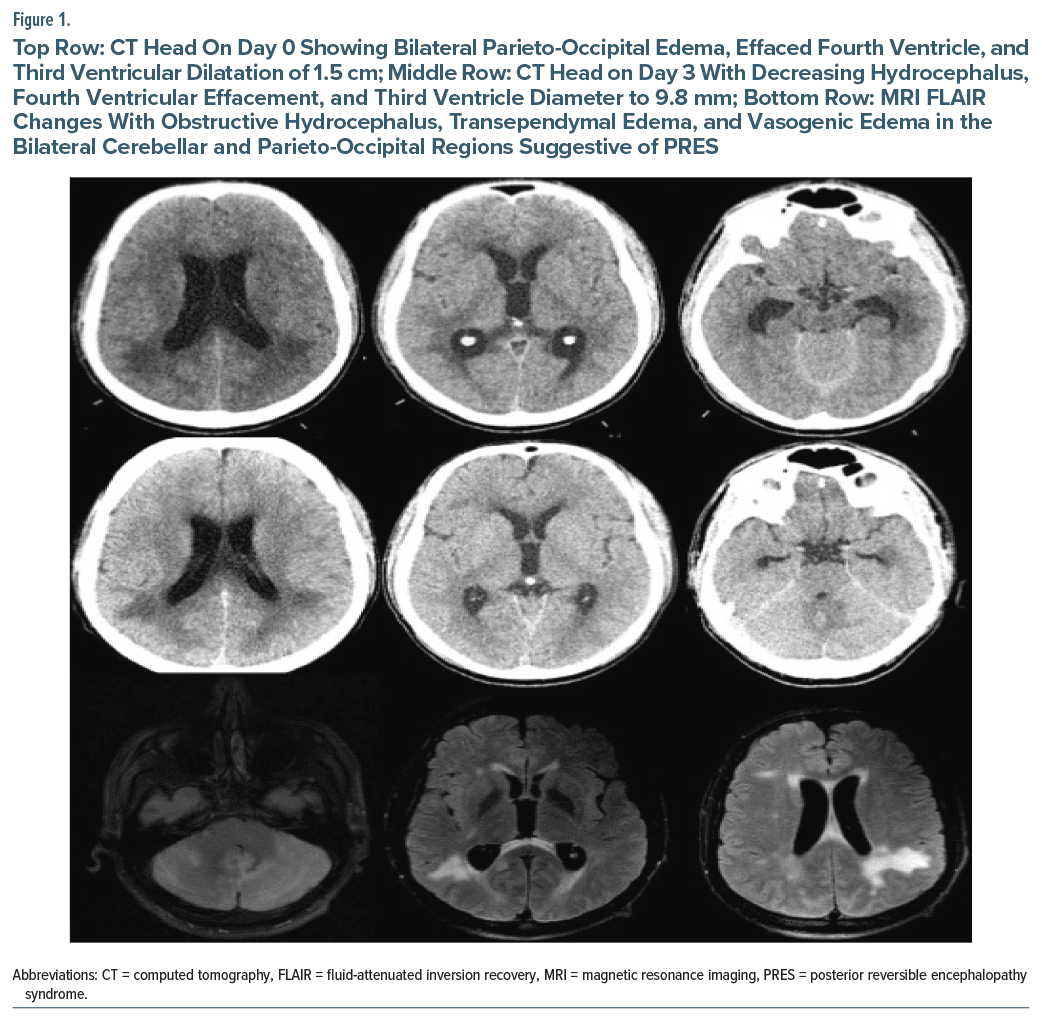
A 28-year-old white man with a history of severe hypertension, hyperthyroidism, and cocaine and methamphetamine use presented to the emergency department (ED) with severe headache, nausea, dizziness, and bright spots in his left eye for 1 day. The patient reported using methamphetamine at the time of symptom onset. At that time, he measured his blood pressure and noted his systolic blood pressure was 279 mm Hg. Upon arrival to the ED, his initial blood pressure was noted to be 222/159 mm Hg. His neurological examination was noted to be unremarkable. A computed tomography (CT) scan showed diffuse edema in the cerebellum and brain stem resulting in significant mass effect on the fourth ventricle and obstructive hydrocephalus (Figure 1). The patient was transferred to our facility with a suspicion of an infratentorial mass. Upon arrival, he was admitted to the neurocritical unit for further management. Magnetic resonance imaging with and without contrast showed vasogenic edema, most pronounced in the bilateral cerebellar hemispheres but also present in the supratentorial compartment. Periventricular transependymal edema was also noted. There was no evidence of any space-occupying lesion. His magnetic resonance angiogram was unremarkable. Based on a careful review of history and imaging studies, a diagnosis of PRES was established.
He was managed with gradual downtitration of his blood pressure. Neurosurgical interventions such as placement of an external ventricular drain were initially considered but withheld given improving symptoms and the reversible nature of PRES. There was a gradual resolution of his symptoms over the course of hospitalization. A repeat head CT at 72 hours showed significantly improving vasogenic edema and decreased hydrocephalus (Figure 1). The patient was discharged on the fourth day of hospitalization.
Discussion
The clinical presentation of PRES is highly variable, ranging from mild disorientation, headache, vomiting, and blurry vision3,4 to cortical blindness, seizures, depressed consciousness5,6 coma, and death.7 Infratentorial involvement causing obstructive hydrocephalus is rare and may be misdiagnosed as an infiltrative tumor, infarction, or encephalitis, which could result in delayed treatment or unnecessary surgical interventions such as biopsy.8 In cases with progressive neurological deterioration, hydrocephalus may require CSF diversion with emergency external ventricular drain placement or endoscopic third ventriculostomy.6,8 Prompt recognition of PRES and its management can help in avoiding these interventions and possible complications.
The exact pathogenesis of PRES is still unknown. The 2 commonly reported mechanisms involve impaired cerebral autoregulation and endothelial dysfunction.3 Under normal circumstances, cerebral vasculature can maintain cerebral blood flow through changes in arteriolar diameter. However, in patients with extreme blood pressure elevation, these mechanisms fail and can result in extravasation across the blood-brain barrier. Such extravasation of fluid can also be seen with other causes of endothelial dysfunction such as autoimmune conditions or exposure to chemotherapeutic or immunosuppressive drugs.4
Our case highlights the association of acute elevation in blood pressure and use of vasoactive drugs such as methamphetamine resulting in PRES and a rare presentation with obstructive hydrocephalus. Effective management of PRES focuses on early detection of symptoms with aggressive blood pressure control, which can prevent invasive procedures and its associated complications.
Article Information
Published Online: May 29, 2025. https://doi.org/10.4088/PCC.24cr03907
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(3):24cr03907
Submitted: December 18, 2024; accepted February 14, 2025.
To Cite: Morakinyo O, Jacob SM, Waqar SZB, et al. Posterior reversible encephalopathy syndrome presenting with obstructive hydrocephalus: a rare presentation. Prim Care Companion CNS Disord 2025;27(3):24cr03907.
Author Affiliations: Department of Neurology, University of Texas Medical Branch, Galveston, Texas (Morakinyo, Jacob, Hafeez); Aga Khan University, Karachi, Pakistan (Waqar).
Corresponding Author: Oreoluwa Morakinyo, MD, Department of Neurology, University of Texas Medical Branch, Galveston, TX 77555-0539 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was obtained to publish the case report, and information has been de-identified to protect patient anonymity.
References (8)

- Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015;14(9):914–925. PubMed CrossRef
- Grossbach AJ, Abel TJ, Hodis B, et al. Hypertensive posterior reversible encephalopathy syndrome causing posterior fossa edema and hydrocephalus. J Clin Neurosci. 2014;21(2):207–211. PubMed CrossRef
- Sudulagunta SR, Sodalagunta MB, Kumbhat M, et al. Posterior reversible encephalopathy syndrome (PRES). Oxf Med Case Rep. 2017;2017(4):omx011. PubMed CrossRef
- Ansari B, Saadatnia M. Prevalence and risk factors of posterior reversible encephalopathy syndrome in Isfahan, Iran. Adv Biomed Res. 2021;10(1):53. PubMed CrossRef
- Hiesgen J, Annor TN. Acute obstructive hydrocephalus in posterior reversible encephalopathy syndrome. South Afr Med J. 2022;113(1):9–12. PubMed CrossRef
- Lee SY, Dinesh SK, Thomas J. Hypertension-induced reversible posterior leukoencephalopathy syndrome causing obstructive hydrocephalus. J Clin Neurosci. 2008;15(4):457–459. PubMed CrossRef
- Geocadin RG. Posterior reversible encephalopathy syndrome. N Engl J Med. 2023;388(23):2171–2178. PubMed CrossRef
- Wirojtananugoon C, Laothamatas J. Posterior reversible encephalopathy syndrome with obstructive hydrocephalus. A case report. Neuroradiol J. 2011;24(2):258–263. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!